A nursing diagnosis is a cornerstone of patient care, acting as a critical link in the nursing process. For healthcare professionals, especially nurses, it’s more than just a label; it’s a roadmap to effective and personalized patient care.
This guide dives deep into the world of nursing diagnosis, particularly focusing on Wellness Diagnosis Care Plan Example. We will explore its significance within the nursing process, different types of diagnoses, and how to construct and implement a nursing diagnosis, with a special emphasis on wellness and health promotion.
Let’s begin our exploration to understand how nursing diagnosis shapes patient well-being.
Deciphering the Nursing Process
Before we delve into nursing diagnosis, it’s essential to understand the broader context – the nursing process. This systematic approach comprises five integral steps, with diagnosis as the second crucial stage.
Assessment – The initial step involves a comprehensive patient evaluation. This includes gathering vital data such as vital signs, medical history, psychological assessments, and socioeconomic factors. This holistic data collection forms the bedrock of the nursing process.
Diagnosis – Following assessment, nurses formulate a nursing diagnosis based on the collected data. This diagnosis is not just a label but a directive, guiding the specific nursing care the patient will receive. It’s about identifying patterns and needs from the assessment data.
Outcomes and Planning – In this phase, nurses develop a tailored care plan, drawing directly from the insights of the nursing diagnosis. Planning here is crucial – it must be measurable, goal-oriented, and patient-centric, setting the stage for effective intervention.
Implementation – This is where the care plan transitions from paper to practice. It involves putting the planned interventions into action throughout the patient’s care journey, from hospitalization to discharge, ensuring consistent and focused care.
Evaluation – The final step is critical for continuous improvement. It involves a thorough evaluation of the care plan against the initial goals and desired outcomes. If results don’t align, the care plan is dynamically adjusted to better meet the patient’s evolving needs, creating a cycle of improvement.
What Exactly is a Nursing Diagnosis?
As highlighted, a nursing diagnosis is a pivotal step in the nursing process. It serves as a structured and evidence-based method for nurses to articulate their professional judgments clearly and effectively. This communication is vital not only within the nursing team but also with patients, other medical professionals, and the wider public. Originating from the assessment phase, the nursing diagnosis directly informs the subsequent care plan, which in turn becomes the benchmark for evaluating patient care outcomes.
NANDA International (NANDA-I), the globally recognized authority, standardizes nursing diagnosis terminology and practices. Their official definition is:
“A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability.”
This definition underscores that a nursing diagnosis is about understanding and addressing the patient’s response to health issues, not just the health issues themselves.
Navigating Different Types of Diagnoses
In healthcare, various types of diagnoses are encountered. It’s crucial to distinguish between nursing, medical, and collaborative diagnoses to understand each role in patient care.
A nursing diagnosis is the nurse’s interpretation and labeling of patient data gathered during assessment, using NANDA-I approved diagnoses. For example, observing a patient coughing before swallowing, showing difficulty in throat elevation, and reporting a sensation of food being “stuck” might lead to a nursing diagnosis of impaired swallowing. This diagnosis focuses on the patient’s functional challenges.
Examples of nursing diagnoses: risk for unstable blood glucose level; toileting self-care deficit; disturbed thought process; sedentary lifestyle.
Conversely, a medical diagnosis is made by a physician or advanced practitioner. It identifies diseases, medical conditions, or pathological states, falling within the medical domain. Medical diagnoses, such as diabetes or pneumonia, typically remain constant in a patient’s medical history, while nursing diagnoses can evolve as the patient’s condition changes.
Examples of medical diagnoses: myocardial infarction; asthma; osteoarthritis; depression.
Collaborative diagnoses, on the other hand, necessitate both nursing and medical interventions. These situations require interdisciplinary teamwork, with nurses monitoring patient problems and medical professionals prescribing treatments and further investigations.
Examples of collaborative diagnoses: potential complication of electrolyte imbalance; risk of complication related to medication interaction.
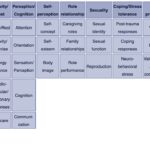
The NANDA-I Classification System
To ensure clarity and organization, nursing diagnoses are systematically classified by NANDA-I in Taxonomy II, a system refined over two decades. This taxonomy is structured into three levels: 13 domains, 47 classes, and 267 specific nursing diagnoses, providing a robust framework for categorizing patient needs.
