Crafting an exceptional nursing care plan hinges on a systematic approach to accurately identify patient needs and potential health risks. This guide offers a detailed walkthrough for developing a robust care plan, emphasizing the critical role of Ncp Nursing Diagnosis. For nursing students and seasoned professionals alike, this resource provides a comprehensive understanding of nursing care plans (NCPs) and the vital function of nursing diagnoses within them. Explore care plan components, illustrative examples, objectives, and the significance of precise ncp nursing diagnosis in enhancing patient outcomes.
Understanding Nursing Care Plans and the Role of Nursing Diagnosis
A Nursing Care Plan (NCP) is a structured framework employed in nursing practice to pinpoint current patient needs and foresee potential health challenges. Crucially, at the heart of every effective NCP lies a well-formulated ncp nursing diagnosis. This diagnosis acts as the cornerstone, guiding the entire care process. NCPs serve as a vital communication tool among nurses, patients, and the broader healthcare team, ensuring cohesive strategies to achieve desired health results. Without the systematic process of nursing care planning, especially the accurate formulation of ncp nursing diagnosis, the consistency and caliber of patient care would undoubtedly suffer.
The nursing care planning journey, deeply rooted in ncp nursing diagnosis, commences upon a patient’s admission and remains a dynamic process. It undergoes continuous refinement, adapting to shifts in the patient’s condition and in response to assessments of goal attainment. The ability to plan and deliver care that is both individualized and patient-centric is the bedrock of outstanding nursing practice. This personalized approach is directly informed by the initial and ongoing ncp nursing diagnosis.
Types of Nursing Care Plans and the Application of Nursing Diagnoses
Nursing care plans exist on a spectrum from informal mental strategies to formal documented guides. An informal NCP is a nurse’s internal plan of action, while a formal NCP is a documented, often computerized, record of patient care strategies.
Formal NCPs are further categorized into standardized and individualized plans. Standardized care plans provide pre-set guidelines for common patient needs, whereas individualized care plans are customized to address the unique needs of a specific patient, needs often identified through a detailed ncp nursing diagnosis.
Standardized Care Plans: A Foundation Built on Common Nursing Diagnoses
Standardized care plans are pre-established protocols developed by healthcare teams to ensure consistent care for patients with similar conditions. These plans are valuable for meeting essential care standards and optimizing nurses’ time by streamlining routine tasks for frequently encountered patient needs. They are often built upon a foundation of common ncp nursing diagnoses associated with specific conditions.
While standardized care plans offer a starting point, they are intentionally broad and not tailored to individual patient goals or specific ncp nursing diagnoses. They serve as a template that needs to be adapted.
The care plans outlined in this guide serve as standardized examples, providing a framework for developing individualized care plans based on specific ncp nursing diagnoses.
Individualized Care Plans: Tailoring Care Through Precise Nursing Diagnosis
An individualized care plan refines a standardized plan to align with the unique needs and objectives of each patient. This personalization is driven by a thorough ncp nursing diagnosis that captures the patient’s specific health status, challenges, and strengths. This approach ensures more targeted and holistic care, resonating with the patient’s distinct circumstances, resources, and aspirations.
Furthermore, individualized care plans, rooted in precise ncp nursing diagnosis, enhance patient satisfaction. When patients perceive their care as personalized and responsive to their individual needs identified through ncp nursing diagnosis, they are more likely to feel valued and understood, leading to greater contentment with their healthcare experience. In today’s healthcare landscape, where patient satisfaction is a key indicator of quality, this aspect is increasingly crucial.
