Primary eye care is a vital component of community health services, encompassing both clinical care and proactive measures for eye health protection and promotion. For community eye care programs to be effective and sustainable, they must be driven and maintained by the community members themselves, with support from the eye care sector. This collaborative approach ensures that interventions are relevant to the community’s specific needs and integrated into their daily lives.
Effective primary eye care begins with a thorough “community diagnosis,” utilizing an epidemiological approach. This diagnosis is crucial for identifying and prioritizing the community’s eye health problems. Such a study should systematically gather key information to guide resource allocation and intervention strategies. The following elements are essential in this assessment:
- Magnitude (M): This refers to the prevalence and incidence of eye conditions within the community. It’s quantified by the number of individuals affected by specific conditions and the anticipated number of new cases within a defined period.
- Implication (I): This considers the social and economic impacts of eye conditions. It includes factors such as healthcare expenditures, lost productivity due to work absence, and educational disruption from school absenteeism.
- Vulnerability (V): This assesses the availability and effectiveness of interventions to address the identified eye conditions. Understanding the vulnerability helps determine if practical and impactful solutions exist.
- Cost (C): This evaluates the resources required to implement and sustain control programs for prioritized eye conditions. Cost considerations are crucial for ensuring program feasibility and long-term sustainability.
Prioritization of eye care interventions can be determined using a simple model that balances these factors:
Priority = (M×I×V) / C
This model provides a framework for objective decision-making in primary eye care planning, moving beyond purely clinical perspectives to incorporate public health principles and resource management. It helps to avoid biases that might arise from focusing solely on clinically interesting cases, ensuring that resource allocation aligns with the greatest community need.
Essential Service Components of Primary Eye Care
Community-based eye care services must be comprehensive, encompassing primary, secondary, and tertiary prevention strategies. These services should be accessible to all community members, regardless of whether they currently have eye problems. This broad approach distinguishes community-based care from hospital-centric models, which often focus primarily on existing patients.
Understanding the community’s eye health status at any given time involves recognizing three distinct groups within the population who require eye care screening:
- Healthy Group: Individuals with no apparent eye problems. Screening for this group focuses on health promotion and preventative measures to maintain their eye health.
- Group with Eye Diseases or Problems: Individuals already experiencing eye conditions. This group requires diagnosis, treatment, and management of their existing conditions.
- Group at Risk of Eye Diseases or Problems: Individuals with risk factors that increase their likelihood of developing eye conditions. Interventions for this group focus on early detection, risk reduction, and preventative strategies.
Therefore, primary eye care services should not be limited to clinical interventions. Equal, if not greater, emphasis is needed on preventive and promotive activities for the entire community, including those without current eye disease. Primary eye care, in its comprehensive form, addresses the full spectrum of eye health needs for all community members.
Clinical Service Components in Detail
Community diagnosis plays a pivotal role in shaping primary eye care activities, often revealing a unique perspective on the eye health landscape of specific communities. This understanding allows for the adaptation of service components to align with the community’s social, economic, and existing healthcare infrastructure. Consequently, the essential elements of primary eye care can vary significantly and extend beyond the commonly recognized major causes of blindness. Prevalent eye disorders within individual communities, even if seemingly minor from a global perspective, require simple yet effective services tailored to that community.
Decision-making regarding service components should be guided by public health priorities rather than solely by clinical interests. Conditions that are easily preventable and manageable, and common across many communities, are prime candidates for inclusion in primary eye care services. For example, addressing reading difficulties among the elderly or managing seasonal conjunctivitis can be as important as tackling major blinding conditions in certain community contexts.
The World Health Organization (WHO) provides essential guidelines for primary eye care, which are crucial for establishing effective community-based programs.
WHO Guidelines for Primary Eye Care
The WHO guidelines categorize eye conditions based on the level of care required, providing a framework for task shifting and appropriate referral pathways within primary eye care systems.
-
Conditions to be Recognized and Treated by Trained Primary Health Care Workers: These are conditions that can be effectively managed at the primary care level with appropriate training and resources.
