I. Introduction: Navigating Respiratory Distress in COPD within Urgent Care Settings
Chronic Obstructive Pulmonary Disease (COPD) is frequently characterized by acute exacerbations marked by worsening dyspnea, often accompanied by increased coughing, sputum production, and changes in sputum consistency. These exacerbations of COPD (ECOPDs) significantly diminish a patient’s quality of life, accelerate the decline of lung function, and elevate the risk of hospitalization. Alarmingly, a substantial proportion of patients, nearly 20%, are readmitted to the hospital within just 30 days post-discharge, imposing a considerable burden on both individuals and healthcare systems. The prognosis for patients hospitalized for ECOPD is grim, with mortality rates reaching approximately 25% within one year and 65% within five years.
COPD patients are typically older and often present with multiple co-existing chronic conditions such as heart failure, coronary artery disease, arrhythmias, interstitial lung diseases, bronchiectasis, and mental health disorders like anxiety and depression. Furthermore, they are at an elevated risk for developing pneumonia, pulmonary embolism (PE), and pneumothorax. These comorbidities not only amplify the likelihood of subsequent ECOPDs but can also mimic or exacerbate their symptoms, creating diagnostic challenges, particularly in urgent care settings where rapid and accurate assessment is crucial. Notably, a significant proportion of readmissions following ECOPD hospitalization, around 70%, are attributed to the decompensation of these underlying comorbidities rather than the COPD itself.
This underscores the critical need for healthcare providers in urgent care and emergency settings to consider a broad differential diagnosis when COPD patients present with worsening respiratory symptoms, especially dyspnea, but lack the typical indicators of an ECOPD. A systematic approach, incorporating a thorough clinical evaluation and targeted investigations, is paramount to accurately identify and effectively manage these mimicking conditions. This article provides a practical guide to navigating the Urgent Care Differential Diagnosis of respiratory distress in COPD patients, aiming to improve patient outcomes and reduce the healthcare costs associated with misdiagnosis and readmissions.
II. Initial Assessment: The CASE Approach in Urgent Care
In the urgent care setting, a rapid yet comprehensive initial evaluation is crucial for patients with COPD presenting with respiratory symptoms. The CASE approach provides a structured framework for this initial assessment:
Complete Clinical Picture
A thorough clinical assessment is the cornerstone of differential diagnosis in urgent care. This involves:
- Detailed History: Obtain a comprehensive medical history, focusing on the patient’s COPD diagnosis, usual symptom patterns, and any known comorbidities. Crucially, inquire about the current episode:
- Symptom Onset and Progression: How quickly did the symptoms worsen? Are they acute or gradual?
- Symptom Profile: Beyond dyspnea, are there changes in cough, sputum volume, or sputum color? Note any presence of chest pain, palpitations, lower extremity swelling, or fever.
- Exacerbating Factors: Identify potential triggers such as infections, environmental exposures, or medication non-adherence.
- Comorbidity History: Specifically probe for a history of heart failure, ischemic heart disease, arrhythmias, thromboembolic events, or other conditions that can mimic ECOPD.
- Physical Examination: A focused physical exam in urgent care should include:
- Vital Signs: Assess respiratory rate, heart rate, blood pressure, oxygen saturation, and temperature. Tachypnea, tachycardia, or fever can point towards alternative diagnoses.
- Respiratory Examination: Evaluate breath sounds for wheezing, crackles, or diminished breath sounds. Note the presence of accessory muscle use, indicating respiratory distress.
- Cardiovascular Examination: Check for jugular venous distension, peripheral edema, and heart sounds (murmurs, gallops). Irregular pulse should raise suspicion for arrhythmias.
- General Examination: Briefly assess for signs of infection, anemia (pallor), or other systemic illnesses.
Assess Symptoms and Signs
Quantifying the severity of symptoms and objectively documenting clinical signs is essential for guiding urgent care differential diagnosis:
- Dyspnea Severity: Utilize a dyspnea scale (e.g., visual analog scale) to quantify the patient’s subjective experience of breathlessness. Changes from baseline are particularly important.
