Nursing diagnosis is a cornerstone of effective patient care. It’s the critical step that bridges assessment and intervention, ensuring that nursing care plans are truly patient-centered and address their unique needs. This guide will provide a comprehensive understanding of how to make a diagnosis in a nursing care plan, enhancing your skills in critical thinking and patient management.
Understanding Nursing Diagnosis: The Foundation of Your Care Plan
A nursing diagnosis is defined as a clinical judgment about individual, family, group, or community responses to actual or potential health problems and life processes. It’s a statement that describes a patient’s health condition from a nursing perspective, identifying areas where nurses can independently intervene. This diagnosis forms the very basis for selecting specific nursing interventions aimed at achieving measurable patient outcomes, for which nurses are accountable. Nursing diagnoses are derived from a thorough nursing assessment, where patient data is collected and analyzed to pinpoint health issues and needs that fall within the nursing scope of practice. Ultimately, a well-formulated nursing diagnosis is the bedrock upon which a successful nursing care plan is built.
Why is Nursing Diagnosis Essential in Care Planning?
Nursing diagnoses serve several crucial purposes, making them indispensable in healthcare:
- Sharpening Critical Thinking for Nursing Students: For those learning the profession, nursing diagnoses are invaluable tools for developing problem-solving and critical thinking abilities. The process of analysis and diagnosis fosters analytical skills essential for effective nursing practice.
- Prioritizing Nursing Care: Nursing diagnoses directly inform the prioritization of care. By clearly identifying patient problems, nurses can effectively direct nursing interventions to address the most urgent and relevant needs first.
- Meeting Quality Assurance and Payer Requirements: In today’s healthcare landscape, demonstrating the value and effectiveness of care is paramount. Nursing diagnoses facilitate the formulation of expected outcomes, which are vital for meeting quality assurance standards and the requirements of third-party payers.
- Focusing on Patient Responses and Strengths: Nursing diagnoses are unique in their focus on how patients respond to health challenges. They go beyond the disease itself to consider the patient’s holistic experience, including their strengths and resources that can be leveraged for problem resolution and prevention.
- Facilitating Communication within the Healthcare Team: Nursing diagnoses provide a standardized language for communication among nurses and the broader healthcare team. This common language ensures clarity and mutual understanding, promoting effective collaboration in patient care.
- Evaluating Nursing Care Effectiveness and Cost-Efficiency: By establishing clear diagnoses and related outcomes, nursing practice can be evaluated for its effectiveness. Nursing diagnoses provide a framework to determine if the care provided was beneficial to the patient and delivered in a cost-effective manner.
Nursing Diagnosis vs. Medical Diagnosis vs. Collaborative Problems: Key Differences
It’s crucial to distinguish nursing diagnoses from other related concepts in healthcare:
Nursing Diagnosis: This is the nurse’s clinical judgment about the patient’s response to health conditions. It focuses on the patient’s needs and problems that nurses can address through independent nursing actions. For example, a patient experiencing anxiety due to hospitalization would receive a nursing diagnosis of “Anxiety related to unfamiliar hospital environment as evidenced by restlessness and verbalization of fear.” Nursing diagnoses are patient-centered and care-focused.
Medical Diagnosis: This is made by a physician or advanced practitioner and identifies a disease, pathology, or medical condition. Medical diagnoses are disease-focused and guide medical treatment. Examples include Diabetes Mellitus, Pneumonia, or Fractured Femur. Nurses implement physician-prescribed treatments related to medical diagnoses.
Collaborative Problems: These are potential or actual health complications that require both medical and nursing interventions. Nurses monitor for and manage collaborative problems using both independent nursing actions and physician-prescribed interventions. An example is “Potential Complication: Hypoglycemia” in a patient with diabetes. Here, nurses monitor blood glucose levels (nursing action) and may administer prescribed insulin (medical order).
The key distinction is that nursing diagnoses focus on the patient’s response to health issues and are addressed through nursing care, while medical diagnoses identify the disease itself and are treated medically. Collaborative problems bridge both, requiring shared management.
