Introduction
Conjunctivitis, broadly defined as inflammation of the conjunctiva, represents a common group of ocular diseases frequently encountered in primary care settings.1 Infectious conjunctivitis is predominantly viral in origin (~80% of cases), followed by bacterial infections.1,2 Non-infectious forms include allergic, mechanical, irritative, toxic, immune-mediated, and neoplastic etiologies.1 Among these, allergic conjunctivitis is the most prevalent non-infectious type, affecting approximately 40% of the US population.2 Conjunctivitis can be further categorized based on onset and clinical course as acute, chronic, or recurrent.1,2 Viral and bacterial conjunctivitis typically present acutely, or less commonly, hyperacutely. Mechanical, irritative, toxic, immune-mediated, and neoplastic forms are generally associated with chronic inflammation,1 although toxic conjunctivitis can have an acute onset. Allergic conjunctivitis can manifest chronically, often beginning in childhood, with acute exacerbations linked to seasonal allergens or contact lens wear.1
Conjunctivitis is a frequent reason for consultation in primary care, accounting for roughly 2% of all medical visits in the United States3 and numerous self-referrals to community pharmacies.4 Accurate epidemiological data is challenging to obtain due to self-treatment, delayed medical care, and diagnostic inaccuracies in primary care. Approximately 70% of patients presenting with acute red eye are seen in primary care and urgent care settings,5 creating a significant economic and social burden.6–8 The economic impact of infectious conjunctivitis is substantial, encompassing costs related to repeat visits, referrals, insurance co-pays, medications, and lost productivity from work or school absences. In the US, acute conjunctivitis affects an estimated 6 million individuals annually,2 with bacterial conjunctivitis treatment alone costing between $377–857 million each year. Notably, there is a lack of published studies on the health-related quality of life in patients with acute infectious conjunctivitis.
This review aims to offer practical guidance on the Differential Diagnosis In Primary Eye Care Pdf for acute infectious conjunctivitis and to highlight discrepancies between current diagnostic practices and optimal management in primary care settings.
Challenges in Acute Infectious Conjunctivitis Management and Diagnosis
While eye care specialists often manage complex cases of acute infectious conjunctivitis, primary care physicians frequently encounter these conditions. However, suboptimal management in primary care is often observed due to an underestimation of viral conjunctivitis prevalence and a high rate of antibiotic prescriptions (~80%) for infectious conjunctivitis.9 This occurs despite clinical guidelines that discourage antibiotic use for self-limiting illnesses.10 Antibiotic prescriptions are often used as an indicator of a presumed bacterial diagnosis, yet clinical accuracy in diagnosing viral conjunctivitis may be as low as 9%.11 Observational data suggests that bacterial pathogens are confirmed in only 30–50% of suspected bacterial conjunctivitis cases through laboratory testing.9,11
Misdiagnosis leads to unnecessary antibiotic exposure. The Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) study, which analyzed 3237 ocular isolates from bacterial eye infections across 72 US centers (2009-2013), found that nearly half were methicillin-resistant staphylococci.12 While the direct contribution of topical antibiotics to antibiotic resistance is debated,11 current resistance trends necessitate careful consideration before prescribing antibiotics for common eye infections.13 Prescribing antibiotics for unconfirmed bacterial infections also contradicts Antibiotic Stewardship initiatives, which are integral to primary care and pediatric practice protocols.14 Beyond antibiotic resistance, misdiagnosis can result in recurrent infectious conjunctivitis, especially in children, or progression to serious ocular and extra-ocular complications.
Several factors complicate accurate diagnosis of acute infectious conjunctivitis. Firstly, clinical overlap exists between viral, bacterial, and allergic forms, making differential diagnosis challenging.11 Distinguishing between viral and bacterial origins based on non-specific clinical signs and symptoms, such as discharge type, is unreliable and not supported by evidence-based diagnostic criteria.11,15 Routine bacterial cultures are typically not performed nor practical for suspected acute bacterial conjunctivitis management,15 except in neonates.1 Cultures should be considered in immunocompromised patients or hyperacute cases. The misdiagnosis issue is further compounded by the common belief that all cases require topical antibiotics, even though most are self-limiting.16,17 Social pressures, such as school policies or work absence concerns, may also prompt primary care providers to prescribe antibiotics.11 Finally, the healthcare entry point significantly influences diagnostic accuracy.