- Conjunctivitis and Lid Infections:
- Acute conjunctivitis (inflammation of the conjunctiva)
- Ophthalmia neonatorum (conjunctivitis in newborns)
- Trachoma (chronic infectious disease of the eye)
- Allergic and irritative conjunctivitis (conjunctivitis due to allergies or irritants)
- Lid lesions, e.g., stye and chalazion (common eyelid conditions)
- Trauma:
- Subconjunctival hemorrhages (bleeding under the conjunctiva)
- Superficial foreign body (foreign object on the surface of the eye)
- Blunt trauma (eye injury from impact)
- Blinding Malnutrition: Nutritional deficiencies that can lead to vision loss.
- Conjunctivitis and Lid Infections:
-
Conditions to be Recognized and Referred After Treatment Initiation: These conditions require specialist referral, but primary healthcare workers can initiate initial management before referral.
- Corneal ulcers (open sores on the cornea)
- Lacerating or perforating injuries of the eyeball (severe eye injuries)
- Lid lacerations (cuts on the eyelids)
- Entropion/trichiasis (inward turning of eyelids/eyelashes)
- Burns: chemical, thermal (eye burns from chemicals or heat)
-
Conditions that Should be Recognized and Referred for Treatment: These conditions require immediate referral to specialized eye care professionals for diagnosis and management.
- Painful red eye with visual loss (symptoms indicating potentially serious eye conditions)
- Cataract (clouding of the lens of the eye)
- Pterygium (growth on the conjunctiva that can affect vision)
- Visual loss (unexplained reduction in vision)
Building upon the WHO guidelines and considering local epidemiological data, countries like Thailand, which initiated primary eye care programs in 1981, have integrated specific conditions into their primary health care frameworks. Thailand’s model includes:
- Cataract (age-related or “senile” type)
- Trachoma and its late complications
 graphic file with name jceh_11_26_019_f01.jpg
graphic file with name jceh_11_26_019_f01.jpg
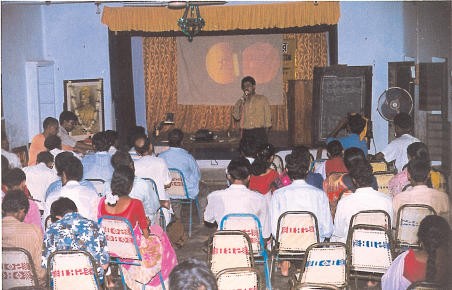
Discussion on common eye diseases for community volunteers, including teachers, traditional healers, and senior students, using an ICEH slide set. Vivekananda Mission Asram, West Bengal, India. - Eye injuries
- Corneal ulcer
- Glaucoma, acute attack and cases with one blind eye
- Ophthalmia neonatorum
- Eye infections
- Pterygium
- Refractive errors and reading difficulties
- Conditions with visual acuity less than 0.05 (indicating severe visual impairment)
Similar conditions were prioritized in Myanmar (formerly Burma) when they also launched primary eye care initiatives in 1981. These conditions represent the core clinical service elements of primary eye care in this region of the world, and are also highly relevant in Vietnam, Laos, Cambodia, and even parts of China.
However, primary eye care needs to be context-specific. Regions with high prevalence of conditions like onchocerciasis (river blindness) require tailored primary eye care strategies to address these specific local challenges.
The Integration Matrix: Embedding Eye Care within Primary Health Care
Primary eye care should not operate in isolation but rather be seamlessly integrated within the broader primary health care system. Primary eye care serves as an entry point to connect with the heart of community health initiatives. It’s crucial to recognize primary health care as the overarching system into which primary eye care is incorporated. Therefore, a thorough situational analysis of the community is essential for effective primary health care implementation, with particular attention to the integration of eye care elements.
Cultural evening focused on health care in India, highlighting community engagement and health promotion.
The integration matrix (Table 1) illustrates how eye care can be effectively integrated into existing primary health care frameworks, assuming a foundational health care system is in place.