Tips for Individualizing a Nursing Care Plan Based on NCP Nursing Diagnosis:
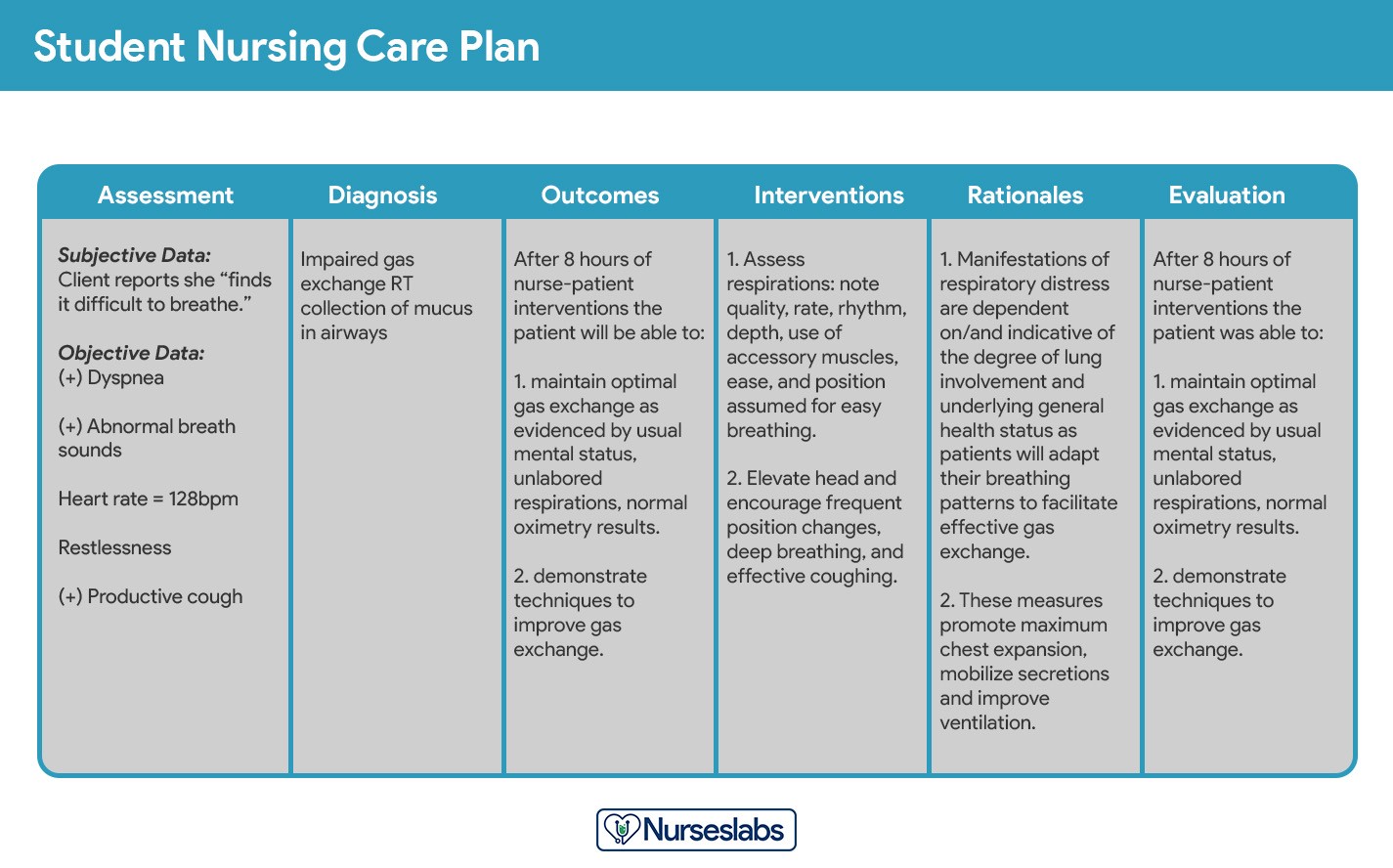
Student nursing care plans are more detailed.
Objectives of Nursing Care Plans and the Centrality of Nursing Diagnosis
The objectives of creating nursing care plans, especially in the context of ncp nursing diagnosis, are multifaceted:
- To foster evidence-based nursing practice and create a supportive and predictable environment within healthcare settings.
- To champion holistic care, addressing the patient’s physical, psychological, social, and spiritual dimensions in disease management and prevention, all informed by the ncp nursing diagnosis.
- To establish structured care pathways and bundles. Care pathways ensure team consensus on care standards and desired outcomes, while care bundles focus on best practices for specific conditions, both relying on accurate ncp nursing diagnosis.
- To clearly define and differentiate between goals and expected outcomes, ensuring they are directly related to the ncp nursing diagnosis.
- To refine communication and documentation of the care plan, making the ncp nursing diagnosis a central point of reference.
- To establish metrics for evaluating nursing care effectiveness, based on the outcomes linked to the ncp nursing diagnosis.
Purposes of a Nursing Care Plan: Why NCP Nursing Diagnosis Matters
The purposes and importance of nursing care plans, and particularly the ncp nursing diagnosis component, are significant:
- Defines the Nurse’s Role: Care plans, driven by ncp nursing diagnosis, highlight the nurse’s unique and independent role in addressing patients’ holistic health needs, going beyond physician directives.
- Provides Direction for Individualized Care: NCPs serve as a personalized roadmap, guiding nurses to critically develop interventions tailored to the individual patient, based on their specific ncp nursing diagnosis.
- Ensures Continuity of Care: Consistent, quality interventions across different nursing shifts and departments are facilitated by NCPs, maximizing treatment benefits for patients. This consistency is built upon a shared understanding of the patient’s ncp nursing diagnosis.
- Coordinates Care: NCPs ensure all healthcare team members are informed of patient needs and necessary actions, preventing gaps in care. The ncp nursing diagnosis acts as a common reference point for all team members.