Guidelines for diagnosing and treating acute infectious conjunctivitis based on etiology and natural history are available.1 However, greater awareness and adherence to differential diagnosis principles are crucial to improve outcomes for patients presenting with suspected acute infectious conjunctivitis.17
Epidemiology and Clinical Presentation
Key differentiating features of viral, bacterial, and allergic acute conjunctivitis are summarized in Table 1.1,2,[18](#CIT0018]
Table 1. Discriminating Clinical Features of Suspected Acute Conjunctivitis
| Type | Conjunctival | Itching | Discharge | Lymphadenopathy | Associated Fever and Sore Throat |
|---|---|---|---|---|---|
| Viral | Follicular | Minimal | Watery | Common (~50%) | Common |
| Adenoviral | |||||
| HSV | |||||
| VZV | |||||
| Bacterial | Papillary | Minimal | Purulent | Uncommon | Occasionally |
| Nongonococcal | Mucopurulent | ||||
| Gonococcal | Hyperpurulent | ||||
| Chlamydial | Follicular | Minimal | Mucopurulent | Common | No |
| Allergic | Papillary with chemosis | Severe | Watery | None | No |
| Mucoid |
Note: Data from these studies.1,2,[18](#CIT0018]
Abbreviations: HSV, herpes simplex virus; VZV, varicella (herpes) zoster virus.
Viral Conjunctivitis
Adenoviruses are responsible for the majority (65–90%) of viral conjunctivitis cases, while herpes simplex virus (HSV) accounts for 1.3–4.8% of acute conjunctivitis cases.2 Other viruses associated with conjunctivitis include varicella zoster virus (VZV) and Molluscum contagiosum.1
Adenoviruses are non-enveloped and resistant to disinfection.19 Adenoviral conjunctivitis is highly contagious due to the virus’s ability to survive in a dry state at room temperature for weeks.20 Transmission risk ranges from 10–50%, spreading through direct contact or shared items.2 Adenoviral conjunctivitis is self-limiting, with symptom improvement within 5–14 days.1 It often starts unilaterally and progresses to both eyes.
Adenovirus serotypes are linked to different ocular infections,21 including pharyngoconjunctival fever and epidemic keratoconjunctivitis (EKC; patient photos in Figure 1). Pharyngoconjunctival fever typically presents bilaterally with fever and periauricular lymph node enlargement.2 EKC is more severe due to potential visual acuity impact; it is characterized by watery discharge, swelling, redness, and bilateral neck lymph node involvement.2,21 EKC is highly contagious, and asymptomatic carriers can unknowingly spread the virus.21
Figure 1. Case photographs of adenoviral conjunctivitis.
(A) gross examination of acute adenoviral conjunctivitis; (B) bilateral AdenoPlus-positive EKC; (C) high magnification of the conjunctiva of positive EKC. Photos provided by Scott Hauswirth and Elizabeth Yeu. Patients have consented to photo publication. Abbreviation: EKC, epidemic keratoconjunctivitis.
