Nursing diagnosis is a cornerstone of modern healthcare, acting as the critical second step in the nursing process. For both seasoned nurses and those just starting their journey in healthcare, a firm grasp of nursing diagnosis is essential. It’s more than just medical terminology; it’s the foundation upon which personalized and effective patient care plans are built. This detailed guide will explore the concept of nursing diagnosis, its vital purposes, and most importantly, break down the 3 key parts of the nursing diagnosis, providing you with a deeper understanding and practical skills to enhance your nursing practice.
What is a Nursing Diagnosis?
At its core, a nursing diagnosis is a clinical judgment made by a registered nurse. This judgment concerns a patient’s response to actual or potential health conditions or life processes. It’s about understanding how an individual, family, group, or community is affected by health issues or vulnerabilities. This definition, endorsed by nursing organizations and educational bodies, highlights the unique role of nurses in patient care.
Nursing diagnoses are not just labels; they are the result of a thorough nursing assessment. During this assessment, nurses gather crucial data about a patient’s physical, psychological, social, and spiritual health. This data then becomes the basis for formulating a nursing diagnosis, which, in turn, directs the selection of appropriate nursing interventions. These interventions are designed to achieve specific patient outcomes for which nurses are accountable. Effectively, the nursing diagnosis bridges the gap between assessment and the creation of a tailored nursing care plan.
Purposes of Nursing Diagnosis in Healthcare
Why is nursing diagnosis so important? Its purposes are multifaceted, contributing significantly to both the quality of patient care and the professional development of nurses.
- Enhancing Critical Thinking Skills: For nursing students, learning to formulate nursing diagnoses is an invaluable exercise in problem-solving and critical thinking. It encourages a systematic approach to patient care, moving beyond rote memorization to analytical application of knowledge.
- Prioritizing Nursing Care: Nursing diagnoses are instrumental in identifying nursing priorities. By clearly defining patient problems, nurses can effectively direct nursing interventions to address the most pressing needs first, ensuring timely and efficient care.
- Formulating Expected Outcomes: For healthcare institutions and third-party payers, nursing diagnoses play a role in quality assurance. They provide a framework for setting measurable expected outcomes, which are essential for evaluating the effectiveness of nursing care and meeting quality standards.
- Understanding Patient Responses: Nursing diagnoses shift the focus to the patient’s response to health issues, rather than just the medical condition itself. This holistic approach helps nurses understand how clients respond to actual or potential health problems, considering their strengths and resources to prevent or resolve these issues.
- Facilitating Communication: In the complex world of healthcare, clear communication is paramount. Nursing diagnoses provide a common language for nurses and the wider healthcare team. This shared understanding promotes effective communication and collaboration, leading to better coordinated patient care.
- Evaluating Nursing Care Effectiveness: Finally, nursing diagnoses are crucial for evaluation. By establishing clear diagnoses and expected outcomes, nurses can determine whether the nursing care provided was beneficial to the client and cost-effective, contributing to evidence-based practice and continuous improvement in healthcare delivery.
Nursing Diagnosis vs. Medical Diagnosis vs. Collaborative Problems
It’s crucial to distinguish nursing diagnoses from medical diagnoses and collaborative problems. While all three are integral to patient care, they represent different perspectives and responsibilities.
A medical diagnosis, made by a physician or advanced practitioner, identifies a disease, medical condition, or pathology that only a medical practitioner can treat. Medical diagnoses focus on the illness itself and aim to identify the underlying cause, which then dictates medical treatment like medication. Examples include Diabetes Mellitus, Tuberculosis, or Hepatitis. Medical diagnoses typically remain constant throughout treatment. Nurses are responsible for following medical orders and implementing prescribed treatments.
On the other hand, a nursing diagnosis focuses on the patient’s response to their medical condition. It addresses the physical, psychological, and spiritual responses to illness or vulnerability. For example, a patient with a medical diagnosis of pneumonia might have nursing diagnoses of Ineffective Airway Clearance or Fatigue. Nursing diagnoses guide nurses in developing care plans that address these patient-specific responses.
