Acute abdominal pain is a frequently encountered complaint in pediatrics, presenting a considerable diagnostic challenge due to the broad spectrum of potential underlying causes, ranging from benign to life-threatening conditions. While many cases of acute abdominal pain in children are self-limiting and benign, such as those associated with gastroenteritis, constipation, or viral infections, it is crucial for clinicians to promptly identify children with serious surgical or medical etiologies requiring urgent intervention. This article aims to provide an in-depth review of pediatric abdominal pain, emphasizing the differential diagnosis, clinical evaluation, and appropriate management strategies for healthcare professionals.
PATHOGENESIS OF ABDOMINAL PAIN IN CHILDREN
Understanding the pathophysiology of abdominal pain is crucial for accurate diagnosis. Abdominal pain can be broadly categorized into three types based on the pain receptors involved: visceral, somatoparietal, and referred pain. Notably, the majority of abdominal pain originates from visceral pain receptors.
Visceral pain receptors are distributed across the serosal surfaces, mesentery, intestinal muscles, and mucosa of hollow organs. These receptors are primarily responsive to mechanical and chemical stimuli, including distension, traction, and ischemia. Visceral pain is typically described as dull, poorly localized, and often perceived in the midline due to the unmyelinated C-fibers that transmit these signals, entering the spinal cord bilaterally at multiple levels. Furthermore, the location of visceral pain can provide clues to the affected organ system. Pain from foregut structures (e.g., stomach, duodenum) is generally felt in the epigastric region, midgut pain (e.g., small intestine, appendix) is localized to the periumbilical area, and hindgut pain (e.g., colon) is typically experienced in the lower abdomen.
Somatoparietal pain arises from receptors located in the parietal peritoneum, muscles, and skin. Inflammation, stretching, or tearing of the parietal peritoneum activates myelinated A-δ fibers, resulting in pain that is sharp, intense, and well-localized. Movement often exacerbates somatoparietal pain, causing the child to remain still in an attempt to minimize discomfort.
Referred pain, while localized, is felt in areas distant from the affected organ, sharing the same cutaneous dermatome. This phenomenon occurs due to the convergence of afferent neurons from different locations at the same spinal cord level. For instance, diaphragmatic irritation, whether from pleurisy or subphrenic abscess, can manifest as pain in the shoulder or lower neck region.
ETIOLOGY AND DIFFERENTIAL DIAGNOSIS OF PEDIATRIC ABDOMINAL PAIN
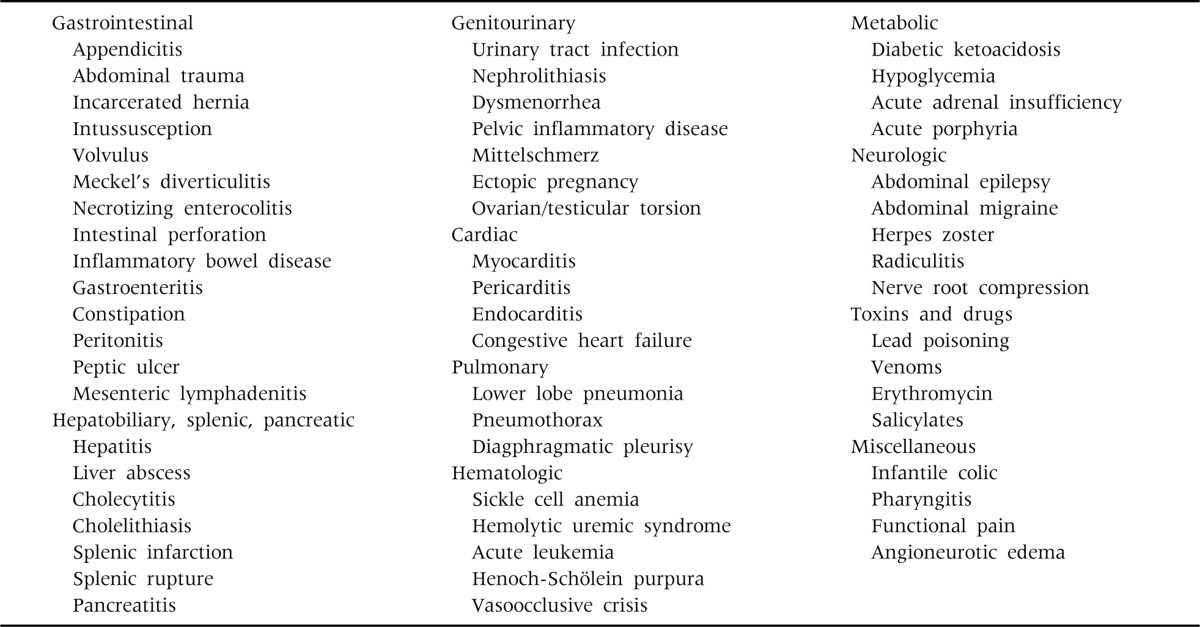
The differential diagnosis of acute abdominal pain in children is extensive, encompassing a wide array of surgical and non-surgical conditions. A comprehensive list of potential causes is presented in Table 1, highlighting the diverse etiologies that must be considered in the diagnostic process.