The domains and classes are structured to cover a broad spectrum of human experiences related to health:
-
Domain 1: Health Promotion
-
-
- Class 1. Health Awareness
- Class 2. Health Management
- Class 1. Health Awareness
-
-
Domain 2: Nutrition
-
-
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Class 1. Ingestion
-
-
Domain 3: Elimination and Exchange
-
-
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
- Class 1. Urinary function
-
-
Domain 4: Activity/Rest
-
-
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
- Class 1. Sleep/Rest
-
-
Domain 5: Perception/Cognition
-
-
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Class 1. Attention
-
-
Domain 6: Self-Perception
-
-
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
- Class 1. Self-concept
-
-
Domain 7: Role relationship
-
-
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
- Class 1. Caregiving roles
-
-
Domain 8: Sexuality
-
-
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
- Class 1. Sexual identity
-
-
Domain 9: Coping/stress tolerance
-
-
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
- Class 1. Post-trauma responses
-
-
Domain 10: Life principles
-
-
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
- Class 1. Values
-
-
Domain 11: Safety/Protection
-
-
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
- Class 1. Infection
-
-
Domain 12: Comfort
-
-
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
- Class 1. Physical comfort
-
-
Domain 13: Growth/Development
-
- Class 1. Growth
- Class 2. Development
- Class 1. Growth
Categories of Nursing Diagnoses: Problem-Focused, Risk, Health Promotion, and Syndrome
NANDA-I categorizes nursing diagnoses into four main types: problem-focused, risk, health promotion, and syndrome diagnoses, each addressing different aspects of patient health.
Problem-focused diagnoses (or actual diagnoses) identify existing patient issues evident during assessment. They are based on observable signs and symptoms and consist of three parts: the diagnosis label, related factors, and defining characteristics. For instance, “Acute Pain related to surgical incision as evidenced by patient report of pain score 7/10 and guarding behavior.”
Risk diagnoses identify potential health problems a patient is vulnerable to developing if no intervention occurs. They indicate a problem is not present, but risk factors suggest it could arise. These diagnoses guide preventative nursing care. They include two components: a risk diagnostic label and risk factors. An example is “Risk for Infection related to surgical incision and invasive procedures.”
Health promotion diagnoses, also known as wellness diagnoses, focus on a patient’s desire and motivation to enhance well-being and achieve their full health potential. These diagnoses highlight a patient’s readiness to improve specific health behaviors and can apply to individuals, families, groups, or communities. This is where the concept of wellness diagnosis care plan example becomes particularly relevant.
Syndrome diagnoses are less common and refer to a cluster of nursing diagnoses that frequently occur together and are managed with similar interventions. They recognize patterns of diagnoses rather than isolated issues.
Examples of each diagnosis type from NANDA-I’s Nursing Diagnosis: Definitions and Classifications, 2021-2023 are listed below:
| Problem Focused Diagnosis | Risk Diagnosis |
|---|---|
| – Ineffective thermoregulation | – Risk for falls |
| – Impaired physical mobility | – Risk for imbalanced body temperature |
| – Acute confusion | – Risk for delayed surgical recovery |
| – Deficient fluid volume | – Risk for aspiration |
| – Disturbed body image | – Risk for loneliness |
| Health Promotion Diagnosis | Syndrome Diagnosis |
| – Readiness for enhanced knowledge | – Chronic pain syndrome |
| – Readiness for enhanced nutrition | – Disuse syndrome |
| – Readiness for enhanced power | – Impaired environmental interpretation syndrome |
| – Readiness for enhanced spiritual well-being | – Sudden infant death syndrome risk |
| – Readiness for enhanced self-care | – Frail elderly syndrome |
Components of a Robust Nursing Diagnosis
A well-formulated nursing diagnosis includes specific components, varying slightly depending on the diagnosis type. These components ensure clarity, accuracy, and effective communication.
Diagnosis Label – This is a concise name summarizing the diagnostic focus and nursing judgment.
Examples: ineffective breathing pattern; impaired verbal communication; deficient knowledge.
Definition – A clear, precise description of the diagnosis, differentiating it from similar diagnoses.
Example: For “Disturbed Sleep Pattern,” the definition is: “Time-limited and or sustained disruption of natural sleep amount and restorative qualities.”
Defining Characteristics – Observable cues that indicate a problem-focused, health promotion, or syndrome diagnosis. These are what nurses assess through sight, sound, touch, smell, and patient reports.
Example: For “Anxiety,” defining characteristics may include restlessness, irritability, increased heart rate, and verbalization of feeling anxious.
Risk Factors – Environmental, physiological, psychological, genetic, or chemical elements increasing a patient’s vulnerability to an unhealthy event. These are exclusive to risk diagnoses.
Example: Risk factors for “Risk for Falls” might include age >65, history of falls, impaired mobility, and medication side effects.
Related Factors – Factors that appear to have a connection with a problem-focused nursing diagnosis or syndrome. They may precede, contribute to, or be associated with the diagnosis. Health promotion diagnoses may sometimes include related factors.
Example: For “Ineffective Tissue Perfusion (peripheral),” related factors can include diabetes mellitus, hypertension, smoking, and sedentary lifestyle.
Constructing a Nursing Diagnosis Statement
Formulating a nursing diagnosis statement requires careful analysis of patient data to identify health problems, risks, and strengths. NANDA International recommends a structured format for accurate, clear, and universally understandable diagnoses.
The structure varies for each type of nursing diagnosis:
- Problem-focused diagnosis:
[Nursing Diagnosis Label] related to [Related Factors] as evidenced by [Defining Characteristics].