- Documentation: NCPs accurately document observations, nursing actions, and patient/family instructions. Correctly documented ncp nursing diagnosis is essential evidence of care provided.
- Guides Staff Assignment: NCPs help assign staff with specific skills to patients with particular needs, based on the complexities identified in the ncp nursing diagnosis.
- Monitors Progress: NCPs track patient progress and facilitate necessary adjustments as health status and goals evolve, allowing for dynamic refinement of the ncp nursing diagnosis if needed.
- Supports Reimbursement: Insurance companies utilize medical records, including NCPs with documented ncp nursing diagnosis, to determine coverage for hospital care.
- Defines Patient Goals: NCPs, developed around the ncp nursing diagnosis, involve patients in their treatment, enhancing engagement and understanding.
Components of a Nursing Care Plan: Nursing Diagnosis as the Core
A typical nursing care plan (NCP) comprises several key elements, with nursing diagnoses forming the foundation. Other components include patient problems, expected outcomes, nursing interventions, and rationales.
Care Plan Formats: Structuring NCP Nursing Diagnosis within the Plan
Nursing care plan formats are commonly structured in columns, typically ranging from three to five columns. These formats are designed to organize the key components, ensuring ncp nursing diagnosis is clearly presented and linked to other elements. Common formats include three-column, four-column, and student-specific formats.
Three-Column Format: Concise NCP Organization
The three-column format neatly organizes ncp nursing diagnosis, desired outcomes/evaluation, and interventions.
Three-column nursing care plan format
Four-Column Format: Detailed NCP Structure
This format expands to include columns for ncp nursing diagnosis, goals/outcomes, interventions, and evaluation, providing a more detailed structure.
Four-column nursing care plan template
Download sample templates for various NCP formats:
Download: Printable Nursing Care Plan Templates and Formats
Student Care Plans: Emphasizing Rationale behind NCP Nursing Diagnosis
Student care plans are designed for learning and are therefore more comprehensive than those used by practicing nurses. They include a rationale column to explain the scientific basis for each intervention, deepening the understanding of ncp nursing diagnosis and its implications. Student care plans are often handwritten to reinforce the learning process.
Writing a Nursing Care Plan: A Step-by-Step Guide to NCP Nursing Diagnosis
Developing a nursing care plan involves a systematic series of steps, with ncp nursing diagnosis as a central element. Follow these steps to create an effective care plan:
Step 1: Data Collection and Patient Assessment: Gathering Information for NCP Nursing Diagnosis
The initial step is to compile a comprehensive patient database using assessment techniques and data collection methods, including physical exams, health histories, interviews, and medical record reviews. This database contains all relevant health information, crucial for identifying related factors and defining characteristics that inform the ncp nursing diagnosis. Specific assessment formats may be required by agencies or nursing schools.
Critical thinking is paramount during patient assessment. Integrating scientific knowledge and professional guidelines is vital to inform evaluations and support complex clinical decision-making, ultimately leading to accurate ncp nursing diagnosis.
Step 2: Data Analysis and Organization: Structuring Data for NCP Nursing Diagnosis
After gathering patient data, the next step involves analyzing, clustering, and organizing this information to formulate ncp nursing diagnoses, prioritize needs, and define desired outcomes. This structured approach ensures that the ncp nursing diagnosis is well-supported by evidence.
Step 3: Formulating Nursing Diagnoses: Defining the NCP Nursing Diagnosis
Nursing diagnoses are standardized statements that identify specific patient needs and responses to actual or potential health problems. They are health issues that nurses can independently address. This step is crucial for establishing the ncp nursing diagnosis.
For a detailed guide on formulating nursing diagnoses, refer to: Nursing Diagnosis (NDx): Complete Guide and List.
Step 4: Setting Priorities: Prioritizing NCP Nursing Diagnoses
Prioritizing involves ranking nursing diagnoses and interventions. Nurses collaborate with patients to determine which problems require immediate attention. Diagnoses are categorized as high, medium, or low priority, with life-threatening issues taking precedence. This prioritization is applied to the ncp nursing diagnoses identified.
Maslow’s Hierarchy of Needs is a helpful framework for prioritizing ncp nursing diagnoses. Basic physiological needs must be addressed before higher-level needs. Physiological and safety needs are foundational in nursing care.
Maslow’s Hierarchy of Needs:
- Basic Physiological Needs: Nutrition, elimination, airway, breathing, circulation, sleep, shelter, exercise.
- Safety and Security: Injury prevention, trust, patient education.
- Love and Belonging: Supportive relationships, social interaction, therapeutic communication.
- Self-Esteem: Community acceptance, personal achievement, empowerment.
- Self-Actualization: Empowering environment, spiritual growth, reaching potential.