Collaborative problems are potential or actual health complications that nurses monitor and manage in collaboration with the medical team. These problems require both physician-prescribed and nurse-initiated interventions. For instance, a patient at risk for complications from surgery presents a collaborative problem. The nursing aspect focuses on monitoring for early signs of complications and implementing preventive measures, while medical interventions may be required to treat the complication if it arises.
In essence, medical diagnoses name the disease, while nursing diagnoses describe the patient’s response to that disease and other health-related situations. Collaborative problems bridge both, requiring interdependent actions from the healthcare team.
The 3 Parts of a Nursing Diagnosis: Diving Deeper
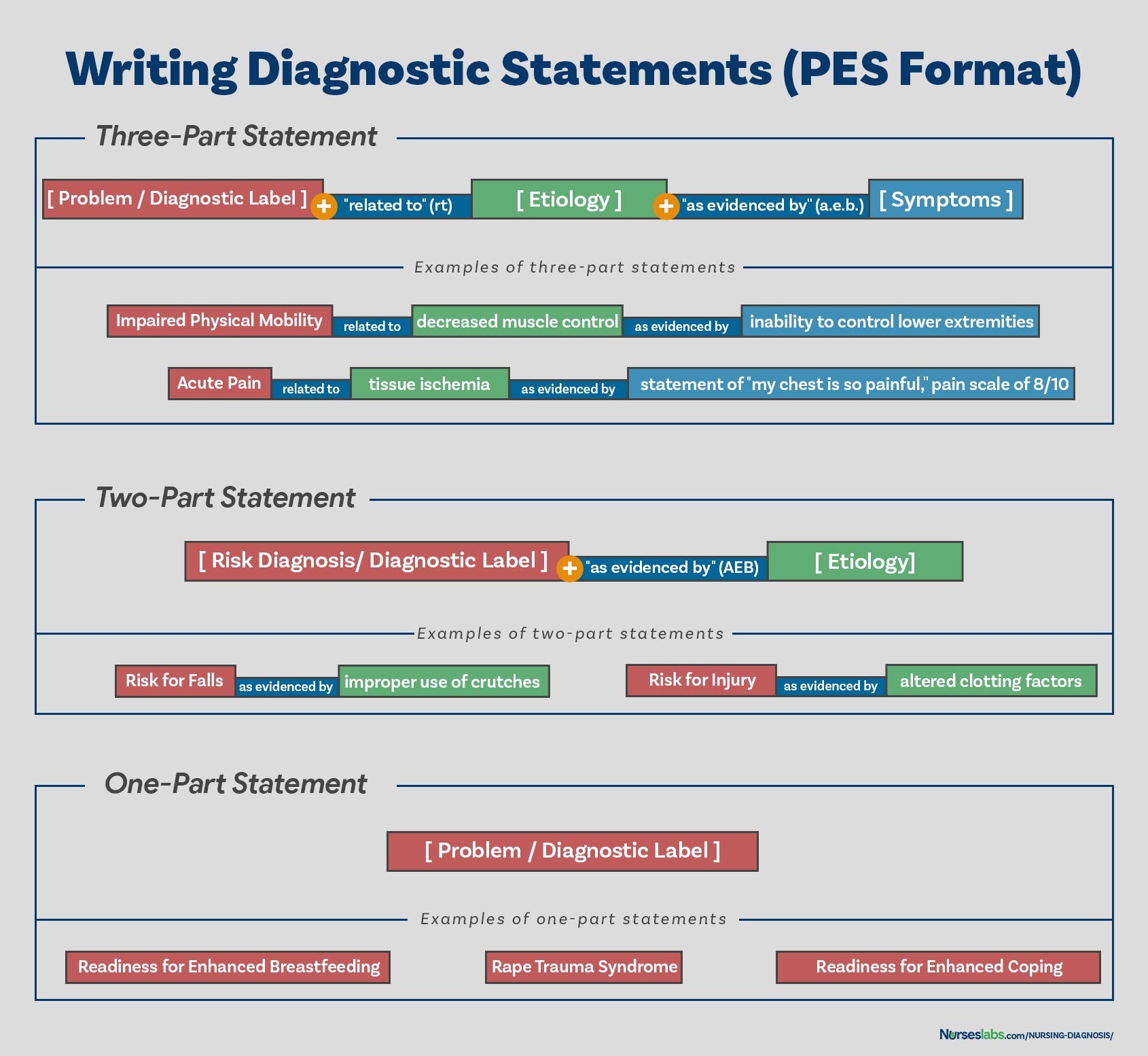
Now, let’s delve into the core of our discussion: the 3 parts of a nursing diagnosis. Understanding these components is essential for formulating accurate and effective diagnoses that drive patient care. Traditionally, a nursing diagnosis is structured into three parts, especially for problem-focused or actual diagnoses. These are often referred to as the PES format:
- Problem (Diagnostic Label): This is a concise statement of the patient’s health problem or response. It is a standardized term or phrase that represents a pattern of related cues.