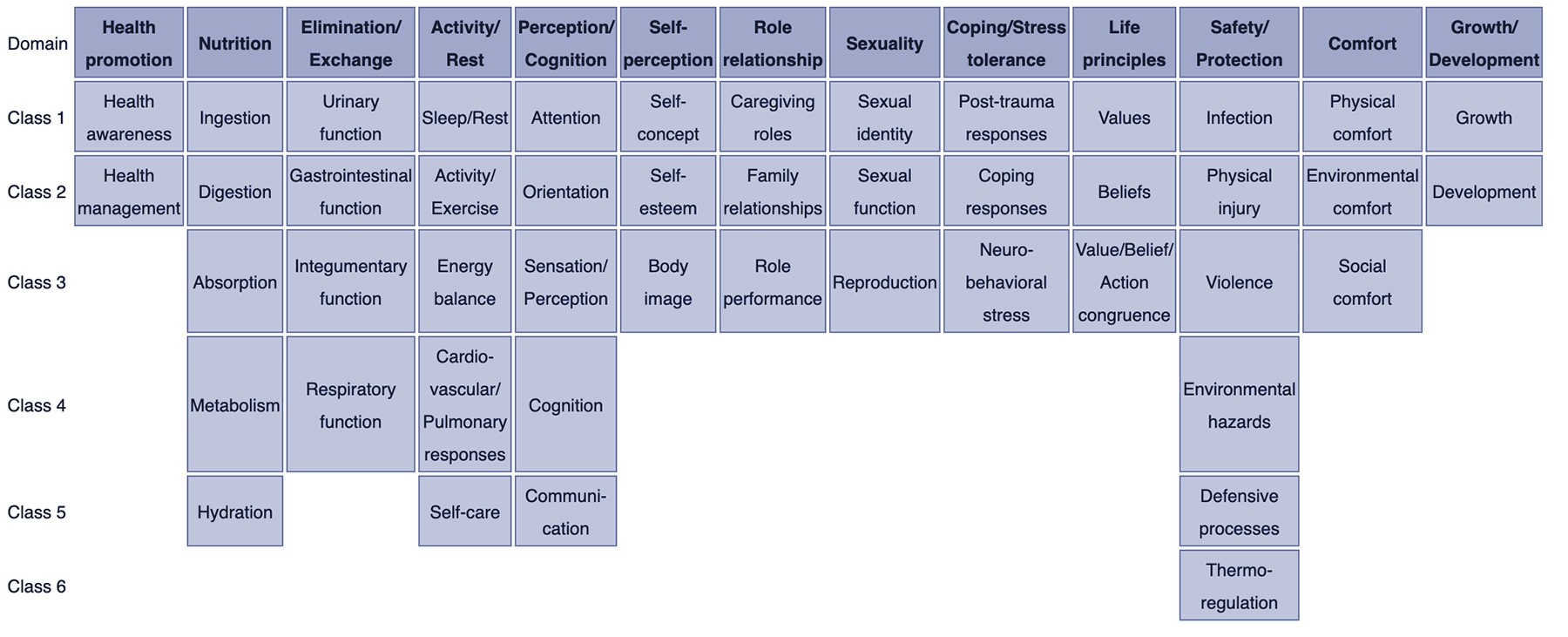
Classifying Nursing Diagnoses: Taxonomy II
To standardize and organize nursing diagnoses, the Taxonomy II system was developed, based on Dr. Mary Joy Gordon’s Functional Health Patterns. This system provides a hierarchical structure for classifying diagnoses:
- Domains (13): Broad categories of human health and functioning (e.g., Health Promotion, Nutrition, Activity/Rest).
- Classes (47): Subcategories within domains, providing more specific groupings (e.g., within Nutrition Domain: Ingestion, Digestion, Metabolism).
- Nursing Diagnoses: Specific, standardized labels for patient health problems, categorized within domains and classes.
Taxonomy II uses a multi-axial system for coding diagnoses, considering factors like diagnostic concept, time, unit of care, age, health status, and descriptors. Diagnoses are listed alphabetically by concept for easy retrieval.