- Cough and Sputum: Document the presence, frequency, and characteristics of cough. Note the volume, color, and consistency of sputum. Purulent sputum may suggest infection but is not specific to bacterial ECOPD or pneumonia.
- Pain Assessment: Inquire about chest pain or discomfort, noting its location, character (pleuritic, ischemic), and radiation. Pleuritic chest pain is less typical of ECOPD and more suggestive of pulmonary embolism or pleurisy.
- Objective Signs: Document tachypnea, tachycardia, presence of arrhythmias, fever, sputum characteristics, respiratory distress signs, and findings from chest auscultation and general physical exam.
Severity Evaluation
Determining the severity of the respiratory event is crucial for urgent care triage and diagnostic pathways:
- Pulse Oximetry: Measure oxygen saturation (SpO2) to assess hypoxemia.
- Point-of-Care Testing (if available and rapidly accessible in urgent care):
- C-Reactive Protein (CRP): Elevated CRP levels may suggest infection or inflammation, but are not specific.
- Arterial Blood Gases (ABGs): If severe respiratory distress is present, ABGs can assess for hypercapnia and hypoxemia, guiding immediate management.
- Electrocardiogram (ECG): Rapid ECG can identify arrhythmias or signs of acute myocardial ischemia, especially if chest pain is present.
- Chest X-ray: Portable chest X-ray in urgent care can help identify pneumonia, pneumothorax, or heart failure, but may not be immediately available or interpretable in all settings.
Establish Potential Cause
Based on the initial assessment, formulate a preliminary differential diagnosis and consider potential causes for the patient’s worsening respiratory symptoms:
- ECOPD: Is this a typical exacerbation of COPD? Are the symptoms and signs consistent with the patient’s usual exacerbation pattern?
- Infection: Pneumonia, bronchitis, or viral respiratory infections should be considered, especially if fever, purulent sputum, or signs of consolidation are present.
- Cardiovascular Events: Acute heart failure, myocardial ischemia, and arrhythmias are critical considerations, particularly in older COPD patients with cardiac risk factors.
- Pulmonary Embolism: Consider PE if there’s acute worsening of dyspnea, pleuritic chest pain, risk factors for thromboembolism, or unexplained hypoxemia.
- Pneumothorax: Suspect pneumothorax in patients with sudden onset dyspnea and pleuritic chest pain, especially those with emphysema or bullous lung disease.
- Other Mimics: Consider asthma exacerbation, interstitial lung disease exacerbation, anxiety/panic attacks, or pleural effusion.