Table 1: Causes of Acute Abdominal Pain in Children
Life-threatening causes of abdominal pain often involve hemorrhage, obstruction, or perforation of the gastrointestinal tract or intra-abdominal organs. These conditions frequently present with specific clinical features that necessitate prompt recognition and intervention. It’s also important to consider extra-abdominal causes of abdominal pain, such as diabetic ketoacidosis, hemolytic uremic syndrome, and myocarditis, each exhibiting distinct clinical presentations beyond abdominal symptoms. Common, less critical causes of abdominal pain include gastroenteritis, constipation, systemic viral illnesses, infections outside the gastrointestinal tract (e.g., streptococcal pharyngitis, pneumonia, urinary tract infections), mesenteric lymphadenitis, and infantile colic.
Acute Appendicitis: The Most Common Surgical Emergency
Acute appendicitis stands as the most prevalent surgical cause of acute abdominal pain in children. The classic presentation of appendicitis typically begins with visceral, vague, periumbilical pain. Over a period of 6 to 48 hours, as the inflammation extends to the parietal peritoneum, the pain transitions to somatoparietal, becoming well-localized to the right lower quadrant. However, it is crucial to recognize that these textbook manifestations are not always present, particularly in younger children, which can complicate diagnosis. Therefore, appendicitis should remain high on the differential in any previously healthy child presenting with abdominal pain and vomiting, regardless of the presence of fever or classic right lower quadrant tenderness.
Abdominal Trauma: Considering Injury
Abdominal trauma, whether blunt or penetrating, represents a significant cause of acute abdominal pain in children. Trauma can lead to a spectrum of intra-abdominal injuries, including hemorrhage or laceration of solid organs, bowel perforation, organ ischemia from vascular injury, and intramural hematoma. Blunt abdominal trauma is more frequent, often resulting from motor vehicle accidents, falls, or, tragically, child abuse. A detailed history of trauma is essential in these cases.
Intestinal Obstruction: Recognizing Mechanical Blockage
Intestinal obstruction is characterized by cramping abdominal pain and is indicative of serious intra-abdominal pathology requiring urgent diagnosis and surgical or non-surgical management. The causes of intestinal obstruction in children are diverse, including intussusception, malrotation with midgut volvulus, necrotizing enterocolitis (primarily in neonates), incarcerated inguinal hernia, and postoperative adhesions. Bilious vomiting in infants and children should always raise suspicion for bowel obstruction.
Gastroenteritis: The Predominant Medical Cause
Gastroenteritis is the most frequent medical cause of abdominal pain in the pediatric population. Viral pathogens, such as rotavirus, norovirus, adenovirus, and enterovirus, are the predominant culprits. Children with acute gastroenteritis may present with fever, severe cramping abdominal pain, and diffuse abdominal tenderness, often preceding the onset of diarrhea. Bacterial and parasitic infections should also be considered in the differential diagnosis, especially in cases with prolonged or bloody diarrhea, or specific risk factors.
Constipation: A Common and Often Overlooked Cause
Constipation is a common yet often overlooked cause of abdominal pain in children. Fecal impaction can lead to significant lower abdominal pain. Constipation should be suspected in children exhibiting at least two of the following: fewer than three bowel movements per week, fecal incontinence (encopresis), palpable large stools in the rectum or abdomen, retentive posturing, or painful defecation. A thorough history and physical examination, including rectal examination, are crucial for diagnosis.
Mesenteric Lymphadenitis: Mimicking Appendicitis
Mesenteric lymphadenitis, inflammation of the mesenteric lymph nodes, can mimic appendicitis clinically, as the mesenteric lymph nodes are predominantly located in the right lower quadrant. However, the pain in mesenteric lymphadenitis is typically more diffuse, and signs of peritonitis are usually absent. Viral infections are the most common etiology, and other causes include bacterial gastroenteritis, inflammatory bowel disease, and lymphoma. Ultrasound can be a helpful imaging modality in differentiating mesenteric lymphadenitis from appendicitis.
Infantile Colic: Pain in Early Infancy
Infantile colic, particularly in infants with a hypertonic presentation, can manifest as severe abdominal pain. Characteristically, infants with colic exhibit paroxysmal crying episodes, often drawing their knees up to their abdomen. Colic typically emerges in the first few weeks of life and may be relieved by the passage of flatus or stool. While the exact etiology remains unclear, it is considered a diagnosis of exclusion after ruling out other organic causes of abdominal pain.
CLINICAL EVALUATION OF PEDIATRIC ABDOMINAL PAIN
The cornerstone of evaluating a child with acute abdominal pain lies in meticulous history taking and repeated physical examinations. While selective laboratory and radiological investigations play a role in confirming a diagnosis, clinical acumen remains paramount. In cases where the diagnosis remains uncertain after initial assessment, close observation with serial examinations in an emergency department setting is crucial to monitor for evolving signs and symptoms.
