Primary care physicians are at the forefront of managing chronic conditions, and hypercholesterolemia, particularly familial hypercholesterolemia (FH), presents a significant challenge in this setting. Effective diagnosis and management are crucial to reducing the risk of cardiovascular disease (CVD) in these patients. This article examines the impact of primary care-led follow-up and management on patients with phenotypic FH, highlighting key strategies for improved patient outcomes.
A study encompassing 133 patients with phenotypic FH, including newly diagnosed cases from targeted screening and those identified through routine clinical assessment, investigated the effectiveness of primary care management. The baseline characteristics of these patients, as detailed in Table 1, revealed a middle-aged, overweight population with mild hypercholesterolemia. Notably, a significant proportion had existing CVD events (44%) and a strong family history of premature coronary artery disease (CAD) (85%). A substantial number were current or former smokers (53%). At baseline, a majority were on statin therapy, either alone or in combination with ezetimibe, with an average atorvastatin equivalent dose of 50.9 mg/day. However, only 65% achieved the target 50% reduction in LDL-cholesterol, and a mere 16% reached recommended absolute LDL-cholesterol targets.
[Inline Image: Table 1 Baseline clinical and biochemical characteristics of the 133 patients with phenotypic familial hypercholesterolaemia. This table likely summarizes key metrics like age, BMI, cholesterol levels, blood pressure, smoking status, CVD history, and family history of CAD for the study participants at the beginning of the study.]
The follow-up phase of the study focused on 77 patients who attended at least one follow-up consultation with their primary care physician and had LDL-cholesterol measurements taken. This group was representative of the initial cohort, with no significant differences in baseline characteristics compared to those lost to follow-up. Over an average follow-up period of 221 days, a significant number of interventions were implemented by the primary care physicians.
A notable 36% of patients received intensified lipid-lowering therapy, with new statin initiation or up-titration of existing statin doses being the most common approaches. Furthermore, 26% received lifestyle modification advice, and a smaller proportion (5.2%) were referred to specialists. Interestingly, patients who did not achieve the 50% LDL-cholesterol reduction target at baseline were more likely to receive intensified treatment, although this trend did not reach statistical significance. It’s important to note that lifestyle advice alone, in a subset of patients, did not result in significant changes in total or LDL-cholesterol levels.
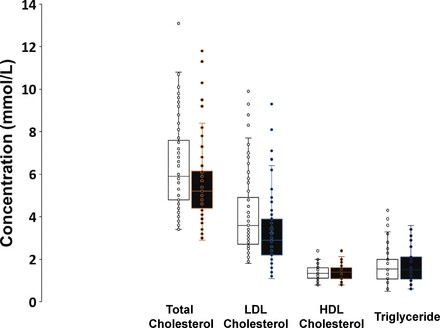
However, the overall impact of primary care management was evident in the significant reductions observed in plasma total cholesterol and LDL-cholesterol levels from baseline to follow-up (Figure 3). The study demonstrated a 9.4% reduction in total cholesterol and a 16% reduction in LDL-cholesterol levels in patients under primary care management (p<0.0001).
[Inline Image: Figure 3 Plasma lipid concentrations in patients before and after primary care management showing reductions in total and LDL cholesterol.]
Figure 4 further illustrates the percentage changes in LDL-cholesterol concentrations, highlighting the impact of intensified statin therapy. Patients who received increased intensity statin treatment showed a greater reduction in LDL-cholesterol compared to those without treatment intensification.
[Inline Image: Figure 4 Percentage changes in LDL-cholesterol levels in patients with and without increased statin intensity for hypercholesterolemia management.]
The success of primary care management is further underscored by the improved attainment of LDL-cholesterol targets (Figure 5). A significantly higher proportion of patients achieved the 50% LDL-cholesterol reduction target after primary care management (74% vs 62%, p<0.05). Moreover, a substantial number of patients who were above the LDL-cholesterol treatment cut-off at baseline successfully reached their target levels following follow-up consultations in primary care.
[Inline Image: Figure 5 Achievement of LDL-cholesterol reduction targets after primary care interventions for hypercholesterolemia patients.]
Beyond individual patient management, the study also highlighted the crucial role of primary care in cascade screening. An average of 4.7 first-degree or second-degree relatives per index case were identified as needing cascade screening, emphasizing the broader public health impact of effective FH diagnosis and management within primary care.
In conclusion, this study demonstrates the significant positive impact of primary care-led diagnosis and management of hypercholesterolemia, particularly phenotypic FH. Through appropriate intensification of lipid-lowering therapy and lifestyle advice, primary care physicians can effectively reduce LDL-cholesterol levels and improve target attainment in these high-risk patients. Furthermore, primary care plays a vital role in identifying family members at risk through cascade screening. These findings underscore the importance of robust systems within primary care to facilitate the effective diagnosis and ongoing management of hypercholesterolemia to mitigate the long-term risk of cardiovascular disease.