By systematically applying the CASE approach in urgent care, clinicians can efficiently gather crucial information to guide the differential diagnosis of respiratory distress in COPD patients and initiate appropriate investigations and management strategies.
III. Cardiovascular Conditions Mimicking ECOPD in Urgent Care
Cardiovascular diseases frequently overlap with COPD and can present with symptoms that closely resemble ECOPDs, posing significant challenges in urgent care differential diagnosis.
A. Acute Heart Failure (AHF)
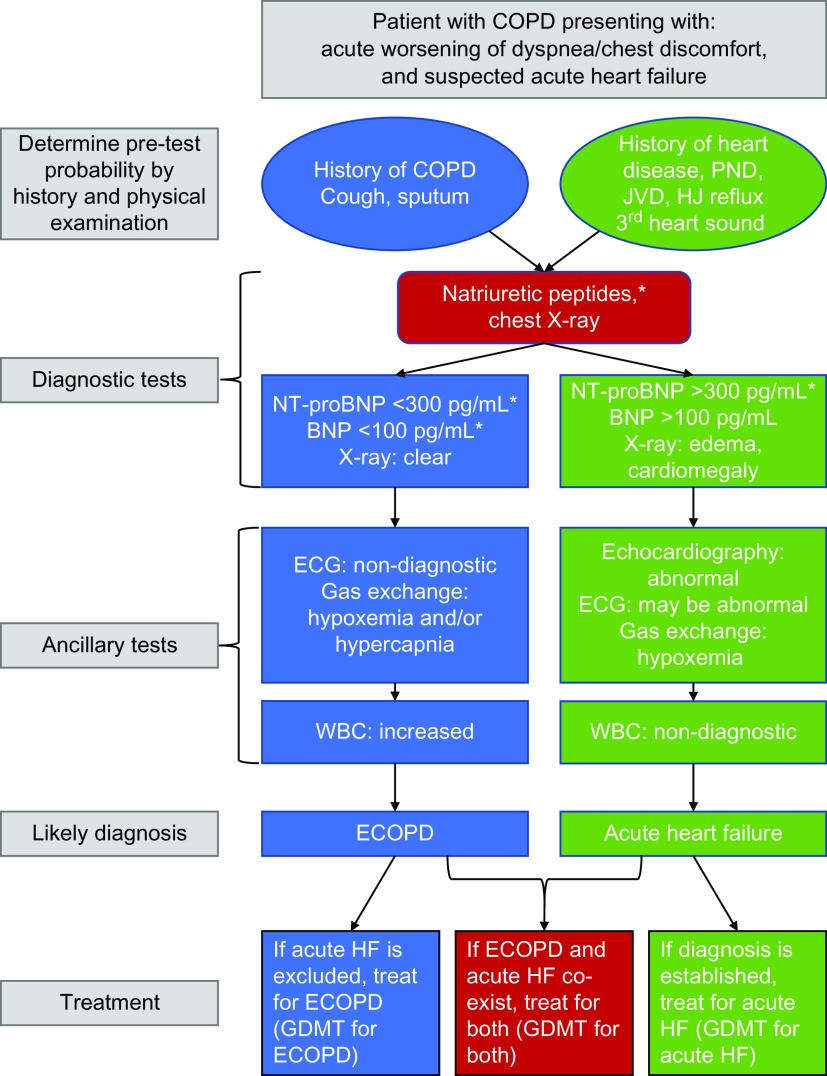
Distinguishing between ECOPD and AHF can be particularly difficult in urgent care as both conditions share common symptoms like dyspnea. Key differentiating features and urgent care diagnostic steps include:
- Clinical Clues Suggesting AHF:
- Dyspnea at Rest or Orthopnea: Dyspnea worsening when lying down is more typical of AHF.
- Fluid Retention Signs: Peripheral edema, jugular venous distension (JVD), and pulmonary congestion (crackles) strongly suggest AHF.
- Chest Pain/Discomfort: While less specific, chest discomfort can be present in both AHF and myocardial ischemia.
- History of Heart Failure: A known history of HF significantly raises suspicion for AHF.
- Urgent Care Diagnostic Approach for Suspected AHF:
- Rapid Physical Exam Focus: Prioritize assessment for JVD, pulmonary crackles, and peripheral edema.
- ECG: Immediately obtain an ECG to rule out acute myocardial ischemia and assess for arrhythmias.
- Chest X-ray (if rapidly available): Look for cardiomegaly and pulmonary edema patterns suggestive of AHF.
- Point-of-Care Natriuretic Peptides (BNP or NT-proBNP) (if available): Elevated levels strongly support AHF, but interpretation in the context of COPD requires caution as COPD itself can elevate BNP. Very low BNP/NT-proBNP can help rule out AHF.
- Consider Point-of-Care Ultrasound (POCUS) (if expertise and equipment are available): POCUS can rapidly assess for B-lines (pulmonary edema) and cardiac function, aiding in differentiating AHF from ECOPD.
Differentiating AHF from ECOPD in urgent care requires careful integration of clinical findings, rapid ECG, chest X-ray (if feasible), and potentially point-of-care biomarkers and POCUS, if available, to guide immediate management.
B. Ischemic Heart Disease (IHD) and Arrhythmias
Myocardial ischemia and arrhythmias are common in COPD patients and can exacerbate respiratory symptoms or present as acute dyspnea, mimicking ECOPD.
- Clinical Clues Suggesting IHD/Arrhythmias:
- Chest Pain/Discomfort: Anginal chest pain, pressure, or tightness should prompt evaluation for myocardial ischemia.
- Palpitations or Irregular Pulse: Suggestive of arrhythmias, particularly atrial fibrillation.
- Risk Factors for IHD: Hypertension, hyperlipidemia, smoking, diabetes increase the likelihood of IHD.