EKC complications include pseudomembrane formation on the palpebral conjunctiva in early and late stages.21,22 Manual removal can prevent symblepharon in severe cases and causes minimal bleeding without epithelial damage.22 Subepithelial infiltrates can develop in the cornea 7–10 days post-infection onset,23 persisting for weeks or years.22 Untreated infiltrates can cause corneal scarring, irregular astigmatism, and vision loss.24 Topical corticosteroids or steroid-sparing agents like cyclosporine eye drops can reduce scarring risk;22 however, corticosteroids should be used cautiously, especially in later recovery stages.21,25 Subepithelial infiltrates can also occur in chlamydial conjunctivitis.1 As no approved medications exist for adenoviral conjunctivitis, treatment is supportive (cold compresses, artificial tears)1 with infection control education, as viral shedding continues post-onset.1,25
Few virucidal agents are in preclinical development. Povidone-iodine (PVP-I) is being explored for its broad-spectrum antimicrobial activity.1 A PVP-I 0.6%/dexamethasone 0.1% ophthalmic suspension (PVP-I 0.6%/DEX 0.1%) showed significant clinical resolution and adenovirus eradication in a Phase 2 trial for acute adenoviral conjunctivitis.26 N-chlorotaurine, with broad-spectrum microbicidal activity, is also under investigation for viral conjunctivitis treatment.27 A 1% N-chlorotaurine solution was well-tolerated in EKC patients and shortened disease duration compared to gentamicin eye drops in a phase 2b study.27 Topical ganciclovir 0.15% ophthalmic gel is FDA-approved for acute herpetic keratitis in the US.1
Prior HSV infection predisposes to HSV conjunctivitis, with reactivation triggered by stress, trauma, UV light, or other viral illnesses.1 HSV conjunctivitis is usually unilateral, with bulbar conjunctival injection, thin watery discharge, and mild follicular conjunctival reaction.1,2 Vesicular eyelid lesions and pleomorphic or dendritic epithelial keratitis on the cornea or conjunctiva are distinctive signs.1 These corneal/conjunctival signs may be present without eyelid lesions and are best visualized with vital dyes like sodium fluorescein, lissamine green, or rose Bengal. HSV conjunctivitis usually resolves in 4–7 days unless complications occur. Topical and/or oral antivirals are recommended to shorten illness duration.1,2 Topical corticosteroids should be avoided due to potential HSV potentiation,1,[2](#CIT0002] especially with corneal or conjunctival epithelial disease.1,[2](#CIT0002] HSV can also cause EKC, clinically similar to adenoviral conjunctivitis.28
Active chickenpox or prior exposure to chickenpox/shingles predisposes to VZV conjunctivitis.1 VZV conjunctivitis is commonly unilateral. Distinctive signs include eyelid, conjunctiva, cornea, or uvea inflammation.2 Uveitis may cause increased intraocular pressure, sometimes to dangerous levels.29 VZV conjunctivitis usually resolves within days.1 Oral antivirals and topical corticosteroids can be used cautiously for VZV conjunctivitis,1,30 as topical antivirals alone are ineffective.1
Bacterial Conjunctivitis
Approximately 32% of acute infectious conjunctivitis cases are bacterial, based on bacterial culture prevalence in adults presenting to primary care with red eye and (muco)purulent discharge or glued eyelids.9 Bacterial conjunctivitis is usually unilateral but can be bilateral.1 Staphylococcal species are the most common adult pathogens, followed by Streptococcus pneumoniae and Haemophilus influenzae.2 In children, bacterial infections cause 50–75% of conjunctivitis, often S. pneumoniae, H. influenzae, or Moraxella catarrhalis. Hyperacute bacterial conjunctivitis is caused by Neisseria gonorrhoeae or Chlamydia trachomatis.
Acute bacterial conjunctivitis has a rapid onset of conjunctival redness and mucopurulent discharge.1,2 Symptoms may include burning and itching, though less common.31 Acute bacterial conjunctivitis is self-limiting, resolving in 7–10 days.2 Broad-spectrum topical antibiotics should be delayed,1,2,[10](#CIT0010] and no evidence suggests superiority of any topical antibiotic agent.1 Methicillin-resistant Staphylococcus aureus (MRSA) conjunctivitis accounts for 3–64% of ocular staphylococcal infections[2](#CIT0002] and requires ophthalmologist management with MRSA-active antibiotics, like besifloxacin ophthalmic suspension.32
Hyperacute bacterial conjunctivitis (often N. gonorrhoeae) requires immediate ophthalmic management to prevent corneal involvement and perforation.1 Symptoms include purulent discharge, reduced visual acuity, eye tenderness, and swollen lymph nodes. Rising gonorrhea incidence was declared an urgent public health threat in the US in 2015.33 Reported gonorrhea cases increased 67% from 2013 to 2017 (555,608 cases in 2017),34,[35](#CIT0035] with an 18.6% increase between 2016 and 2017.34 Gonococcal ocular infection can occur in neonates after vaginal delivery from infected mothers.1 Treatment includes intramuscular ceftriaxone for all ages and oral azithromycin or doxycycline for adults.2 CDC guidelines in 2015 recommended dual therapy with ceftriaxone and azithromycin due to increased N. gonorrhoeae resistance to previous treatments.36 Bacterial conjunctivitis lasting over 4 weeks is chronic.2
Chlamydia causes 1.8–5.6% of acute conjunctivitis cases.2 Chlamydial conjunctivitis is primarily unilateral with concurrent genital infection[1](#CIT0001] and presents with conjunctival redness, lymphoid follicles, or mild purulent discharge.1,2 Bulbar conjunctival follicles are a distinctive sign in adults, absent in neonates/infants.1 Chlamydial conjunctivitis is typically sexually transmitted.1 Chlamydia is the most common sexually transmitted disease in the US, with 1,708,569 cases reported in 2017.37 Reported chlamydia cases in the US increased 22% from 2013 to 2017.38 Neonates can be infected during vaginal delivery by infected mothers.1 Treatment includes oral azithromycin or doxycycline in adults and erythromycin in neonates.
