Impaired oral mucous membrane is a common nursing diagnosis that indicates disruptions to the delicate tissues lining the mouth. This condition can significantly affect patient comfort, nutrition, and overall well-being. Understanding the causes, symptoms, and appropriate nursing interventions is crucial for effective patient care. This article provides a comprehensive nursing care plan for patients diagnosed with impaired oral mucous membrane, focusing on assessment, diagnosis, expected outcomes, and targeted interventions to promote oral health and patient comfort.
Understanding Impaired Oral Mucous Membrane
According to NANDA International, Inc., impaired oral mucous membrane is defined as the state in which an individual experiences or is at risk of experiencing disruptions in the tissues of the oral cavity. This disruption can range from mild dryness to severe lesions and infections, impacting the patient’s ability to eat, speak, and maintain oral hygiene. Recognizing the risk factors and signs of impaired oral mucous membrane is the first step in providing effective nursing care.
Common Causes and Risk Factors
Several factors can contribute to the development of impaired oral mucous membranes. These can be broadly categorized as:
- Systemic Factors:
- Dehydration: Reduced fluid intake leads to dryness throughout the body, including the oral mucosa.
- Nutritional Deficiencies: Lack of essential vitamins and minerals, particularly B vitamins, iron, and vitamin C, can weaken oral tissues.
- Medical Conditions: Conditions like diabetes mellitus, Sjögren’s syndrome, and renal failure are associated with dry mouth (xerostomia) and impaired oral mucosa.
- Medications: Many medications, including steroids, immunosuppressants, anti-neoplastic drugs, anticholinergics, diuretics, and antihistamines, can have a drying effect on the oral mucosa.
- Local Factors:
- Mechanical Irritation: Ill-fitting dentures, nasogastric tubes, trauma, or aggressive tooth brushing can damage the oral tissues.
- Mouth Breathing: Chronic mouth breathing, often due to nasal congestion or habits, dries out the oral mucosa.
- Inadequate Oral Hygiene: Poor oral hygiene practices lead to plaque and bacterial buildup, increasing the risk of infection and inflammation.
- Radiation Therapy and Chemotherapy: These cancer treatments can severely damage the rapidly dividing cells of the oral mucosa, leading to mucositis.
- Infections: Viral, bacterial, or fungal infections like oral candidiasis (thrush) can directly impair the oral mucous membrane.
Signs and Symptoms
Patients with impaired oral mucous membranes may present with a variety of signs and symptoms, including:
- Dryness (Xerostomia): A common complaint, patients may describe a sticky, dry feeling in the mouth.
- Redness (Erythema): Inflammation of the oral mucosa can cause redness.
- Lesions or Ulcerations: Open sores or breaks in the mucosal lining can be painful and prone to infection.
- Coated Tongue: A white or yellowish coating on the tongue may indicate bacterial or fungal overgrowth.
- Leukoplakia: White patches on the mucous membrane that cannot be scraped off, sometimes precancerous.
- Edema: Swelling of the oral tissues.
- Gingivitis: Inflammation of the gums, characterized by redness, swelling, and bleeding.
- Purulent Drainage: Pus or discharge may indicate infection.
- Taste Changes: Altered taste perception or loss of taste.
- Pain or Discomfort: Soreness, tenderness, or burning sensations in the mouth.
- Difficulty Eating or Swallowing: Pain and dryness can make chewing and swallowing uncomfortable.
Nursing Diagnosis
Impaired Oral Mucous Membrane related to [related factor, e.g., drying effect of steroid medication, dehydration, inadequate oral hygiene] as evidenced by [evidence, e.g., patient report of dry mouth, dry and red mucous membranes, presence of leukoplakia].
Example: Impaired Oral Mucous Membrane related to drying effect of prolonged use of steroids as evidenced by patient report of “extremely tender” mouth, dry mucous membranes, and red tongue with some leukoplakia.
Nursing Assessment
A thorough assessment is essential to identify the extent and cause of impaired oral mucous membranes. This includes both subjective and objective data collection.
Subjective Data
- Patient History: Gather information about the patient’s medical history, including pre-existing conditions, medications, allergies, and any history of oral problems.
- Symptom Assessment: Ask the patient to describe their oral symptoms, including onset, duration, severity, and relieving or aggravating factors. Specifically inquire about:
- Dryness, soreness, or pain in the mouth.
- Difficulty eating, swallowing, or speaking.
- Changes in taste.
- Oral hygiene practices.
- Use of dentures or other oral appliances.
Objective Data
- Physical Examination:
- Inspect the oral cavity: Use a penlight and tongue blade to visualize the oral mucosa, tongue, gums, and teeth. Assess for:
- Moisture level: Dry, moist, or excessively salivated.
- Color: Pink, red, pale, or white patches.