Domains and Classes within Nursing Diagnosis Taxonomy II:
- Domain 1: Health Promotion
- Class 1: Health Awareness
- Class 2: Health Management
- Domain 2: Nutrition
- Class 1: Ingestion
- Class 2: Digestion
- Class 3: Absorption
- Class 4: Metabolism
- Class 5: Hydration
- Domain 3: Elimination and Exchange
- Class 1: Urinary Function
- Class 2: Gastrointestinal Function
- Class 3: Integumentary Function
- Class 4: Respiratory Function
- Domain 4: Activity/Rest
- Class 1: Sleep/Rest
- Class 2: Activity/Exercise
- Class 3: Energy Balance
- Class 4: Cardiovascular/Pulmonary Responses
- Class 5: Self-Care
- Domain 5: Perception/Cognition
- Class 1: Attention
- Class 2: Orientation
- Class 3: Sensation/Perception
- Class 4: Cognition
- Class 5: Communication
- Domain 6: Self-Perception
- Class 1: Self-Concept
- Class 2: Self-Esteem
- Class 3: Body Image
- Domain 7: Role Relationship
- Class 1: Caregiving Roles
- Class 2: Family Relationships
- Class 3: Role Performance
- Domain 8: Sexuality
- Class 1: Sexual Identity
- Class 2: Sexual Function
- Class 3: Reproduction
- Domain 9: Coping/Stress Tolerance
- Class 1: Post-Trauma Responses
- Class 2: Coping Responses
- Class 3: Neurobehavioral Stress
- Domain 10: Life Principles
- Class 1: Values
- Class 2: Beliefs
- Class 3: Value/Belief/Action Congruence
- Domain 11: Safety/Protection
- Class 1: Infection
- Class 2: Physical Injury
- Class 3: Violence
- Class 4: Environmental Hazards
- Class 5: Defensive Processes
- Class 6: Thermoregulation
- Domain 12: Comfort
- Class 1: Physical Comfort
- Class 2: Environmental Comfort
- Class 3: Social Comfort
- Domain 13: Growth/Development
- Class 1: Growth
- Class 2: Development
Understanding this classification helps nurses select appropriate diagnoses within a structured framework.
The Nursing Process: Diagnosis in Context
Nursing diagnosis is the second step in the nursing process, a systematic, five-step approach to patient care:
- Assessment: Collecting comprehensive patient data.
- Diagnosis: Analyzing assessment data to identify nursing diagnoses.
- Planning: Developing a nursing care plan with goals and interventions.
- Implementation: Carrying out the planned interventions.
- Evaluation: Assessing the effectiveness of interventions and patient progress.