Allergic Conjunctivitis
Most allergic conjunctivitis cases are due to seasonal allergies, presenting with bilateral symptoms.1 Key symptoms are mild to severe itching and redness,[18](#CIT0018] with watery or mucoid discharge.1 Treatment includes supportive measures (cold compress, artificial tears), topical or oral antihistamines, and mast cell inhibitors. Short-term topical corticosteroids can be used in select cases, after ruling out corneal involvement and herpetic infection, as steroids can worsen both.1,2
Differential Diagnosis
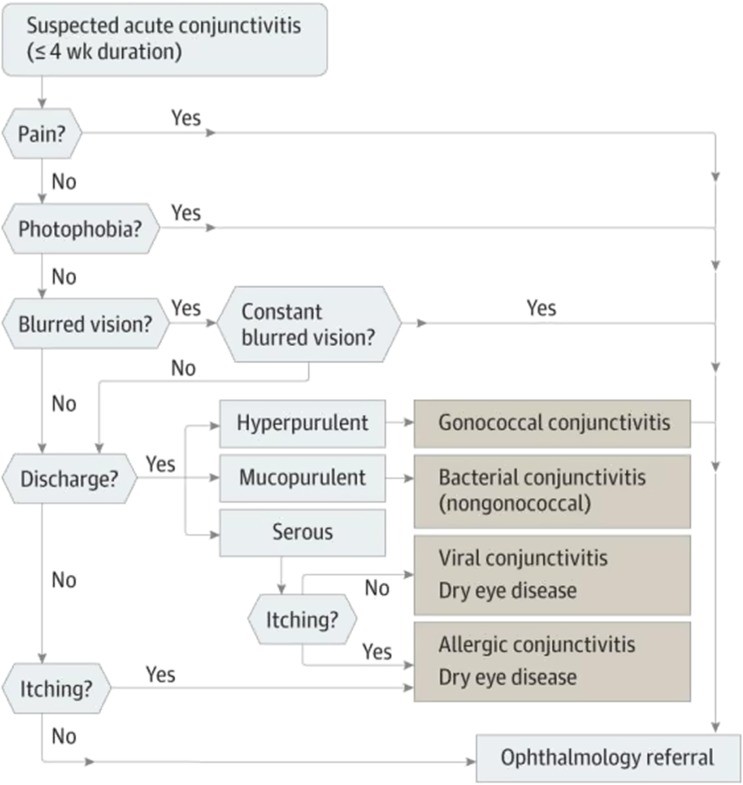
To align with the American Academy of Ophthalmology Preferred Practice Pattern guidelines, which emphasize treating the underlying cause of conjunctivitis,[1](#CIT0001] physicians should adopt a systematic approach (Figure 2). This approach involves considering the epidemiological context of infectious conjunctivitis, patient history, clinical examination, and diagnostic tests when necessary.
Figure 2. Differential diagnosis algorithm for suspected acute conjunctivitis.