- ECG Abnormalities: New ST-segment changes, T-wave inversions, or arrhythmias on ECG are highly suggestive.
- Urgent Care Diagnostic Approach for Suspected IHD/Arrhythmias:
- ECG: Immediate ECG is mandatory for patients with chest pain or suspected arrhythmias.
- Cardiac Monitoring: Continuous cardiac monitoring may be warranted in patients with palpitations or ECG abnormalities.
- Troponin (if IHD suspected): Point-of-care troponin testing can help rule in or rule out acute myocardial infarction, especially in patients with chest pain or ECG changes.
Rapid ECG and cardiac biomarker testing are essential in urgent care to promptly identify and manage cardiac conditions that may be mimicking or complicating respiratory symptoms in COPD patients.
C. Pulmonary Embolism (PE)
PE is a life-threatening condition that can present with acute dyspnea and chest pain, easily confused with ECOPD in urgent care.
- Clinical Clues Suggesting PE:
- Sudden Onset Dyspnea: Abrupt worsening of breathlessness without typical ECOPD triggers.
- Pleuritic Chest Pain: Sharp chest pain worsened by breathing is more typical of PE than ECOPD.
- Hemoptysis: Coughing up blood, though less common, is more suggestive of PE.
- Risk Factors for PE: Immobility, recent surgery, malignancy, prior venous thromboembolism, hypercoagulable states increase PE risk.
- Signs of Deep Vein Thrombosis (DVT): Leg swelling, pain, or tenderness can suggest DVT, a source of PE.
- Urgent Care Diagnostic Approach for Suspected PE:
- Risk Stratification: Utilize clinical scoring systems like the Geneva or Wells score to assess pretest probability of PE.
- D-dimer Testing: In patients with low to intermediate pretest probability, a negative D-dimer can help rule out PE. However, D-dimer can be elevated in ECOPD and other conditions, reducing its specificity.
- Computed Tomography Pulmonary Angiography (CTPA): CTPA is the definitive imaging test for PE. Consider CTPA in urgent care if PE is suspected based on clinical probability and D-dimer results, or if clinical suspicion is high regardless of D-dimer.
- Lower Extremity Ultrasound (CUS): If CTPA is contraindicated or unavailable, or if DVT is suspected, CUS can help identify DVT, supporting a diagnosis of venous thromboembolism.
Promptly considering and investigating PE in COPD patients presenting with acute respiratory distress is critical in urgent care to avoid potentially fatal delays in diagnosis and treatment.
IV. Infectious Diseases in the Urgent Care Differential
Infections, particularly pneumonia, are frequent in COPD patients and can mimic or trigger ECOPDs. Differentiating pneumonia from ECOPD is vital for appropriate urgent care management.
A. Pneumonia
Pneumonia and ECOPD share overlapping symptoms, but key clinical and diagnostic features can aid in differentiation in urgent care.
- Clinical Clues Suggesting Pneumonia:
- Fever and Chills: More common in pneumonia than uncomplicated ECOPD.
- Focal Chest Findings: Localized crackles, bronchial breath sounds, or dullness to percussion on chest exam are suggestive of consolidation in pneumonia.
- Purulent Sputum: While present in both, copious purulent sputum may be more prominent in bacterial pneumonia.
- Elevated White Blood Cell Count (WBC) and CRP: Inflammatory markers tend to be higher in pneumonia.
- Urgent Care Diagnostic Approach for Suspected Pneumonia:
- Chest X-ray: Chest X-ray is crucial to identify pulmonary infiltrates consistent with pneumonia. In urgent care, portable chest X-ray may be the most readily available option.
- CRP and WBC Count: Point-of-care CRP and WBC count can provide rapid information to support or refute pneumonia diagnosis.
- Sputum Gram Stain and Culture (if feasible): If sputum is productive and pneumonia is suspected, consider sending sputum for Gram stain and culture, though results will not be immediately available in urgent care.
- Rapid Respiratory Viral Panel (if available): In certain seasons or outbreaks, rapid testing for influenza, RSV, or COVID-19 may be relevant, especially as specific antiviral treatments exist.