Each step of the nursing process relies on critical thinking. For effective diagnosis, nurses need to understand not only the definitions of nursing diagnoses but also their defining characteristics, related factors, and appropriate interventions. The nursing process is a dynamic and cyclical process, ensuring patient care is continuously assessed and adjusted based on patient needs and outcomes.
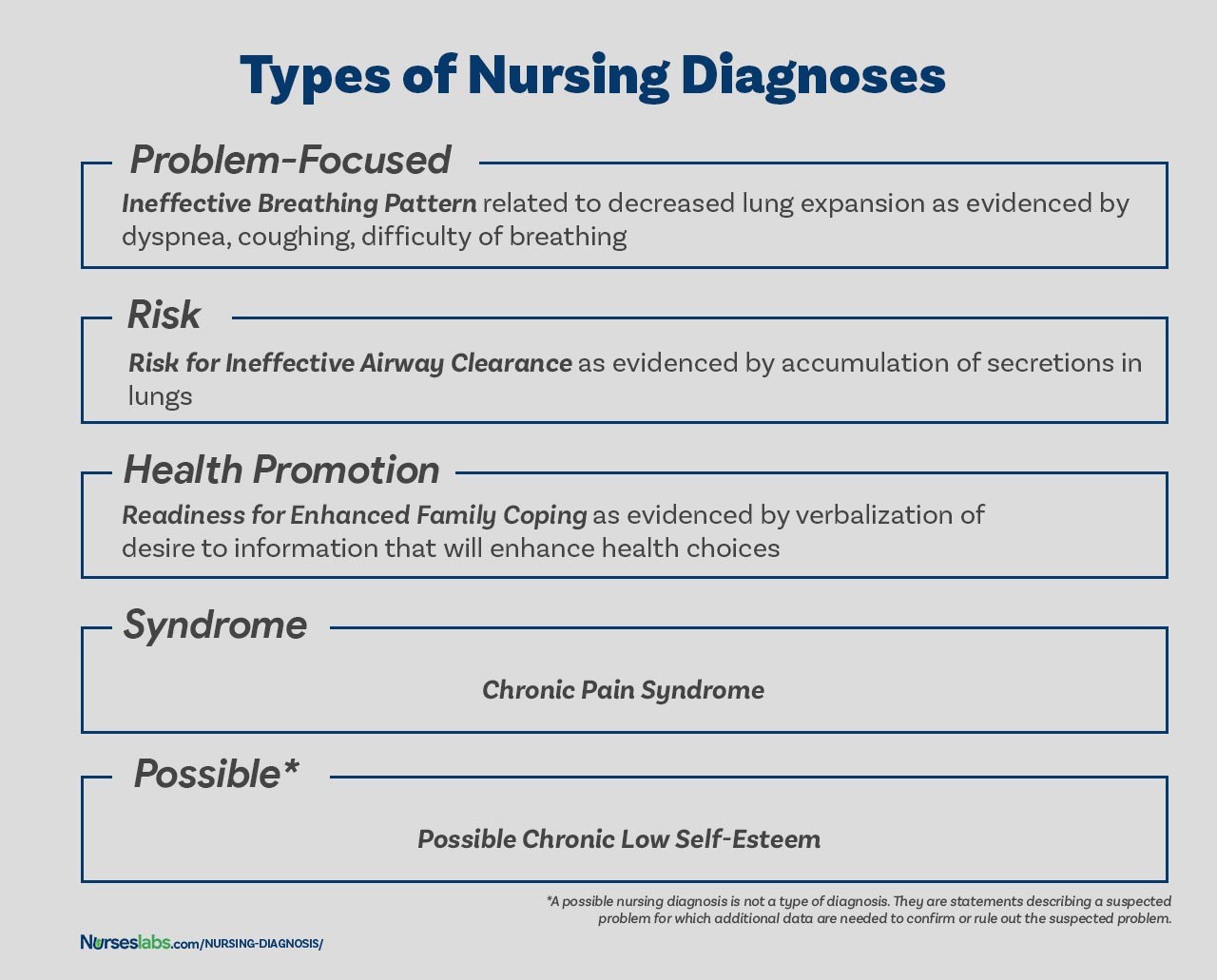
Types of Nursing Diagnoses: Choosing the Right Category
There are four main types of nursing diagnoses, each serving a distinct purpose in care planning:
- Problem-Focused (Actual) Nursing Diagnosis: Describes a current problem present at the time of assessment.
- Risk Nursing Diagnosis: Identifies potential problems a patient is vulnerable to developing.
- Health Promotion Nursing Diagnosis: Focuses on a patient’s desire to improve their well-being and health status.
- Syndrome Nursing Diagnosis: Clusters a group of nursing diagnoses that typically occur together.
Problem-Focused Nursing Diagnosis: Addressing Current Issues
A problem-focused nursing diagnosis, also known as an actual diagnosis, identifies an existing patient problem confirmed by signs and symptoms during the nursing assessment. While actual problems are evident, it’s important to remember that risk diagnoses can be equally or even more critical for preventative care.
Components of a Problem-Focused Nursing Diagnosis:
- Nursing Diagnosis Label: A standardized NANDA-I diagnosis name (e.g., Acute Pain).
- Related Factors: The “related to” phrase linking the diagnosis to contributing factors or etiology (e.g., related to surgical incision).
- Defining Characteristics: The “as evidenced by” phrase listing observable signs and symptoms (e.g., as evidenced by patient reporting pain level of 7/10 and guarding behavior).
Example: Acute Pain related to surgical incision as evidenced by patient reporting pain level of 7/10 and guarding behavior.
Risk Nursing Diagnosis: Preventing Potential Problems
Risk nursing diagnoses identify vulnerabilities – situations where a problem does not currently exist but is likely to develop without nursing intervention. They are based on risk factors – conditions or circumstances that increase susceptibility to a problem. Risk diagnoses are crucial for preventative care, allowing nurses to proactively mitigate potential health issues.