Reproduced with permission from JAMA. 2013;310(16):1721–1729. Copyright©2013 American Medical Association. All rights reserved.2
Clinical Examination
Initial diagnosis must rule out serious causes of acute red eye. Historical evaluation includes pain or photophobia, which may indicate bacterial keratitis, anterior uveitis, or acute angle-closure glaucoma.39 Upper respiratory infection symptoms or known exposure to infected individuals suggest viral conjunctivitis.39 Patient history of ocular trauma should be considered. Corneal abrasion from foreign bodies or UV exposure can present as red eye.39 Red, painful, watery eyes from corneal or conjunctival foreign bodies can mimic acute and chronic conjunctivitis. Foreign body presence is determined via history and biomicroscopic exam. Contact lens wearers have a higher risk of corneal involvement and bacterial keratitis and should be referred to eye care specialists.2,39 Dry eye disease can mimic acute infectious conjunctivitis with hyperemia,[32](#CIT0032] grittiness, and stinging.40 Adhering to triage questions and risk factor analysis from the Tear Film & Ocular Surface Society Dry Eye Workshop II (TFOS DEWS II)40 helps exclude dry eye, although it can coexist with acute infectious conjunctivitis due to high prevalence of both. Immune-mediated conjunctivitis (e.g., ocular mucous membrane pemphigoid, graft-versus-host disease, Stevens-Johnson syndrome) early, milder forms may share symptoms with acute infectious conjunctivitis (redness, tearing, clear discharge, conjunctival injection).1 However, these often differ in time course, being protracted and resembling chronic processes more than acute episodes.
Medication history is informative; anticoagulants are linked to subconjunctival hemorrhage, and topiramate to angle-closure glaucoma. Patients needing steroids may have more severe disease or other pathology and should be referred to eye care specialists.2 Clinical examination should assess lymph nodes (submandibular and preauricular). Lymphadenopathy, like enlarged, tender preauricular nodes, is more common in viral than bacterial conjunctivitis.31
Physical eye examination should assess visual acuity, discharge type, corneal opacity, pupil abnormalities, eyelid swelling, and orbit protrusion/asymmetry.1,2,31 Immediate referral to an ophthalmologist or eye care professional is needed for visual loss, moderate to severe pain, severe purulent discharge, or corneal involvement.1,2 A penlight can be useful without a slit lamp, especially for anterior chamber depth and ruling out angle closure.2 Viral conjunctivitis presentation varies, but tearing, clear to white discharge, redness, and bilaterality are common. It often starts in one eye, then the other within days.15 Bacterial conjunctivitis is suggested by glued eyelids, lack of itching, and no prior conjunctivitis history.9 A diagnostic index by van Weert et al indicates younger adults without glued eyelids upon waking are less likely to have bacterial conjunctivitis; risk increases with age and two glued eyes.11
A slit lamp allows detailed conjunctival epithelium examination, differentiating inflammation types (follicular – infectious; papillary – allergic; pseudomembranous – severe EKC; eosinophilic – allergic). Fluorescein staining with slit lamp highlights corneal uptake patterns and anterior chamber inflammation.39 HSV infection typically shows branching lesions with intensely stained end bulbs, while VZV lesions are highly branched without end bulbs.39
Diagnostic Tests
Viral diagnostic tests are not routine in primary care, but increased access can improve diagnostic accuracy. PCR for adenoviral DNA in tear fluid is more common, but cost and training still limit use.28 Viral cell culture with confirmatory immunofluorescence is time-consuming and rare.28
Rapid in-office tests, like AdenoPlus (Quidel, San Diego, CA, USA), are promising for timely diagnosis and reducing unnecessary antibiotics.6,28,41,42 Accurate point-of-care adenovirus detection could also reduce societal costs of acute conjunctivitis.6 AdenoPlus detects adenovirus serotypes via antigen-based microfiltration sampling.28,42 Sensitivity ranges from 39.5 to 93%.28,41,42 Sambursky et al. noted potential artificial sensitivity inflation due to testing conditions,[28](#CIT0028] and Holtz et al. suggested real-time PCR to verify negative results.42 Clinical judgment may outweigh test results regarding treatment, partly because no ophthalmic agent is indicated for viral conjunctivitis.