Prompt diagnosis of pneumonia in COPD patients presenting to urgent care is essential to initiate appropriate antibiotic therapy and improve outcomes.
B. Bronchiectasis
Bronchiectasis, characterized by chronic airway dilation, frequently coexists with COPD and can complicate the clinical picture in urgent care.
- Clinical Clues Suggesting Bronchiectasis:
- Chronic Productive Cough: Daily cough with sputum production, often mucopurulent, is a hallmark of bronchiectasis.
- History of Recurrent Respiratory Infections: Bronchiectasis predisposes to frequent infections.
- High-Resolution CT (HRCT) Scan History: If available, prior HRCT demonstrating bronchiectasis is highly suggestive.
- Urgent Care Considerations for Bronchiectasis:
- Consider in Frequent Exacerbators: In COPD patients with unusually frequent or severe exacerbations, consider bronchiectasis as a contributing factor.
- Sputum Culture: Sputum culture may identify chronic bacterial colonization, such as Pseudomonas aeruginosa, which can guide antibiotic selection in exacerbations.
- HRCT Scan (if not previously performed): If bronchiectasis is suspected but not confirmed, consider referral for outpatient HRCT scan to establish the diagnosis.
While bronchiectasis is a chronic condition, recognizing its presence in COPD patients presenting to urgent care can influence management strategies, particularly regarding antibiotic selection and long-term respiratory care.
V. Other Conditions in the Urgent Care Differential
Beyond cardiovascular and infectious etiologies, several other conditions can mimic ECOPD in urgent care.
A. Asthma Exacerbation
Overlap between asthma and COPD can make differentiating exacerbations challenging, especially in urgent care.
- Clinical Clues Suggesting Asthma Exacerbation:
- Younger Age of Onset: Asthma typically starts earlier in life than COPD.
- History of Asthma or Atopy: Personal or family history of asthma, allergies, or eczema raises suspicion for asthma.
- Variable Symptoms: Asthma symptoms often exhibit greater diurnal variability and are triggered by allergens or irritants.
- Reversible Airflow Obstruction: Asthma is characterized by more reversible airflow obstruction compared to COPD. However, this is not easily assessed in the urgent care setting.
- Urgent Care Management Considerations for Asthma-COPD Overlap:
- Bronchodilator Responsiveness: Asthma exacerbations often show a more pronounced response to bronchodilators.
- Corticosteroids: Systemic corticosteroids are a mainstay of treatment for both asthma and COPD exacerbations.
- Consider Asthma if Atypical Presentation: If the clinical presentation is atypical for COPD exacerbation or suggests a strong allergic component, consider asthma exacerbation, particularly in younger patients.
B. Interstitial Lung Disease (ILD) Exacerbation
ILDs, such as idiopathic pulmonary fibrosis (IPF), can coexist with COPD and present with acute respiratory worsening.
- Clinical Clues Suggesting ILD Exacerbation:
- Dry Cough Predominance: Cough in ILD is often dry and nonproductive.
- Fine Inspiratory Crackles: Bibasilar fine crackles on auscultation may be more prominent in ILD.
- Prior ILD Diagnosis: Known history of ILD is a critical clue.
- HRCT Scan History: Prior HRCT demonstrating ILD patterns is highly suggestive.
- Urgent Care Considerations for ILD Exacerbation:
- Limited Specific Urgent Care Treatment: Urgent care management of ILD exacerbation is largely supportive.
- Focus on Oxygenation and Supportive Care: Ensure adequate oxygenation and manage symptoms.
- Consider Specialist Consultation: Urgent care may need to consult with or refer to pulmonology for further management of suspected ILD exacerbation.
C. Anxiety and Panic Attacks
Anxiety and panic disorders are common in COPD and can manifest with acute dyspnea, mimicking ECOPD.
- Clinical Clues Suggesting Anxiety/Panic:
- Rapid Onset of Dyspnea: Sudden onset of breathlessness often associated with panic attacks.
- Absence of Typical ECOPD Features: Lack of increased cough, sputum production, or purulence.
- Hyperventilation Symptoms: Lightheadedness, dizziness, tingling, or carpopedal spasms due to hyperventilation.