Example: Acute Pain related to surgical incision as evidenced by patient reporting pain score of 8/10 and guarding incision site.
- Risk Diagnosis:
Risk for [Nursing Diagnosis Label] as evidenced by [Risk Factors].
Example: Risk for Infection as evidenced by surgical incision and compromised skin integrity.
- Health Promotion Diagnosis (Wellness Diagnosis):
Readiness for enhanced [Health Behavior] as evidenced by [Expressed desire to enhance behavior].
Example: Readiness for enhanced nutrition as evidenced by patient expressing interest in learning about healthy eating and meal planning.
- Syndrome Diagnosis:
[Syndrome Diagnosis Label]. (Syndromes are typically recognized labels without further components in the statement itself).
Example: Chronic Pain Syndrome.
Wellness Diagnosis Care Plan Example: Promoting Healthy Lifestyle
Let’s focus on wellness diagnosis care plan example to illustrate its practical application.
Scenario: A 45-year-old patient expresses a desire to improve their overall health and adopt a healthier lifestyle. During assessment, you note they are currently sedentary, have a diet high in processed foods, and express feeling stressed due to work demands.
Nursing Diagnosis (Health Promotion): Readiness for enhanced health management as evidenced by expressed desire to improve lifestyle habits.
Care Plan Goals:
- Short-term Goal: Patient will identify three specific, realistic, and measurable health goals within one week.
- Long-term Goal: Patient will demonstrate consistent engagement in chosen healthy behaviors (e.g., regular exercise, improved dietary choices, stress management techniques) for at least three months.
Nursing Interventions:
-
Collaborative Goal Setting (Week 1):
- Discuss the benefits of a healthy lifestyle and explore the patient’s motivations for change.
- Guide the patient to identify areas for improvement (diet, exercise, stress).
- Assist in setting SMART (Specific, Measurable, Achievable, Relevant, Time-bound) goals. For example: “Walk for 30 minutes three times a week,” “Replace sugary drinks with water,” “Practice deep breathing exercises for 10 minutes daily.”
- Provide resources and information on healthy eating, exercise options, and stress management techniques.
-
Nutritional Guidance (Weeks 2-4):
- Educate the patient on balanced nutrition, portion control, and healthy food choices.
- Offer sample meal plans and recipes focusing on whole foods, fruits, and vegetables.
- Encourage the patient to keep a food diary to track intake and identify areas for improvement.
- Provide referrals to a registered dietitian if needed for more in-depth nutritional counseling.
-
Exercise and Activity Promotion (Weeks 2-4):
- Discuss different types of physical activity and help the patient choose activities they enjoy and can realistically incorporate into their routine.
- Start with small, achievable exercise goals and gradually increase intensity and duration.
- Offer guidance on safe exercise practices and encourage patient to consult with their physician before starting a new exercise program.
-
Stress Management Techniques (Weeks 2-4):
- Teach relaxation techniques such as deep breathing, meditation, or progressive muscle relaxation.
- Explore stress-reducing activities like hobbies, spending time in nature, or social engagement.
- Discuss time management strategies and work-life balance.
- Provide information on community resources for stress management and mental well-being.
-
Ongoing Support and Evaluation (Months 1-3):
- Schedule regular follow-up appointments (phone or in-person) to monitor progress, provide encouragement, and address any challenges.
- Review the patient’s food diary, exercise log, and stress management practices.
- Celebrate successes and adjust the care plan as needed based on the patient’s progress and feedback.
- Re-evaluate goals and set new ones as the patient achieves initial targets.
This wellness diagnosis care plan example demonstrates a proactive approach to healthcare, focusing on empowering patients to take charge of their well-being through education, support, and personalized strategies. It emphasizes the nurse’s role in facilitating health promotion and guiding patients towards sustainable lifestyle changes.
Expanding Your Nursing Diagnosis Toolkit
The NANDA-I nursing diagnosis list, with its 267 entries, is a comprehensive resource for nurses worldwide. Throughout this guide, we’ve utilized examples from the NANDA-I 2021-2023 handbook. Here are additional nursing diagnosis examples to further enrich your care planning capabilities:
- Readiness for enhanced self-concept
- Risk for caregiver role strain
- Impaired memory
- Deficient diversional activity
- Ineffective relationship
- Spiritual distress
- Risk for falls
- Impaired skin integrity
- Urinary incontinence (functional, reflex, stress, urge)
- Constipation
- Diarrhea
- Nausea
- Readiness for enhanced comfort
- Readiness for enhanced coping
- Readiness for enhanced family processes
- Readiness for enhanced parenting
Embracing Nursing Diagnosis for Enhanced Patient Care
Nursing diagnoses are indispensable tools that empower nurses to deliver safe, high-quality, and evidence-based care. Mastering the art and science of nursing diagnosis—from understanding its types and components to crafting effective care plans, especially in wellness and health promotion—is fundamental for every nurse committed to patient well-being. By utilizing nursing diagnoses effectively, healthcare professionals can significantly impact patient outcomes and contribute to a healthier future.