Conjunctival cultures are needed for suspected neonatal infectious conjunctivitis.1 Bacterial cultures are recommended for recurrent, severe, or chronic purulent infectious conjunctivitis at any age.1 ESwab (Copan Diagnostics, Murrieta, CA, USA) offers convenient sample preparation for bacterial testing where culture plating is less common.43 ESwab is a liquid-based collection and transport system suitable for automation, Gram stains, and traditional culture.43 It maintains bacterial viability at room temperature for ≤48 hrs.43 Suspected adult and neonatal chlamydial conjunctivitis can be confirmed using immunofluorescent antibody tests and enzyme-linked immunosorbent assays.1 PCR testing of ocular samples is not currently FDA-approved. Gram or Giemsa staining of conjunctival cytology smears is recommended for diagnosing neonatal or gonococcal conjunctivitis at any age.1,44 Conjunctival biopsy with immunofluorescent staining can be considered for unresponsive conjunctivitis.1
Conclusions
Diagnosing acute infectious conjunctivitis is complex due to overlapping signs and symptoms with other inflammatory conjunctival conditions, leading to high misdiagnosis rates. Misdiagnosing viral as bacterial conjunctivitis can result in inappropriate antibiotic use, contributing to antibiotic resistance. Misdiagnosis can also impair quality of life and productivity due to poor outcomes. Adherence to American Academy of Ophthalmology guidelines and enhanced patient and physician education can improve acute infectious conjunctivitis management. Antibiotic prescriptions should be delayed until bacterial etiology is confirmed, and educational materials should be provided to primary and emergency care practitioners. Developing broad-spectrum antimicrobial agents may offer new treatment options without resistance concerns.26,27,45
Acknowledgments
The authors thank Dr. Terry O’Brien for his valuable discussions and insights during the initial manuscript phase. The authors also acknowledge Daniella Babu, PhD, of Excel Medical Affairs, for medical writing assistance, funded by Shire, a Takeda company.
Funding
Medical writing support was funded by Shire (a Takeda company). Shire (a Takeda company) reviewed the manuscript for medical accuracy only.
Disclosure
EY has consulted for Allergan, Bausch & Lomb, JJV, Novartis, Shire (a Takeda company), TearLab, and TissueTech during the study. EY has also consulted for Alcon, Aurea Medical, Avedro, Avellino, BioTissue, Beaver Visitec, BlephEx, Bruder, CorneaGen, Dompe, EyePoint Pharmaceuticals, iOptics, Glaukos, Guidepoint, LENSAR, Kala Pharmaceuticals, Merck, Mynosys, Ocular Science, Ocular Therapeutix, Ocusoft, Omeros, Oyster Point Pharmaceuticals, Science Based Health, Sight Sciences, Sun, Surface, TopCon, TearLab Corporation, and Zeiss, outside this work. SH has served as an advisor or investigator for Allergan, Alcon, Avedro, BioTissue/TissueTech, Dompe, Eyevance, EyePoint Medical, Johnson & Johnson, Kala, NuSight Medical, Ocular Therapeutix, Quidel, Shire (a Takeda company), Science Based Health, Sight Sciences, Sun, Tear Solutions, Tear Restore, and TissueTech. The authors declare no other conflicts of interest.
References
[1] American Academy of Ophthalmology Cornea/External Disease Panel. Conjunctivitis PPP – 2023. https://www.aao.org/preferred-practice-pattern/conjunctivitis-ppp-2023. Accessed November 15, 2023.
[2] Azari AA, Barney NP. Conjunctivitis: a systematic review of diagnosis and treatment. JAMA. 2013;310(16):1721-1729. doi:10.1001/jama.2013.280493
[3] McCulloch M, Fan VS, Mandl KD, Kohane IS. Routinely collected data for comparative effectiveness research: the case of conjunctivitis. J Am Med Inform Assoc. 2010;17(1):37-43. doi: 10.1136/jamia.2009.000930.
[4] Lopatka CW, Weber SE, Lopatka EG. Acute conjunctivitis: point-of-care diagnosis and treatment. Clin Optom (Auckl). 2016;8:161-170. doi: 10.2147/OPTO.S91865.
[5] Sheikh A, Hurwitz B, Cave J. Antibiotics for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2012;(8):CD001211. doi: 10.1002/14651858.CD001211.pub3.
[6] O’Brien TP, Seminario-Vidal L, Halstrom S, Salinas C, Protzko EE, Torkildsen G. Impact of rapid point-of-care test for adenoviral conjunctivitis on antibiotic prescribing. JAMA Ophthalmol. 2015;133(10):1102-1108. doi: 10.1001/jamaophthalmol.2015.2441.
[7] Cronau H, Kanaan M, Maier-Wenzel H. Diagnosis and management of red eye in primary care. Am Fam Physician. 2010;81(2):137-144.
[8] Weiss KD, Murchison C. Conjunctivitis. Pediatr Rev. 2014;35(3):111-118; quiz 119. doi: 10.1542/pir.35-3-111.