- Etiology (Related Factors): This identifies the probable cause(s) or contributing factors to the health problem. It’s not a medical diagnosis, but rather conditions or circumstances that influence or cause the patient’s response.
- Signs and Symptoms (Defining Characteristics): These are the clinical manifestations, or evidence, that the problem exists. For actual diagnoses, these are observable and measurable signs and symptoms.
Let’s examine each part in detail.
Part 1: The Problem (Diagnostic Label)
The first part, the problem, is also known as the diagnostic label. This component provides a standardized name for the patient’s health issue. It’s a concise term that represents a cluster of related patient needs or responses. Using standardized labels ensures clear communication among healthcare professionals.
Diagnostic labels often consist of two parts themselves:
- Qualifier: This word adds specific meaning to the diagnosis, refining the label. Qualifiers describe the extent or nature of the problem.
- Focus of the Diagnosis: This is the area of patient functioning that is affected. It pinpoints the specific health domain involved.
| Qualifier | Focus of the Diagnosis | Example Nursing Diagnosis |
|---|---|---|
| Deficient | Fluid Volume | Deficient Fluid Volume |
| Imbalanced | Nutrition: Less Than Body Requirements | Imbalanced Nutrition: Less Than Body Requirements |
| Impaired | Gas Exchange | Impaired Gas Exchange |
| Ineffective | Tissue Perfusion | Ineffective Peripheral Tissue Perfusion |
| Risk for | Injury | Risk for Injury |
It’s important to note that some nursing diagnoses are single-word terms, such as Anxiety, Constipation, Pain, or Nausea. In these cases, the qualifier and focus are inherent within the term itself.
Part 2: Etiology (Related Factors)
The etiology, or related factors, is the second essential part of a nursing diagnosis. This component identifies what is causing or contributing to the patient’s problem. It is crucial to understand that etiology in nursing diagnosis is not the same as the etiology of a medical disease. Instead, it focuses on the factors that nurses can address or influence through nursing interventions.
Identifying related factors is vital for several reasons:
- Directing Nursing Interventions: Etiology guides the selection of appropriate nursing interventions. Interventions should be aimed at modifying or removing the etiological factors, thereby resolving or alleviating the nursing diagnosis.
- Individualizing Patient Care: Understanding the specific related factors for a patient allows nurses to tailor care plans to address the root causes of the problem, rather than just managing symptoms.
- Enhancing Problem Solving: Identifying etiology requires critical thinking and analysis of assessment data. It pushes nurses to think beyond the surface symptoms and consider the underlying reasons for the patient’s health issue.
Etiology is connected to the problem statement using the phrase “related to“. For example:
- Impaired Physical Mobility related to pain and stiffness in joints.
- Deficient Knowledge (regarding medication regimen) related to lack of prior exposure to information.
- Anxiety related to uncertainty about upcoming surgery.
It’s crucial to identify etiologies that are nursing-focused, meaning they are conditions or factors that nurses can independently or collaboratively treat. Medical diagnoses are not used as etiologies, as nurses do not treat medical diseases directly.
Part 3: Signs and Symptoms (Defining Characteristics)
The third part of a nursing diagnosis is the defining characteristics, also known as signs and symptoms. These are the observable and measurable cues that cluster together as evidence of the nursing diagnosis. They are the clinical manifestations that confirm the presence of the problem. Defining characteristics must be present for an actual or problem-focused nursing diagnosis.
Defining characteristics serve to:
- Validate the Diagnosis: They provide the objective and subjective data that support the nursing diagnosis.