*Virginia Henderson’s 14 Needs as applied to Maslow’s Hierarchy of Needs. Learn more about it here. *
Patient values, beliefs, resources, and urgency are crucial considerations when prioritizing ncp nursing diagnoses. Patient involvement in this process enhances cooperation.
Step 5: Establishing Client Goals and Desired Outcomes: Setting Goals Based on NCP Nursing Diagnosis
Once ncp nursing diagnoses are prioritized, nurses and patients collaborate to set goals for each diagnosis. Goals and desired outcomes define what the nurse aims to achieve through interventions derived from the ncp nursing diagnosis. Goals guide intervention planning, provide evaluation criteria, and motivate both patient and nurse.
Examples of goals and desired outcomes.
One overall goal is established per ncp nursing diagnosis. Goals should be SMART: Specific, Measurable, Attainable, Realistic, and Time-oriented. They should also adhere to REEPIG standards: Realistic, Explicitly stated, Evidence-based, Prioritized, Involve patient and team, Goal-centered. Goals can be short-term or long-term, depending on the care setting and patient needs.
Goals and desired outcomes must be measurable and patient-centered, focusing on problem resolution, prevention, and rehabilitation, all guided by the ncp nursing diagnosis.
Components of Goals and Desired Outcomes:
Components of goals and desired outcomes in a nursing care plan.
Goals typically include a subject (patient), verb (action), conditions/modifiers, and criteria of desired performance. Goals should be written in terms of patient responses, be realistic, compatible with other therapies, and derived from a single ncp nursing diagnosis. Patient involvement in goal setting is essential.
Step 6: Selecting Nursing Interventions: Actions to Address NCP Nursing Diagnosis
Nursing interventions are actions nurses take to achieve patient goals, directly addressing the etiology of the ncp nursing diagnosis. For risk diagnoses, interventions focus on reducing risk factors. Interventions are planned during the nursing process planning phase but implemented during the implementation phase.
Types of Nursing Interventions: Tailoring Actions to NCP Nursing Diagnosis
Nursing interventions can be independent, dependent, or collaborative.
Types of nursing interventions in a care plan.
- Independent interventions are nurse-initiated actions based on their judgment and skills, such as assessment, emotional support, education, and referrals.
- Dependent interventions are carried out under physician orders, including medication administration, IV therapy, and specific treatments.
- Collaborative interventions involve teamwork with other healthcare professionals like physicians, social workers, and therapists, ensuring a holistic approach informed by the ncp nursing diagnosis.
Interventions should be safe, appropriate, achievable, and aligned with patient values and other therapies. They must be grounded in nursing knowledge and evidence-based practices, directly addressing the ncp nursing diagnosis. Interventions should be specific, clearly stated with action verbs, and dated and signed for accountability.
Evidence-Based Practice: Guiding Intervention Selection for NCP Nursing Diagnosis
When selecting interventions, evidence-based guidelines and consensus statements relevant to the patient’s condition are invaluable. For example, heart failure guidelines inform interventions such as daily weight checks and sodium-restricted diets. Diabetes guidelines guide blood glucose monitoring and foot care routines. These guidelines ensure interventions are effective and aligned with best practices for each ncp nursing diagnosis.
Step 7: Providing Rationale: Explaining the “Why” Behind Interventions for NCP Nursing Diagnosis
Rationales, or scientific explanations, justify the selected nursing interventions, linking them back to the ncp nursing diagnosis. While not always included in regular care plans, rationales are crucial for student nurses to connect interventions with pathophysiological and psychological principles underlying the ncp nursing diagnosis.
Step 8: Evaluation: Assessing the Effectiveness of NCP Nursing Diagnosis and Interventions
Evaluation is an ongoing process to assess patient progress toward goals and the effectiveness of the nursing care plan. It determines whether interventions should continue, be modified, or terminated, based on the outcomes related to the ncp nursing diagnosis. Evaluation is a critical phase of the nursing process.
Step 9: Documentation: Putting the NCP Nursing Diagnosis on Paper
The patient’s care plan is documented according to hospital policy and becomes part of their permanent medical record. This documentation, including the clearly stated ncp nursing diagnosis, is essential for communication among healthcare providers and for continuity of care. Various nursing programs and healthcare facilities utilize different care plan formats.
Nursing Care Plan List: Examples of NCP Nursing Diagnoses in Practice
This section provides a comprehensive list of sample nursing care plans (NCPs) and nursing diagnoses for various health conditions, categorized for easy navigation. These examples illustrate the practical application of ncp nursing diagnosis in diverse clinical scenarios.
(The original list of nursing care plans is included here as in the original article.)
Recommended Resources: Enhancing Your Understanding of NCP Nursing Diagnosis
(The original list of recommended resources is included here as in the original article.)
References and Sources
(The original list of references and sources is included here as in the original article.)