- History of Anxiety/Panic Disorder: Known history of anxiety or panic attacks is a significant risk factor.
- Urgent Care Approach for Suspected Anxiety/Panic:
- Rule Out Organic Causes First: Exclude other serious conditions (cardiac, pulmonary) before attributing dyspnea to anxiety.
- Clinical Assessment for Panic Symptoms: Inquire about associated anxiety symptoms, triggers, and prior panic episodes.
- Reassurance and Breathing Techniques: Provide reassurance and guide the patient in slow, controlled breathing techniques.
- Consider Anxiolytics (judiciously): In selected cases, short-acting anxiolytics may be considered, but use cautiously in COPD patients, especially with hypercapnia risk.
D. Pneumothorax and Pleural Effusion
Pneumothorax and large pleural effusions can cause acute dyspnea in COPD patients.
- Clinical Clues Suggesting Pneumothorax:
- Sudden Onset Pleuritic Chest Pain and Dyspnea: Abrupt onset of chest pain and breathlessness, often unilateral.
- Decreased Breath Sounds: Unilateral diminished or absent breath sounds on auscultation.
- Hyperresonance to Percussion: Increased resonance on percussion of the affected hemithorax.
- Risk Factors: Bullous emphysema, tall thin males are at higher risk.
- Clinical Clues Suggesting Pleural Effusion:
- Progressive Dyspnea: Gradual worsening of breathlessness.
- Dullness to Percussion: Dullness on percussion over the effusion.
- Decreased or Absent Breath Sounds: Diminished breath sounds over the effusion.
- Underlying Conditions: Consider heart failure, pneumonia, malignancy as potential causes of pleural effusion.
- Urgent Care Diagnostic Approach for Pneumothorax/Pleural Effusion:
- Chest X-ray: Chest X-ray is diagnostic for pneumothorax and can detect significant pleural effusions.
- Lung Ultrasound (POCUS): POCUS can rapidly identify pneumothorax and pleural effusions, especially in settings where chest X-ray is delayed or less accessible.
Rapid recognition of pneumothorax or large pleural effusion is crucial in urgent care as both require specific interventions.
E. Anemia
Anemia, while not a primary mimic of ECOPD, can exacerbate dyspnea in COPD patients.
- Clinical Clues Suggesting Anemia:
- Fatigue and Weakness: Generalized fatigue and weakness accompanying dyspnea.
- Pallor: Pale skin and mucous membranes suggesting anemia.
- Tachycardia: Heart rate may be elevated to compensate for reduced oxygen-carrying capacity.
- History of Anemia or Chronic Disease: Known anemia or underlying chronic conditions predispose to anemia.
- Urgent Care Considerations for Anemia:
- Hemoglobin/Hematocrit Testing: Point-of-care hemoglobin testing can rapidly assess for anemia.
- Consider as Contributing Factor: Recognize anemia as a potential contributor to dyspnea in COPD patients.
- Outpatient Follow-up: Address underlying causes of anemia in outpatient follow-up.
VI. Conclusion: Enhancing Urgent Care Differential Diagnosis for COPD Respiratory Distress
Effectively differentiating ECOPDs from other conditions presenting with similar respiratory symptoms is paramount in the urgent care setting. A systematic approach, employing the CASE framework, coupled with targeted investigations based on clinical suspicion, is essential for accurate and timely diagnosis. By diligently considering the broad differential diagnosis – encompassing cardiovascular diseases, infections, asthma, ILD, anxiety, pneumothorax, pleural effusion, and anemia – urgent care clinicians can significantly improve the management of COPD patients presenting with respiratory distress. This refined diagnostic approach not only optimizes individual patient care but also contributes to reducing hospital readmissions and the overall healthcare burden associated with COPD exacerbations and their mimics. The emphasis on urgent care differential diagnosis is not just about excluding ECOPD, but about proactively identifying and addressing the true underlying cause of respiratory distress, leading to more effective and patient-centered care.
References
References from the original article can be included here. (For brevity and focus on content generation as per instructions, the specific references are not copied here, but would be included in a final, complete article).