Components of a Risk Nursing Diagnosis:
- Risk Diagnosis Label: A standardized NANDA-I diagnosis name preceded by “Risk for” (e.g., Risk for Infection).
- Risk Factors: The “as evidenced by” phrase listing factors that increase risk (e.g., as evidenced by surgical wound and immunosuppression).
Example: Risk for Infection as evidenced by surgical wound and immunosuppression.
Important Note: Risk diagnoses use “as evidenced by” to connect the diagnosis to risk factors, not defining characteristics (which are absent as the problem hasn’t developed).
Health Promotion Diagnosis: Enhancing Well-being
Health promotion diagnoses, also called wellness diagnoses, focus on a patient’s readiness to enhance well-being and optimize health. They identify a patient’s strengths and motivation for positive health practices. These diagnoses are used to guide interventions that support health enhancement and higher levels of wellness.
Components of a Health Promotion Diagnosis:
- Health Promotion Diagnosis Label: A standardized NANDA-I diagnosis name, often starting with “Readiness for Enhanced…” (e.g., Readiness for Enhanced Nutrition).
- May include Related Factors: Although often a one-part statement, related factors can be added for clarity (e.g., Readiness for Enhanced Nutrition related to expressed interest in healthy eating).
Example: Readiness for Enhanced Nutrition related to expressed interest in healthy eating.
Syndrome Diagnosis: Recognizing Patterns
Syndrome diagnoses represent a cluster of nursing diagnoses that are frequently seen together due to a specific event or situation. They are also written as one-part statements, using only the diagnostic label. Syndrome diagnoses help nurses recognize common patterns of problems and plan holistic care.
Examples of Syndrome Diagnoses:
- Rape-Trauma Syndrome
- Disuse Syndrome
- Relocation Stress Syndrome
Possible Nursing Diagnosis: Investigating Suspected Problems
A possible nursing diagnosis is used when a nurse suspects a problem but needs more data to confirm or rule it out. It indicates a need for further assessment and data collection. It is not a formal type of diagnosis but rather a temporary label to guide investigation.
Example: Possible Risk for Deficient Fluid Volume related to unknown etiology. (Further assessment needed to confirm fluid volume status and contributing factors).
Components of a Nursing Diagnosis Statement: Building Blocks for Clarity
A complete nursing diagnosis statement typically has three key components, particularly for problem-focused diagnoses:
- Problem (Diagnostic Label): A concise term describing the patient’s health problem.
- Etiology (Related Factors): Contributing factors or causes of the problem.
- Defining Characteristics (Signs & Symptoms): Evidence that the problem exists (for actual diagnoses) or risk factors (for risk diagnoses).
Problem and Definition: The Diagnostic Label
The problem statement or diagnostic label is a standardized term from a recognized classification system like NANDA-I. It concisely describes the patient’s health response requiring nursing intervention. Diagnostic labels often include qualifiers (modifiers) to add specificity and meaning:
| Qualifier | Focus of the Diagnosis | Example |
|---|---|---|
| Deficient | Fluid Volume | Deficient Fluid Volume |
| Imbalanced | Nutrition: Less Than Body Requirements | Imbalanced Nutrition: Less Than Body Requirements |
| Impaired | Gas Exchange | Impaired Gas Exchange |
| Ineffective | Tissue Perfusion | Ineffective Peripheral Tissue Perfusion |
| Risk for | Injury | Risk for Injury |
Some diagnoses are single words (e.g., Anxiety, Constipation), where the qualifier and focus are inherent in the term.
Etiology: Identifying Related Factors
The etiology or related factors component identifies the probable causes or contributing factors to the health problem. Understanding etiology is crucial because nursing interventions should be directed at addressing these underlying causes. Etiology is linked to the problem statement using the phrase “related to.”
Example: Impaired Physical Mobility related to pain and stiffness.
Risk Factors: For Risk Diagnoses
For risk nursing diagnoses, risk factors replace etiological factors. Risk factors are conditions that increase vulnerability to a problem. They are written after “as evidenced by” in the diagnostic statement.