- Distinguish Between Diagnoses: Different nursing diagnoses have different sets of defining characteristics. Identifying these helps in accurately differentiating between similar diagnoses.
- Evaluate Patient Progress: As nursing interventions are implemented, the presence and severity of defining characteristics are reassessed to evaluate the effectiveness of care.
Defining characteristics are linked to the problem and etiology using the phrase “as evidenced by” or “as manifested by“. For example, continuing with our previous examples:
- Impaired Physical Mobility related to pain and stiffness in joints as evidenced by limited range of motion in knees and hips, and verbal report of difficulty walking.
- Deficient Knowledge (regarding medication regimen) related to lack of prior exposure to information as evidenced by verbalization of misunderstanding of medication purpose and schedule, and incorrect self-administration of medication.
- Anxiety related to uncertainty about upcoming surgery as evidenced by restlessness, increased heart rate, and verbalization of worry about surgical outcome.
Types of Nursing Diagnoses and the 3 Parts
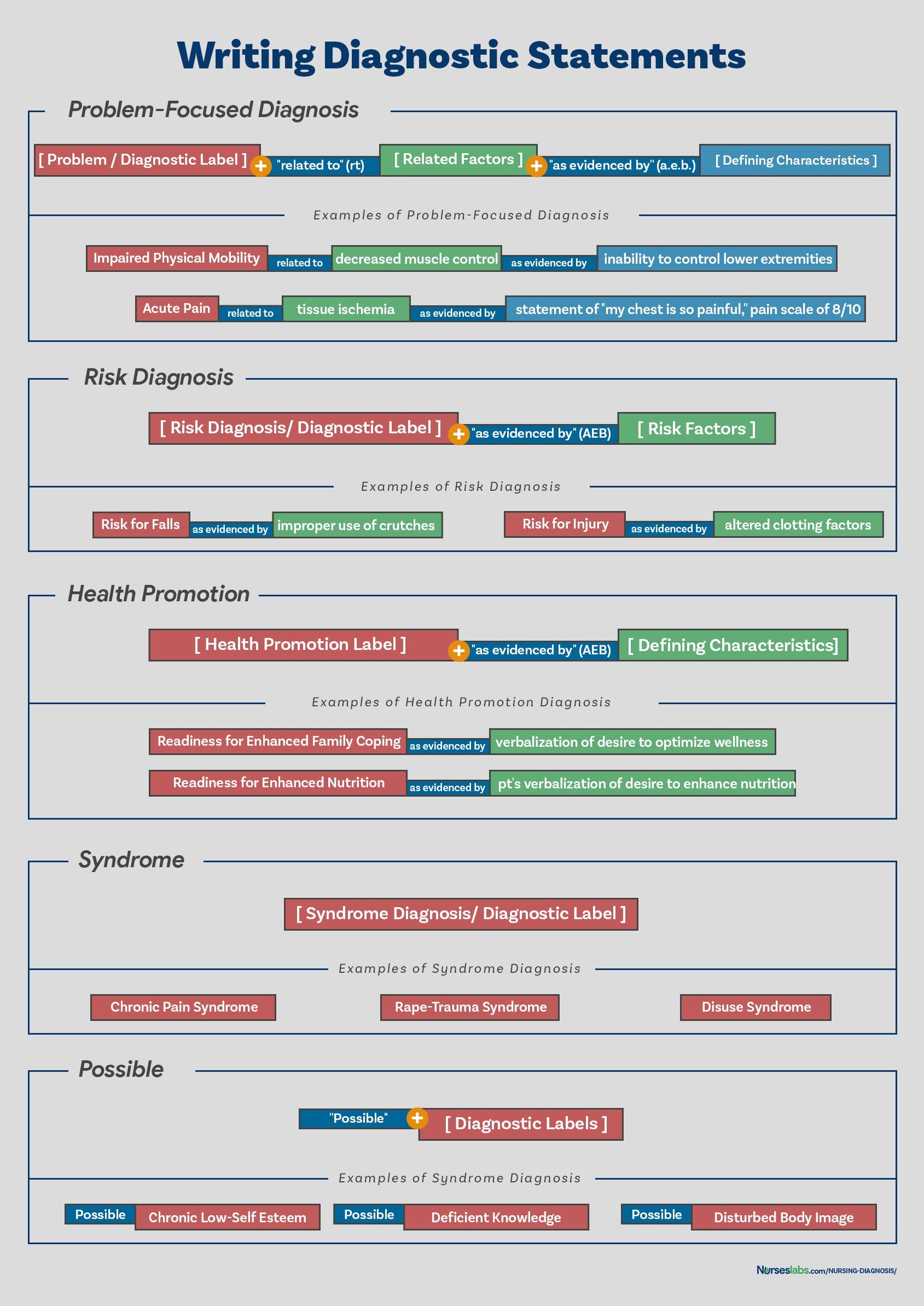
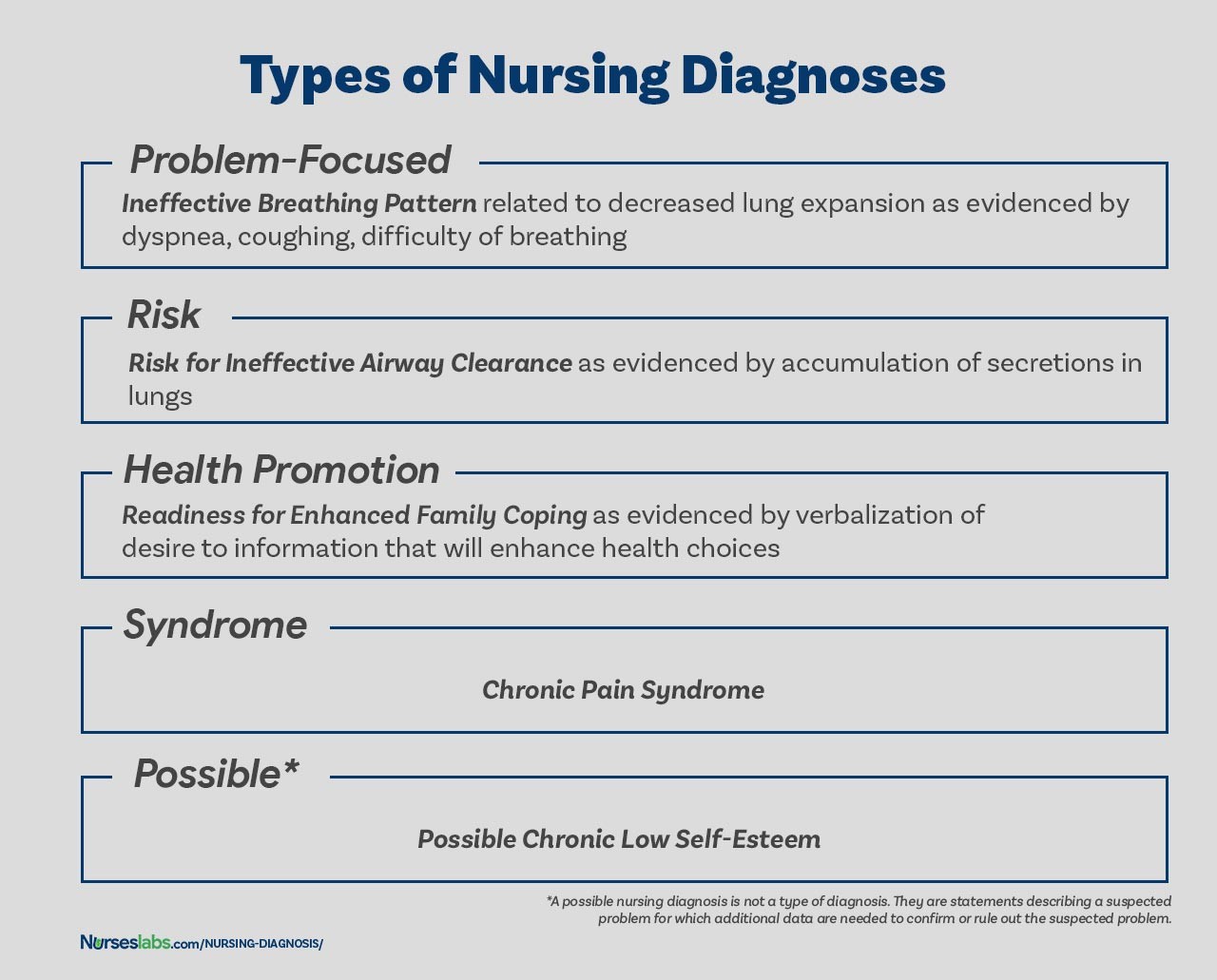
While the three-part PES format is primarily used for problem-focused (actual) nursing diagnoses, it’s important to understand how these parts apply to other types of nursing diagnoses.
