Introduction
In the realm of healthcare, individual care plans, such as a hypothetical “Kenneth Bronson Care Plan Nursing Diagnosis,” are crucial for personalized patient management. However, extending the focus beyond the individual to community-based interventions is increasingly recognized as vital for achieving widespread mental health and social equity. This article delves into recent advancements in community interventions designed to bolster mental health and address social determinants of health, drawing upon a review of literature spanning collaborative care, early psychosis, school-based programs, homelessness, criminal justice, global mental health, and mental health promotion. We aim to provide a comprehensive overview, surpassing previous discussions in depth and SEO optimization for an English-speaking audience interested in the multifaceted nature of mental health support systems.
Multi-sector Collaborative Care: Integrating Community Resources
Collaborative care models, inspired by the Chronic Care Model (CCM), emphasize the integration of health system reforms and community-based resources. While many collaborative care studies have concentrated on embedding mental health services within primary care settings, the significance of community organizations and social services is paramount, especially when addressing inequities. These external resources become indispensable for under-resourced populations and in disaster recovery scenarios, offering support beyond the conventional healthcare sector.
Community Partners in Care (CPIC), a notable depression collaborative care study, engaged 95 programs across five sectors, including primary care, mental health, substance use treatment, homeless services, and community support services. CPIC stood out as a high-quality study evaluating the added value of community engagement in depression care. This group-level randomized study compared Community Engagement and Planning (CEP) with Resources for Services (RS). CEP involved a multi-sector coalition approach, fostering community program participation in psychoeducation and streamlined referrals. CPIC’s community-partnered participatory research approach is well-documented, highlighting its robust community partnerships.
CPIC uniquely focused on an under-resourced racial/ethnic minority sample, enrolling participants with complex comorbidities. At a 6-month follow-up, CEP participants showed significant improvements in health-related quality of life, increased physical activity, reduced homelessness risk factors, and fewer behavioral health hospitalizations compared to RS. While some benefits persisted over time, the most pronounced effects were observed in the initial 6 months.
Since CPIC, few collaborative care studies have incorporated non-healthcare partners. However, Hankerson et al.’s depression screenings in African American mega-churches in New York City, utilizing a community coalition, demonstrated the critical role of faith-based organizations and local government in mental health initiatives. Despite a high rate of moderate depression among screened individuals, none requested mental health referrals, underscoring the importance of churches as accessible sites for mental health support and referral.
Early Intervention Services for Psychosis: Community Outreach and Support
The literature on coordinated specialty care programs for early psychosis, such as RAISE and OnTrackNY, is extensive and growing. Many early psychosis interventions adapt Assertive Community Treatment (ACT), emphasizing outreach-based services within community settings.
The Danish OPUS trial, a two-site RCT of ACT-based early intervention, revealed significant positive outcomes at 2 years, including reduced psychotic symptoms and improved treatment adherence. However, at a 10-year follow-up, these differences largely diminished, suggesting the need for longer-term specialized interventions, booster sessions, or early detection programs to sustain initial gains.
A London Early Intervention Service (EIS) initiative aimed to reduce untreated psychosis duration by engaging 36 community organizations through psychoeducational workshops. Despite improved attitudes toward EIS referrals among community staff, the study showed no significant reduction in untreated psychosis duration and, unexpectedly, a less streamlined referral process. Interviews highlighted barriers such as mental health stigma, staff turnover, and resistance from EIS clinic staff to community-based work, reinforcing the need for sustained resources and addressing systemic challenges.
School-Based Interventions: Accessible Mental Healthcare for Youth
Schools are critical sites for delivering mental healthcare to youth, particularly under-resourced youth who face barriers to community mental health services. School infrastructures facilitate large-scale prevention interventions. Successful implementation, however, requires consideration of policies, school culture, and leadership.
Skryabina et al.’s RCT assessed educational outcomes of the FRIENDS program, a universal school-based cognitive behavioral therapy prevention program. Health-led FRIENDS was more effective in reducing anxiety scores compared to school-led FRIENDS and standard health education. However, no intervention effects were observed on standardized academic test scores.
Studies in pre-kindergarten years demonstrate the importance of early intervention. An evaluation of an enriched Head Start Curriculum revealed that children in the Head Start REDI intervention showed significantly better developmental trajectories in social behavior and learning engagement over a 5-year period. These findings highlight the value of interventions at the classroom and whole-school levels.