Example: Risk for Falls as evidenced by history of falls and impaired balance.
Defining Characteristics: Signs and Symptoms
Defining characteristics are the observable signs and symptoms that cluster together to indicate the presence of an actual nursing diagnosis. For risk diagnoses, defining characteristics are absent; instead, risk factors serve as the evidence. Defining characteristics are linked to the diagnosis statement using “as evidenced by” or “as manifested by.”
Example: Ineffective Airway Clearance related to excessive mucus as evidenced by productive cough and abnormal breath sounds.
The Diagnostic Process: A Step-by-Step Approach
Formulating accurate nursing diagnoses involves a systematic diagnostic process with three key phases:
- Data Analysis: Examine collected assessment data.
- Problem Identification: Identify health problems, risks, and strengths.
- Diagnostic Statement Formulation: Write the nursing diagnosis statement.
Analyzing Data: Finding Patterns and Gaps
Data analysis involves several key steps:
- Comparing Data to Standards: Compare patient data to established norms and healthy ranges to identify deviations.
- Clustering Cues: Group related data points together to identify patterns and potential problems.
- Identifying Gaps and Inconsistencies: Look for missing information or conflicting data that requires further investigation.
Identifying Health Problems, Risks, and Strengths: Making Clinical Judgments
After data analysis, the nurse, in collaboration with the patient, identifies:
- Actual Problems: Existing health issues identified through assessment data.
- Risk Problems: Potential issues the patient is vulnerable to.
- Possible Problems: Suspected issues requiring further data.
- Strengths: Patient’s resources, abilities, and coping mechanisms that can be leveraged in the care plan.