[9] Rose PW, Mathers J, Gathercole J, Jones L, Hay AD, Little P. Study of patient initiated treatment for acute infective conjunctivitis (PITCH): a randomised controlled trial. BMJ. 2005;331(7527):1183. doi: 10.1136/bmj.331.7527.1183.
[10] Harris P, Melia M, Lawrence D, Kramer MS, Lenton S, Knottnerus JA. Appropriate use of antibiotics for common general practice conditions: the views of general practitioners in the Netherlands, Australia and the UK. Fam Pract. 2006;23(4):414-419. doi: 10.1093/fampra/cml028.
[11] van Weert HC, Pickering JW, van den Broek JM, Bindels PJ, Dekker JH. Accuracy of history taking and physical examination in diagnosing bacterial conjunctivitis: a systematic review of the literature. Br J Gen Pract. 2007;57(539):631-637.
[12] Asbell PA, Collier S, Sahm DF, Shaw M, Draghi DC, ARMOR Study Group. Antibiotic resistance among ocular pathogens in the United States: five-year results from the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) surveillance study. JAMA Ophthalmol. 2015;133(12):1430-1438. doi: 10.1001/jamaophthalmol.2015.3742.
[13] Dave T, O’Brien TP. Antibiotic resistance: reality and implications for ophthalmology. JAMA Ophthalmol. 2015;133(12):1439-1441. doi: 10.1001/jamaophthalmol.2015.3737.
[14] Dell’Anna AM, Ingraham AM, Samore MH, LaPlante KL. Antimicrobial stewardship in outpatient settings: a systematic review. Infect Control Hosp Epidemiol. 2016;37(1):1-12. doi: 10.1017/ice.2015.249.
[15] Uchio E, Ikezawa Z, Ohno S, Aoki K. Clinical features of adenovirus conjunctivitis in patients with and without bacterial co-infection. Jpn J Ophthalmol. 2000;44(4):375-381.
[16] Weiss KS, Gottsch JD. Hyperacute bacterial conjunctivitis. Curr Opin Ophthalmol. 2006;17(4):332-334. doi: 10.1097/01.icu.0000234236.86482.84.
[17] Ta CN, Strelow S, Usner DW, et al. Clinical and economic outcomes of acute bacterial conjunctivitis in patients treated with azithromycin ophthalmic solution 1% or tobramycin ophthalmic solution 0.3%. Clin Ther. 2007;29(8):1777-1785. doi: 10.1016/j.clinthera.2007.08.025.
[18] Friedlaender MH. Conjunctivitis of allergic origin: clinical presentation and differential diagnosis. Surv Ophthalmol. 1993;38 Suppl:105-114.
[19] Hierholzer JC, Tabor E. Human adenovirus types 2, 4, 5, 6, and 7: newly recognized respiratory tract pathogens. J Infect Dis. 1975;131 Suppl:S272-S277.
[20] Jawetz E, Dawson CR, Hanna L, Thygeson P. Adenovirus infections of the eye. Am J Ophthalmol. 1967;63(5):1318-1328.
[21] Welliver RC. Adenovirus infections. In: Feigin RD, Cherry JD, Demmler GJ, Kaplan SL, eds. Textbook of Pediatric Infectious Diseases. 5th ed. Philadelphia, PA: WB Saunders; 2004:2043-2052.
[22] Tsubota K, Satake Y, Ohshima Y, et al. Treatment of epidemic keratoconjunctivitis by removal of pseudomembranes and topical application of cyclosporin A. Cornea. 1993;12(2):125-130.
[23] Laibson PR, Kibrick MS, McCarthy M. Frequency of subepithelial corneal infiltrates in epidemic keratoconjunctivitis. Arch Ophthalmol. 1969;82(1):17-21.
[24] Romanowski EG, Yiin Y, Gordon YJ. Adenoviral conjunctivitis. Curr Opin Ophthalmol. 1996;7(4):32-37.
[25] Chigbu DI, Labugger I, Hofmann-Wellenhof R, et al. High viral load in tear fluid during acute adenoviral keratoconjunctivitis. Invest Ophthalmol Vis Sci. 2008;49(7):2935-2939. doi: 10.1167/iovs.07-1556.