Homeless Services: Housing First and Integrated Support
Individuals experiencing homelessness face heightened risks of mental illness and reduced life expectancy. The Housing First model, providing permanent housing without preconditions like sobriety, has gained prominence. Studies show Housing First leads to quicker and more sustained housing retention compared to traditional continuum housing approaches.
The Canadian At Home/Chez Moi study, a multi-city RCT, demonstrated that Housing First participants entered housing more quickly, retained housing longer, and reported higher housing quality at 2-year follow-up, alongside improved community functioning and quality of life.
Family-focused studies on homelessness also provide valuable insights. Nath’s study in New Delhi found that drop-in homeless service centers for children were associated with fewer ill health outcomes and reduced substance use. Shinn et al.’s study on newly homeless families showed that a family-adapted critical time intervention improved outcomes for children, particularly reducing school troubles at 24-month follow-up. Future research should further explore broader social outcomes relevant to individuals who have experienced homelessness.
Criminal Justice: Diverting and Supporting Justice-Involved Individuals
A significant proportion of jail and prison inmates have a history of mental illness. Community interventions collaborating with the criminal justice system are crucial for addressing health disparities in this population.
In Monroe County, New York, a study compared Forensic Assertive Community Treatment (FACT) with usual treatment for adults with psychotic disorders charged with misdemeanors. FACT, adapted from ACT with criminal justice system collaboration, resulted in significantly fewer convictions and days in jail, and more days in outpatient mental health treatment over a year.
A pilot study examined a social worker-administered decision-making intervention for police encounters with individuals with mental illness. Linkage specialists provided mental health history and referral options to police officers, showing promise for reducing arrests in this population through cross-sector collaboration.
Interventions addressing recidivism risk factors, such as healthcare access and unemployment, are also vital. Studies on expedited Medicaid enrollment for recent prison releasees demonstrated reduced recidivism and increased service utilization, highlighting the impact of healthcare access on justice outcomes.
Global Mental Health: Lay Health Workers and Community-Based Solutions
Global mental health prioritizes health improvement and equity worldwide. Lay health worker (LHW) interventions are prominent in this field, increasing service demand, mental health literacy, and service supply in under-resourced areas.
Patel et al.’s RCT in India demonstrated the effectiveness of the Healthy Activity Program (HAP), a psychological intervention for depression delivered by LHWs in primary care. HAP participants showed significantly reduced depression symptoms and improved functioning compared to enhanced usual care.
A study in South Africa examined a child abuse prevention program for adolescents delivered by local childcare workers. The intervention yielded significant improvements in social outcomes, including reduced child abuse and improved caregiver mental health.
Research on the impact of war and structural forces on mental health underscores the need for community-based interventions to address broad societal challenges. Cilliers et al.’s study on truth and reconciliation commissions (TRCs) in Sierra Leone found that while TRCs improved societal healing, they worsened individuals’ psychological health, suggesting the need for integrated counseling and alternative post-conflict unification methods.
Mental Health Promotion and Prevention: Community-Level Systems
Communities That Care (CTC) is a community-level prevention system focusing on youth substance use, violence, and delinquency, with secondary foci on mental health outcomes. CTC involves community coalitions, risk and protective factor assessment, action planning, and evidence-based program implementation. The Community Youth Development Study, a community-randomized study of CTC, showed improved individual outcomes in CTC communities, including reduced substance use and delinquency, with some effects persisting into adulthood.
Long-term follow-up of the Community Youth Development Study at age 21 revealed that CTC communities showed increased lifetime abstinence from substance use and antisocial behavior, and decreased lifetime incidence of violence.
Social protection studies investigating the effects of direct resource provision, such as cash and food transfers, on mental health and social outcomes demonstrate the impact of addressing social inequities. An RCT in Ecuador showed that cash and food transfers significantly reduced intimate partner violence. Similar studies on cash transfers in Kenya and urban greening initiatives have shown improvements in depression outcomes, highlighting the crucial link between social determinants and mental health.
