Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition that manifests in early childhood and impacts various aspects of a child’s life. Characterized by challenges in social interaction, communication, and the presence of restricted or repetitive behaviors or interests, ASD requires a multifaceted approach to care. For pediatric nurses, developing a robust and individualized nursing care plan following a diagnosis of ASD is paramount to providing effective, compassionate, and patient-centered care. This comprehensive guide delves into the critical components of a Pediatric Autism Spectrum Disorder Diagnosis Nursing Care Plan, aiming to equip healthcare professionals with the knowledge and strategies necessary to support children and their families effectively.
%25252520Autism%25252520Spectrum%25252520Disorder.jpeg)
Understanding Pediatric Autism Spectrum Disorder
Pediatric Autism Spectrum Disorder is not a single condition but a spectrum, meaning its presentation and severity vary widely among individuals. The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), defines ASD by persistent difficulties in social communication and social interaction across multiple contexts, alongside restricted, repetitive patterns of behavior, interests, or activities. These symptoms are present from early childhood and significantly limit and impair everyday functioning.
The spectrum nature of ASD means that one child might present with significant language delays and intense sensory sensitivities, while another may have advanced verbal skills but struggle profoundly with social reciprocity and nuanced communication. Recognizing this heterogeneity is the first step in creating a personalized and effective nursing care plan. Early diagnosis, often occurring in the pediatric setting, is crucial as it opens doors to early intervention services, which are proven to significantly improve long-term outcomes for children with ASD.
Key Characteristics in Pediatric ASD
Identifying the core characteristics of ASD in children is essential for accurate diagnosis and tailored nursing interventions. These characteristics typically fall into several categories:
- Social Communication and Interaction Deficits: This domain includes difficulties in social-emotional reciprocity, challenges with nonverbal communicative behaviors used for social interaction, and deficits in developing, maintaining, and understanding relationships. Pediatric nurses may observe a child struggling to initiate or respond to social interactions, make eye contact, understand social cues, or engage in imaginative play with peers.
- Restricted, Repetitive Behaviors, Interests, or Activities: This category encompasses stereotyped or repetitive motor movements, use of objects, or speech; insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior; highly restricted, fixated interests that are abnormal in intensity or focus; and hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment. Examples in a pediatric setting might include repetitive rocking, lining up toys obsessively, distress at changes in routine, or extreme reactions to certain sounds or textures.
- Sensory Processing Differences: Many children with ASD experience atypical sensory processing. This can manifest as hypersensitivity (over-responsiveness) or hyposensitivity (under-responsiveness) to sensory stimuli such as sounds, lights, touch, taste, smell, pain, temperature, and movement. These sensitivities can significantly impact a child’s comfort, behavior, and ability to engage in daily activities.
- Cognitive and Learning Profiles: Cognitive abilities in children with ASD are highly variable. Some children may have intellectual disabilities, while others may have average or above-average intelligence. Learning styles also differ, with many children with ASD being visual learners and benefiting from structured, predictable environments. Nurses need to be aware of these varied cognitive profiles when implementing care plans and educational strategies.
Understanding these multifaceted characteristics is fundamental for pediatric nurses in formulating a nursing care plan that addresses the specific and individualized needs of each child diagnosed with ASD.
Developing a Pediatric ASD Nursing Care Plan
A nursing care plan for a child with pediatric ASD must be comprehensive, individualized, and family-centered. It should be developed in collaboration with the child’s family, caregivers, and a multidisciplinary team of professionals, including physicians, therapists (speech, occupational, behavioral), and educators. The primary goals of the nursing care plan are to promote the child’s optimal development, enhance their quality of life, and support the family in managing the challenges associated with ASD.
Key Components of a Pediatric ASD Nursing Care Plan:
-
Assessment: A thorough and ongoing assessment is the cornerstone of an effective care plan. This includes:
- Developmental History: Gathering detailed information about the child’s developmental milestones, including communication, social, motor, and cognitive skills.
- Behavioral Assessment: Identifying and documenting specific challenging behaviors (aggression, self-injury, tantrums, elopement), their triggers, and their frequency, intensity, and duration. Standardized tools like the Vineland Adaptive Behavior Scales or the Aberrant Behavior Checklist may be used.
- Communication Assessment: Evaluating the child’s communication abilities, both verbal and nonverbal, and identifying communication strengths and weaknesses.
- Sensory Assessment: Determining the child’s sensory sensitivities and preferences through observation and parental reports. Sensory profiles can be helpful tools.
- Medical History and Comorbidity Assessment: Identifying any co-occurring medical conditions, such as seizures, gastrointestinal disorders, sleep disturbances, or anxiety, which are common in children with ASD and require integrated management.
- Family Assessment: Understanding the family’s strengths, needs, resources, and cultural background. Assessing family dynamics and coping mechanisms is crucial for providing holistic support.
-
Nursing Diagnoses: Based on the assessment data, appropriate nursing diagnoses are formulated. Common nursing diagnoses for children with ASD may include:
- Impaired Social Interaction
- Impaired Verbal Communication
- Delayed Growth and Development
- Sensory Processing Sensitivity
- Risk for Self-Directed Violence
- Anxiety
- Disturbed Sleep Pattern
- Caregiver Role Strain
-
Planning and Goals: Specific, measurable, achievable, relevant, and time-bound (SMART) goals are established for each nursing diagnosis. Goals should be individualized and prioritize the child’s and family’s needs. Examples of goals might include:
- The child will initiate social interaction with a peer during playtime within one month.
- The child will use a picture exchange communication system (PECS) to request desired items by the end of two weeks.
- The child will participate in self-care activities (e.g., brushing teeth) with minimal prompting within six weeks.
- The child will demonstrate reduced sensory-seeking behaviors in noisy environments within three weeks.