- Integrity: Lesions, ulcers, cracks, or bleeding.
- Coatings: Presence of plaque, debris, or abnormal coatings on the tongue or mucosa.
- Condition of gums: Swelling, redness, bleeding.
- Condition of teeth: Caries, missing teeth, dentures fit.
- Palpate oral tissues: Gently palpate for tenderness, masses, or induration.
- Assess Saliva: Observe the quantity and consistency of saliva. Is it thick, ropey, or watery?
- Inspect the oral cavity: Use a penlight and tongue blade to visualize the oral mucosa, tongue, gums, and teeth. Assess for:
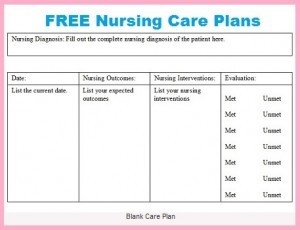 Nursing Care Plan
Nursing Care Plan
Image alt text: Nurse reviewing a patient’s medical chart to develop a nursing care plan, emphasizing patient-centered care and systematic healthcare planning.
Nursing Outcomes (Goals)
The goals of nursing interventions for impaired oral mucous membranes are patient-centered and measurable. Examples include:
- Short-term Goals:
- Patient will report decreased oral discomfort while eating and drinking within 24-48 hours.
- Patient will demonstrate proper oral rinsing techniques after meals within 24 hours.
- Long-term Goals:
- Patient’s oral mucous membranes will appear moist, pink, and intact within 3-5 days.
- Patient will maintain oral mucous membranes free from plaque and infection throughout hospitalization.
- Patient will verbalize three methods to manage dry mouth upon discharge.
- Patient will demonstrate consistent and proper oral hygiene practices by discharge.
Nursing Interventions
Nursing interventions aim to alleviate symptoms, promote healing, prevent complications, and educate the patient on self-care.
Oral Hygiene Practices
- Gentle Oral Care: Provide or assist with gentle oral hygiene at least twice daily and after meals. Use a soft-bristled toothbrush and non-irritating toothpaste.
- Mouth Rinses: Encourage frequent mouth rinsing (every 2-3 hours and as needed) with:
- Saline Solution: Isotonic saline is gentle and effective for moisturizing and cleansing.
- Sodium Bicarbonate Solution: A mild solution can help neutralize acidity and soothe inflamed mucosa (e.g., ½ teaspoon of baking soda in 8 ounces of water). Avoid overuse as it can disrupt oral pH balance.
- Avoid Alcohol-Based Mouthwashes: These can further dry and irritate the oral mucosa.
- Avoid Lemon Glycerin Swabs: Lemon can be acidic and drying, and glycerin can leave a sticky residue.
- Avoid Prolonged Use of Hydrogen Peroxide: While sometimes used for debridement, prolonged use can damage healthy tissues.
- зубная floss (if appropriate): If the patient’s gums are healthy enough, gentle flossing once daily can help remove plaque. Avoid flossing if gums are bleeding or very tender.
Moisturizing and Lubricating Oral Mucosa
- Humidification: Encourage humidification of the patient’s environment, especially if mouth breathing is a factor.
- искусственная saliva: Administer artificial saliva products as prescribed or recommended to keep the oral mucosa moist. These come in sprays, gels, and lozenges.
- Lubricants: Apply water-soluble lip lubricants frequently to prevent cracked and dry lips.
- Sucking on Sugar-Free Candies or Lozenges: Sugar-free options can stimulate saliva production and provide moisture. Avoid sugary candies, which can contribute to dental caries.
- Frequent Sips of Water: Encourage small, frequent sips of water throughout the day to maintain hydration and oral moisture. Avoid sugary drinks and acidic juices.
Patient Education
- Self-Care Techniques: Educate the patient and family on proper oral hygiene techniques, including gentle brushing, rinsing, and moisturizing.
- Medication Education: If medications are contributing to dry mouth, discuss strategies with the physician, such as adjusting medication timing, dosage, or considering alternative medications if possible.
- Dietary Modifications: Recommend soft, moist foods that are easy to chew and swallow. Avoid spicy, acidic, or very hot foods that can irritate the oral mucosa.
- Hydration Importance: Emphasize the importance of adequate fluid intake.
- When to Seek Medical Advice: Instruct the patient to report any worsening symptoms, signs of infection (increased pain, swelling, pus), or inability to manage symptoms at home.
- Dry Mouth Management at Home: Educate the patient on home remedies for dry mouth, such as using a humidifier, sugar-free saliva stimulants, and avoiding irritants like smoking and alcohol.
By implementing this comprehensive nursing care plan, nurses can effectively address impaired oral mucous membranes, improve patient comfort, and promote oral health. Consistent assessment, targeted interventions, and thorough patient education are key to achieving positive outcomes and preventing complications.