-
Risk Nursing Diagnoses: These diagnoses describe potential problems. They have two parts: the diagnostic label and risk factors. Risk factors are the circumstances or conditions that increase the patient’s vulnerability to a problem. Since the problem hasn’t occurred yet, there are no defining characteristics. Risk diagnoses are written as: Risk for [Nursing Diagnosis] as evidenced by [Risk Factors]. For example: Risk for Infection as evidenced by surgical incision and compromised immune system.
-
Health Promotion Nursing Diagnoses: These focus on the patient’s readiness to enhance well-being. They are typically one-part statements: Readiness for Enhanced [Specific Health Behavior]. For example: Readiness for Enhanced Nutrition. Related factors may be added for clarity but are not mandatory. Defining characteristics aren’t applicable as these diagnoses are about potential for improvement, not existing problems.
-
Syndrome Diagnoses: These are diagnoses that represent a cluster of nursing diagnoses that occur together. They are also one-part statements, using only the diagnostic label, for example: Rape Trauma Syndrome. Defining characteristics and related factors are inherent in the syndrome diagnosis itself.
-
Possible Nursing Diagnoses: These describe suspected problems requiring more data to confirm or rule out. They are not formally recognized as a distinct type but represent a stage in the diagnostic process. They also do not strictly adhere to the 3-part structure until confirmed as actual or risk diagnoses.
Formulating Nursing Diagnoses: The Diagnostic Process
Formulating accurate nursing diagnoses involves a systematic process:
- Data Analysis: This involves reviewing the patient assessment data, comparing it to norms, identifying patterns, and recognizing any gaps or inconsistencies.
- Problem Identification: Based on data analysis, identify potential health problems, risks, and strengths. Differentiate between nursing diagnoses, medical diagnoses, and collaborative problems.
- Diagnostic Statement Formulation: Construct clear and concise diagnostic statements using the appropriate format (PES for actual diagnoses, two-part for risk diagnoses, one-part for health promotion and syndrome diagnoses).
Writing Effective Nursing Diagnosis Statements
To write clear and effective nursing diagnoses:
- Be Specific and Concise: Use precise language and avoid jargon.
- Be Patient-Centered: Focus on the patient’s responses, not just the medical condition.
- Be Nursing-Focused: Address problems that nurses can treat within their scope of practice.
- Use Standardized Language: Employ NANDA-I (or other recognized classification systems) approved diagnostic labels.
- Ensure Logical Links: Make sure the etiology logically relates to the problem, and the defining characteristics support the diagnosis.
Nursing Diagnosis: The Bedrock of Nursing Care Plans
Nursing diagnoses are not just academic exercises; they are the crucial link to developing effective nursing care plans. Each nursing diagnosis becomes the basis for setting patient goals, planning nursing interventions, and evaluating outcomes. A well-formulated nursing diagnosis ensures that the care plan is focused, individualized, and directly addresses the patient’s specific needs.
Conclusion: Mastering the 3 Parts for Enhanced Patient Care
Understanding the 3 parts of a nursing diagnosis – the Problem (Diagnostic Label), Etiology (Related Factors), and Signs and Symptoms (Defining Characteristics) – is fundamental to nursing practice. These components provide a structured approach to identifying patient problems, understanding their causes, and recognizing their manifestations. By mastering these elements, nurses can formulate accurate and comprehensive nursing diagnoses that serve as the cornerstone of effective, patient-centered care. This detailed understanding not only improves patient outcomes but also enhances professional communication and critical thinking within the healthcare team.
Recommended Resources
To further enhance your understanding and skills in nursing diagnosis, consider these resources:
- Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care
- Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition)
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care
- All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health
References and Sources
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.