- The child will sleep through the night for 5 out of 7 nights within one month.
- Caregivers will report decreased feelings of stress and increased access to respite care within two months.
-
Nursing Interventions: These are the specific actions nurses will take to achieve the established goals. Interventions should be evidence-based and tailored to the child’s and family’s unique needs. Key intervention areas include:
-
Enhancing Communication and Social Interaction:
- Utilizing visual supports (picture schedules, social stories, visual timers) to aid understanding and predictability.
- Implementing augmentative and alternative communication (AAC) systems if needed (PECS, speech-generating devices).
- Facilitating social skills training through structured play and social stories.
- Creating opportunities for structured social interactions in safe and supportive environments.
-
Managing Challenging Behaviors:
- Conducting functional behavior assessments (FBAs) to understand the function (purpose) of challenging behaviors.
- Developing positive behavior support (PBS) plans that focus on antecedent modifications, teaching replacement behaviors, and consequence strategies.
- Using evidence-based behavioral interventions such as Applied Behavior Analysis (ABA) principles.
- Creating structured and predictable routines to minimize anxiety and behavioral triggers.
-
Addressing Sensory Sensitivities:
- Creating sensory-friendly environments by reducing overwhelming stimuli (noise, bright lights).
- Providing sensory tools and activities to meet sensory needs (weighted blankets, fidget toys, quiet spaces).
- Collaborating with occupational therapists to develop sensory integration strategies.
- Educating caregivers on recognizing and responding to sensory overload.
-
Promoting Self-Care and Adaptive Skills:
- Breaking down self-care tasks into smaller, manageable steps.
- Using visual schedules and task analyses to teach daily living skills (dressing, hygiene, feeding).
- Providing positive reinforcement and prompting to encourage independence.
-
Managing Comorbidities:
- Monitoring for and managing seizures according to prescribed medication regimens and safety protocols.
- Collaborating with dietitians and gastroenterologists to address gastrointestinal issues through dietary modifications and medication management.
- Implementing strategies to improve sleep hygiene and address sleep disturbances.
- Working with mental health professionals to manage anxiety, depression, or ADHD if co-occurring.
-
-
Evaluation: Regularly evaluate the effectiveness of the nursing care plan by monitoring the child’s progress towards the established goals. Adjust the plan as needed based on ongoing assessment data and the child’s and family’s evolving needs. Document progress, modifications, and outcomes clearly and consistently.
Strategies for Managing Challenging Behaviors in Pediatric ASD
Challenging behaviors are a significant concern in pediatric ASD and require proactive and compassionate management within the nursing care plan. Effective strategies are rooted in understanding the function of the behavior and implementing positive, proactive interventions.
Table: Common Strategies for Managing Challenging Behaviors in Pediatric Autism
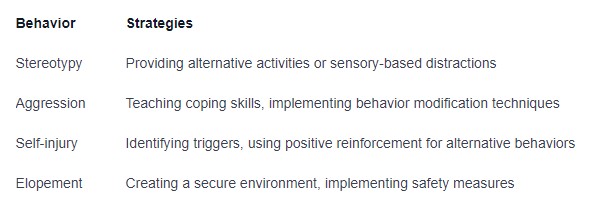 Strategies for Managing Challenging Behaviors in Pediatric Autism: A table outlining common behavioral interventions and nursing considerations for children with autism spectrum disorder.
Strategies for Managing Challenging Behaviors in Pediatric Autism: A table outlining common behavioral interventions and nursing considerations for children with autism spectrum disorder.
Supporting Families of Children with Pediatric ASD
Providing care for a child with ASD extends beyond the child themselves to encompass the entire family. Family support is a critical component of the pediatric ASD nursing care plan. Nurses play a vital role in:
- Education: Providing families with comprehensive information about ASD, diagnosis, treatment options, and available resources.
- Emotional Support: Offering empathetic listening, validation, and emotional support to families navigating the challenges of raising a child with ASD.
- Respite Care Information: Connecting families with respite care services to provide temporary relief and prevent caregiver burnout.
- Advocacy: Assisting families in accessing needed services, advocating for their child’s needs within healthcare and educational settings.
- Community Resources: Linking families with local support groups, autism organizations, and community-based services.
- Sibling Support: Recognizing the needs of siblings and providing resources to help them understand ASD and cope with the family dynamics.
Ensuring Safety and Promoting Well-being
Safety is paramount in the nursing care of children with ASD. This includes:
- Environmental Safety: Creating safe environments that minimize sensory overload and potential hazards. This may involve securing exits to prevent elopement, padding sharp corners, and reducing loud noises and bright lights.
- Seizure Precautions: For children with seizure disorders, implementing seizure precautions and ensuring staff and family are trained in seizure first aid.
- Medication Safety: Ensuring safe medication administration and monitoring for side effects, particularly for medications used to manage comorbidities.
- Promoting Healthy Habits: Encouraging healthy eating, physical activity, and sleep routines to promote overall well-being.
- Addressing Bullying and Social Isolation: Educating families and schools about bullying prevention and strategies to promote social inclusion for children with ASD.
Conclusion
Developing a pediatric autism spectrum disorder diagnosis nursing care plan is a complex yet profoundly rewarding endeavor. By understanding the unique characteristics of ASD, conducting thorough assessments, and implementing individualized, evidence-based interventions, pediatric nurses can significantly improve the lives of children with ASD and their families. A collaborative, family-centered approach, focused on promoting communication, social interaction, managing challenging behaviors, addressing comorbidities, and ensuring safety and well-being, is essential for providing holistic and compassionate nursing care that empowers children with ASD to reach their full potential. Ongoing evaluation and adaptation of the care plan are crucial to meet the evolving needs of the child and family throughout their journey with ASD.