History Taking: Unraveling the Narrative
A comprehensive history should encompass the symptom onset pattern, progression, location, intensity, character, and precipitating and relieving factors of the abdominal pain, as well as associated symptoms. The child’s age is a critical factor in guiding the differential diagnosis, as certain conditions are more prevalent in specific age groups, as outlined in Table 2. Other vital historical details include recent abdominal trauma, prior abdominal surgeries, and a thorough review of systems to identify extra-abdominal causes.
Table 2: Differential Diagnosis of Acute Abdominal Pain by Predominant Age
Relief of pain following a bowel movement may suggest a colonic origin, while pain reduction after vomiting might indicate a small bowel issue. In surgical abdominal conditions, pain typically precedes vomiting, whereas vomiting often precedes pain in medical conditions. Bilious vomiting, as mentioned earlier, is a red flag for bowel obstruction.
Physical Examination: A Hands-On Approach
A thorough physical examination is indispensable for accurate diagnosis. This includes examination of the external genitalia, testes, anus, and rectum as part of the abdominal pain evaluation. In sexually active adolescent females, a pelvic examination is also essential to consider gynecological causes of abdominal pain.
General Appearance: Observing the Child’s Demeanor
The child’s general appearance can provide valuable clues. Children with peritoneal irritation tend to remain still, resisting movement, while those with visceral pain may be restless, frequently changing position, or writhing in discomfort.
Vital Signs: Physiological Indicators
Vital signs are crucial in assessing the child’s hemodynamic status and can offer diagnostic insights. Fever suggests an underlying infection or inflammatory process, such as gastroenteritis, pneumonia, pyelonephritis, or intra-abdominal abscess. Tachypnea may indicate pneumonia or respiratory compensation for metabolic acidosis. Tachycardia and hypotension are concerning for hypovolemia or third-space fluid losses, potentially due to dehydration, sepsis, or hemorrhage.
Abdominal Examination: Palpation and Observation
The abdominal examination should commence with gentle palpation, progressing towards the area of maximal tenderness. The examiner should carefully assess the degree of abdominal tenderness, its location, rebound tenderness, rigidity, distension, the presence of any palpable masses, and organomegaly. A rectal examination provides valuable information regarding sphincter tone, the presence of masses, stool consistency, and the presence of hematochezia or melena.
Investigations: Guiding Diagnostic Accuracy
Selective laboratory and radiologic investigations are valuable adjuncts in evaluating pediatric abdominal pain, aiding in assessing the patient’s physiological status and refining the differential diagnosis. A complete blood cell count (CBC) and urinalysis are generally indicated in most patients with acute abdominal pain. Serum glucose and electrolyte measurements help assess hydration status and acid-base balance. A pregnancy test should be performed in postmenarcheal girls to rule out pregnancy-related complications. Figure 1 presents an algorithmic approach to the management of children with acute abdominal pain requiring urgent intervention.
Figure 1: Algorithmic Approach to Pediatric Acute Abdominal Pain
Plain abdominal radiographs are useful when intestinal obstruction or perforation is suspected, while chest radiographs can help exclude pneumonia as a cause of abdominal pain. In the emergency department setting, ultrasound and computed tomography (CT) are frequently employed to further investigate the etiology of abdominal pain. While CT is generally considered more accurate, ultrasound is often favored as the initial imaging modality for pediatric abdominal pain due to its non-invasive nature, lack of ionizing radiation, and lower cost.
MANAGEMENT OF PEDIATRIC ABDOMINAL PAIN
Management strategies for acute abdominal pain in children are directed towards addressing the underlying cause. As illustrated in Figure 1, urgent intervention is warranted for children who appear prostrated or toxic, exhibit signs of bowel obstruction, or demonstrate evidence of peritoneal irritation. Initial resuscitation measures include addressing hypoxemia, restoring intravascular volume deficits, and correcting metabolic derangements. Nasogastric decompression may be necessary in cases of bowel obstruction. Empiric intravenous antibiotics are often indicated when there is clinical suspicion of a serious intra-abdominal infection, such as appendicitis with perforation or peritonitis. Furthermore, adequate analgesia should be provided to children experiencing severe pain, ideally before surgical evaluation, to ensure patient comfort and facilitate accurate assessment.
CONCLUSION: Timely Diagnosis for Optimal Outcomes
Acute abdominal pain is a common pediatric complaint that necessitates efficient and accurate diagnosis and management, particularly in the emergency department. While the majority of cases are benign and self-limiting, the critical challenge lies in promptly identifying potentially life-threatening conditions such as appendicitis, intussusception, or bowel obstruction. Meticulous history taking, thorough and repeated physical examinations, and judicious use of investigations are essential to establish the correct diagnosis, guide appropriate management, and ultimately improve outcomes for children presenting with acute abdominal pain.