[26] Baum JD, Draelos ZD, Lachapelle J, et al. Povidone-iodine/dexamethasone ophthalmic suspension for acute adenoviral conjunctivitis: a randomized, controlled, phase II trial. J Ocul Pharmacol Ther. 2017;33(7):524-531. doi: 10.1089/jop.2017.0014.
[27] Geffken K, Bräutigam M, Gündling S, et al. N-chlorotaurine eye drops for treatment of adenovirus keratoconjunctivitis: a randomised phase IIb clinical trial. Br J Ophthalmol. 2017;101(11):1479-1484. doi: 10.1136/bjophthalmol-2016-309982.
[28] Sambursky R, Tauber S, Blanchard A, et al. Sensitivity and specificity of AdenoPlus for diagnosing adenoviral conjunctivitis. Ophthalmology. 2007;114(1):8-14. doi: 10.1016/j.ophtha.2006.04.054.
[29] Liesegang TJ. Varicella zoster virus keratitis. Ophthalmology. 1985;92(12):1731-1746.
[30] Marsh RJ, Cooper M, Dukes GE, Maurice DM. Topical acyclovir and adenine arabinoside in the treatment of herpes zoster ophthalmicus. Br J Ophthalmol. 1983;67(10):676-679.
[31] Wiley LA, Kutz WE. Conjunctivitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK543107/.
[32] McDonald M, Protzko EE, McGill J, et al. Besifloxacin ophthalmic suspension 0.6% in methicillin-resistant Staphylococcus aureus conjunctivitis. Ophthalmology. 2012;119(9):1769-1775. doi: 10.1016/j.ophtha.2012.03.047.
[33] Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2019. Atlanta, GA: U.S. Department of Health and Human Services, CDC; 2019. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf. Accessed November 15, 2023.
[34] Centers for Disease Control and Prevention (CDC). Sexually transmitted disease surveillance 2017. Atlanta, GA: U.S. Department of Health and Human Services, CDC; 2018. https://www.cdc.gov/std/stats17/default.htm. Accessed November 15, 2023.
[35] Kreisel KM, Torrone E, Harris N, Weinstock H, Sexually Transmitted Disease Surveillance 2017 Writing Group. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex Transm Dis. 2021;48(4):207-214. doi: 10.1097/OLQ.0000000000001355.
[36] Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1-137.
[37] Centers for Disease Control and Prevention (CDC). Chlamydia – 2017 STD Surveillance Report. https://www.cdc.gov/std/stats17/chlamydia.htm. Accessed November 15, 2023.
[38] Kreisel K, Sparks A, Torrone E, Weinstock H. Trends in chlamydia, gonorrhea, and syphilis in the United States, 2013-2017. Sex Transm Dis. 2020;47(1):1-7. doi: 10.1097/OLQ.0000000000001079.
[39] Bowling B. Kanski’s Clinical Ophthalmology: A Systematic Approach. 9th ed. Philadelphia, PA: Elsevier Saunders; 2020.
[40] Wolffsohn JS, Arita R, Baudouin C, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539-574. doi: 10.1016/j.jtos.2017.05.001.
[41] Clausen ML, Christiansen CB, Hansen A, et al. Rapid diagnostic test for adenoviral conjunctivitis: a prospective study. Acta Ophthalmol. 2016;94(2):e62-e67. doi: 10.1111/aos.12694.
[42] Holtz S, Lausen B, Struyf F, et al. Clinical performance of a rapid antigen test for diagnosing acute adenoviral conjunctivitis. J Clin Virol. 2011;52(3):213-217. doi: 10.1016/j.jcv.2011.07.016.
[43] Pancholi P, Peterson LR, Moody J, Weinstein MP, Massey M, Thomson RB Jr. Multicenter evaluation of Copan ESwab collection and transport system for aerobic and anaerobic bacteria. J Clin Microbiol. 2007;45(11):3521-3525. doi: 10.1128/JCM.01254-07.
[44] Isenberg SJ, Apostolides J, Chasan R, et al. Conjunctivitis in the first month of life. Am J Ophthalmol. 1985;100(3):450-456.
[45] Romanowski EG, Gordon YJ. Update on the adenovirus virucidal activity of cidofovir. Invest Ophthalmol Vis Sci. 2000;41(5):1159-1168.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.