Discussion: Actions of Community Interventions by Social-Ecological Level
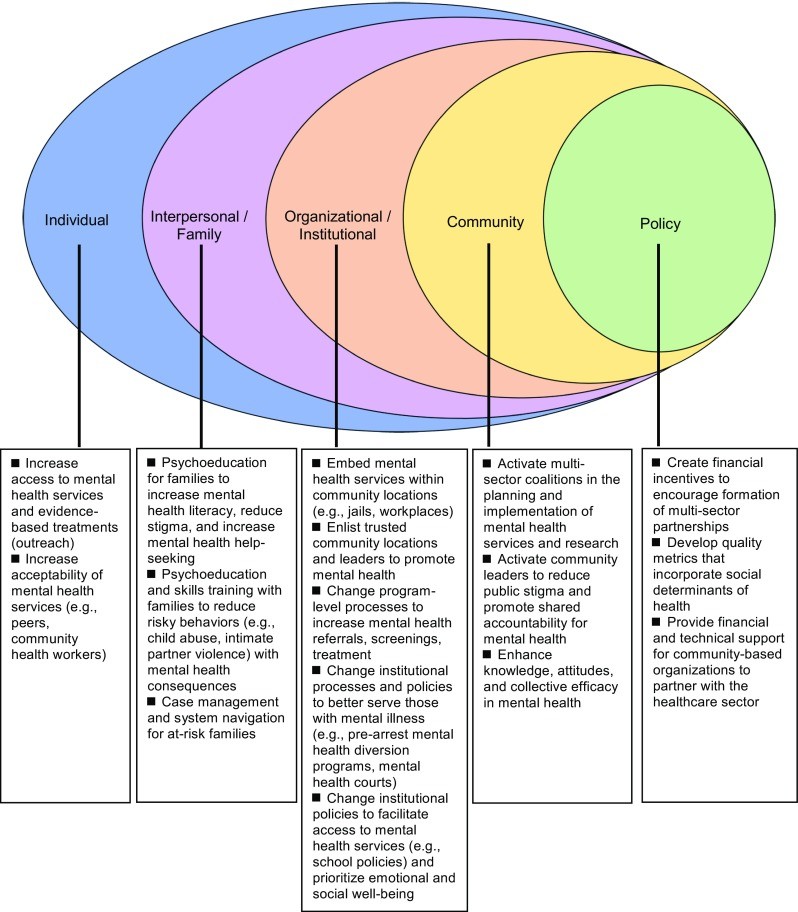 Fig. 1
Fig. 1
Overview of community intervention processes by social-ecological level, adapted from McElroy et al., illustrating the multi-layered approach to health promotion.
Community interventions operate across social-ecological levels: individual, interpersonal/family, organizational/institutional, community, and policy. Most interventions reviewed focus on individual-level changes, often simultaneously acting at organizational/institutional levels. Lay health worker interventions and adapted treatment models exemplify individual-level strategies, while school-based programs and professional development for teachers represent organizational/institutional actions.
Interpersonal-level interventions, such as parent and family programs, and organizational/institutional interventions, like depression screenings in churches and school-based prevention programs, are also prevalent. Fewer studies intervene at the whole community level. CPIC and CTC are notable examples of community-level interventions, alongside resource provision through cash/food transfers and land revitalization efforts.
Policy interventions, while beyond the scope of this review, are crucial for promoting mental health equity. Policies supporting multi-sector health collaborations and nation-level efforts to promote mental and social well-being, such as Thrive NYC, demonstrate the potential of policy-level actions.
Ethical Considerations in Community Interventions
Ethical considerations are paramount in community interventions, particularly when working with marginalized populations. Building trust, recognizing structural forces, and equitable community stakeholder involvement are essential. Community-based organizations, social services, and healthcare agencies require sustained funding and infrastructure to ensure equitable partnerships and intervention sustainability.
Conclusions: Towards Sustainable and Equitable Community Mental Health
Community interventions demonstrate effectiveness across various topic areas and social-ecological levels. Lay health worker programs, parenting interventions, school-based prevention, adapted ACT models, Housing First, and multi-sector collaborative care exemplify successful approaches. Sustaining long-term outcomes requires ongoing resources, training, and policy reforms supporting healthcare-community partnerships. Future research should refine best practices for multi-sector collaborations, ensure sustainable change beyond research periods, and identify optimal community intervention strategies for specific health and social challenges. By fostering equitable partnerships and addressing social and structural inequities, community interventions can significantly improve mental health and achieve large-scale social well-being.
Electronic supplementary material
ESM 1 (DOCX 24 kb)
ESM 2 (DOCX 104 kb)