Table 1. Primary Eye Care Integration Matrix
| PHC PEC | Health education | Family planning & MCH | Food & nutrition | Safe Water & basic sanitation | Extended programme of immunisation (∗∗) | Essential drugs | Control of local endemic diseases (∗∗∗∗) | Care for mild ailments (‘simple’ treatment) |
|---|---|---|---|---|---|---|---|---|
| Cataract Surgical Non-surgical | +++ ++ | + for congenital cataract | NA | NA | NA | ++ post operation care | +++ case finding, referral & community care | +++ case finding, referral & community care |
| Trachoma Active Complications | +++ ++ | +++ | +++ ++ | NA | +++ tetracycline ointment | trachoma programme +++ +++ | trachoma programme +++ +++ | |
| Glaucoma Acute attack Angle-closed(∗) | ++ ++ | + for congenital glaucoma | NA | NA | NA | ++ pilocarpine eye drops | ++ pilocarpine eye drops | |
| Eye injuries | ++ | +++ accident prevention | ++ improve environment | NA | +++ tetracycline ointment | +++ tetracycline ointment | ||
| Corneal ulcer | +++ | +++ accident prevention | NA | NA | measles immunisation | +++ tetracycline ointment | +++ tetracycline ointment | |
| Eye infections EKG Chronic | ++ ++ | +++ ++ | NA | ++ ++ | NA | +++ ++ | disaster management sometimes | +++ tetracycline ointment |
| Ophthalmia neonatorum | +++ | +++ | NA | +++ | +++ immediate referral | |||
| Pterygium Surgical Non-surgical | ++ + | NA | NA | ++ ++ | NA | NA | ++ referral | |
| Refractive error & Reading difficulties | ++ | ++ family screening | NA | NA | NA | + providing simple spectacles | + providing simple spectacles | |
| VA less than 0.05 ( | ++ | ++ family screening | NA | NA | NA | NA | ++ referral |
- (∗) In many instances, angle-closure glaucoma refers to the acute attack, with one eye already blind and prophylaxis required for the second eye. Secondary glaucoma is common among neglected age-related cataract patients.
- (∗∗) EPI staff are good health communicators, educators and gather community information.
- (∗∗∗) Diabetic retinopathy is common in some communities. This is the category 4 in the WHO categories of visual impairment.
- (∗∗∗∗) The cataract backlog might be regarded as an endemic disease in the given region, like tuberculosis, malaria and leprosy, etc. Trachoma, and its control is also relevant here. When the conditions are welt controlled, they become part of a successful integrated health programme in that locality.
Cataract Programs as a Model for Primary Eye Care Integration
Cataract programs serve as an excellent illustration of how primary eye care can effectively function within the primary health care framework. The success of cataract programs integrated into primary eye care has been demonstrated across numerous countries. These programs heavily rely on community participation, particularly in case finding and facilitating referrals for surgery. Surgical eye teams can operate cost-effectively when community-level preparations are thoroughly completed before surgical interventions.
Cataract program activities typically begin with brief training sessions for community health workers on cataract recognition. This is followed by door-to-door visits to identify potential cases. Multi-stage screening is a key aspect of primary eye care in case finding, and in encouraging patients to seek surgical treatment. Simultaneously, comprehensive eye care information should be disseminated throughout the community using various communication channels. Table 2 summarizes potential community-level activities within a cataract program.
Table 2. Cataract Program at Community Level
| Level | Individual | Family | Community | 1st level of contact (Health Centre) | 1st level of referral (District Hospital) |
|---|---|---|---|---|---|
| Action | Aware of own vision. Slowly progressing, painless visual impairment, either one or both eyes. Respond to health workers after screening. Prompt report to eye team for operation. | Help bringing the cataract patient to eye unit. Encourage operation and prepare hospitalisation. Adequate postoperative care and suitable home and out-door activites. | Co-operate with health workers and visiting eye personnel in surgical care. Surgical subsidies for the poor. | Co-operate with visiting eye team in community activities. Co-ordinate community in the cataract programmes. | Co-operate with visiting eye team and preparation of service sites. Post-operative follow-up. Proper care for complicated cases. |
| Input | Health education, posters, booklets, etc. | Health education, posters, booklets, etc. | Primary eye care course. Primary eye care kits, manual and guidelines, records and reporting systems. | Primary eye care course, minimum supplies and equipment, records and reporting systems. | Short, clinical training, minimum required supplies and equipment. Monitoring/supervision. |
Conclusion
Primary eye care is an essential public health service that must be community-based and integrated into broader primary health care systems. By adopting a comprehensive approach that includes community diagnosis, preventative measures, and clinical services, and by prioritizing conditions based on magnitude, implication, vulnerability, and cost, primary eye care programs can effectively address the eye health needs of communities worldwide. The integration matrix and the example of cataract programs highlight practical strategies for implementing and scaling up successful primary eye care initiatives, ultimately contributing to improved vision and quality of life for all.