This step also involves differentiating between nursing diagnoses, medical diagnoses, and collaborative problems to ensure appropriate interventions are planned.
Formulating Diagnostic Statements: Communicating the Diagnosis Clearly
The final phase is formulating the diagnostic statement, which clearly and concisely communicates the nursing diagnosis. The structure and components of the statement depend on the type of nursing diagnosis being formulated.
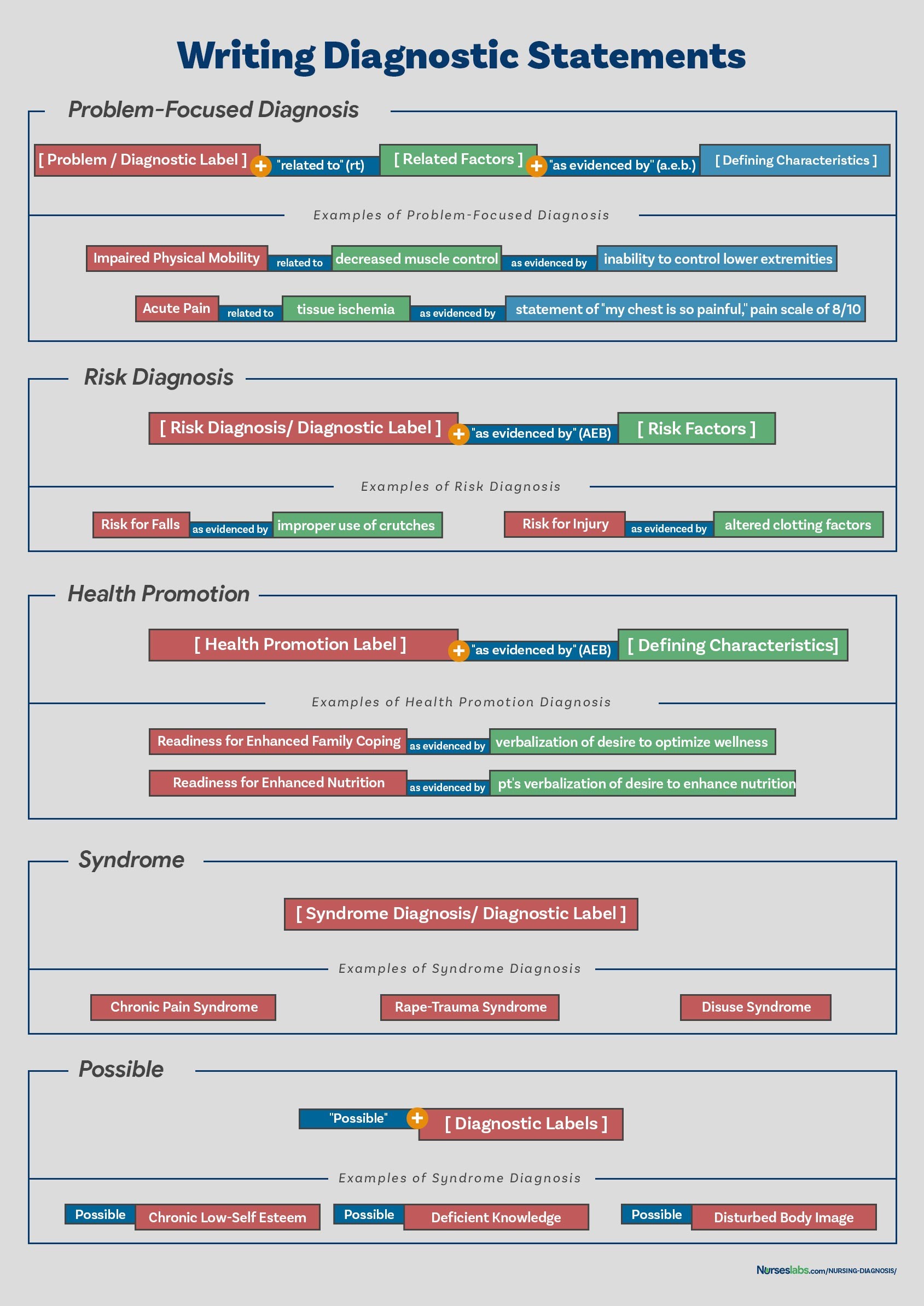
How to Write a Nursing Diagnosis Statement: Different Formats for Different Needs
Writing effective nursing diagnosis statements requires understanding different formats based on the type of diagnosis. Accurate and well-written statements are essential for clear communication and effective care planning.
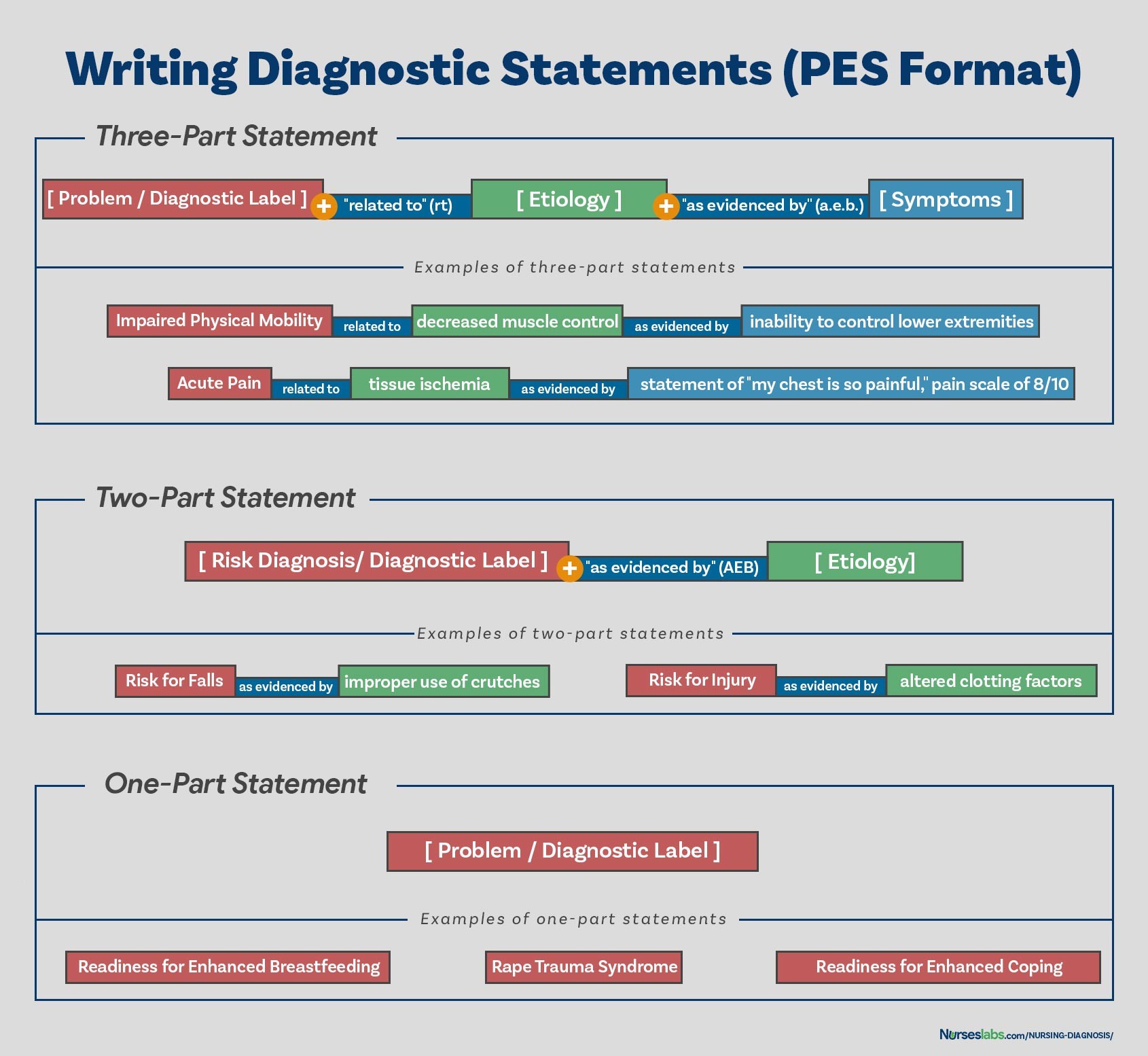
PES Format: A Common Framework
The PES format (Problem-Etiology-Symptoms) is a widely used structure for writing nursing diagnoses, particularly for problem-focused diagnoses. It ensures all essential components are included:
- P (Problem): The diagnostic label (NANDA-I diagnosis).
- E (Etiology): Related factors, linked with “related to.”
- S (Symptoms): Defining characteristics, linked with “as evidenced by.”
PES format statements can be one-part, two-part, or three-part, depending on the type of diagnosis.
One-Part Nursing Diagnosis Statements
Health promotion diagnoses and syndrome diagnoses are typically written as one-part statements. For health promotion diagnoses, the related factor is often inherent (“motivated to enhance well-being”). Syndrome diagnoses also do not require related factors.
Examples:
- Readiness for Enhanced Coping
- Rape-Trauma Syndrome
Two-Part Nursing Diagnosis Statements
Risk diagnoses and possible diagnoses are written as two-part statements:
- Part 1: Diagnostic label (e.g., Risk for Infection).
- Part 2: Risk factors (for risk diagnoses) or validation for possible diagnoses, linked with “as evidenced by.”
Examples:
- Risk for Infection as evidenced by compromised immune system.
- Possible Deficient Fluid Volume related to unknown etiology.
Three-Part Nursing Diagnosis Statements
Problem-focused (actual) diagnoses typically use three-part statements (PES format):
- Part 1: Diagnostic label (Problem).
- Part 2: Related factors (Etiology), linked with “related to.”
- Part 3: Defining characteristics (Symptoms), linked with “as evidenced by” or “as manifested by.”
Example: Anxiety related to unfamiliar hospital environment as evidenced by restlessness and verbalization of fear.
Nursing Diagnosis: The Heart of Your Nursing Care Plan
Mastering nursing diagnosis is essential for creating effective, patient-centered nursing care plans. By understanding the types of diagnoses, their components, and the diagnostic process, nurses can accurately identify patient needs and develop targeted interventions. This guide provides a foundational understanding of how to make a diagnosis in a nursing care plan, empowering you to deliver high-quality, individualized care.
Recommended Resources
To further enhance your understanding and skills in nursing diagnosis and care planning, consider these resources:
- Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care
- Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition)
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care
- All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health
These resources offer comprehensive guidance, evidence-based interventions, and numerous examples to support your learning and practice in nursing diagnosis.
References and Sources
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.