Establishing an accurate diagnosis of pulpal and periapical conditions is fundamental in dentistry. It dictates the appropriate clinical treatment, ensuring patients receive the necessary care while avoiding unnecessary procedures. Historically, endodontic diagnosis was often based on histopathological findings, leading to inconsistencies and confusion. To address this, the American Association of Endodontists (AAE) convened a consensus conference in 2008 to standardize diagnostic terminology. This article serves as your essential Aae Endo Diagnosis Chart guide, detailing these standardized terms and their clinical applications for effective endodontic practice.
A universal and clinically relevant diagnostic system is crucial for clear communication among dental professionals – from educators and clinicians to students and researchers. This standardized approach, endorsed by both the AAE and the American Board of Endodontics, utilizes terms grounded in clinical findings, promoting a shared understanding of pulpal and periapical diseases and guiding appropriate treatment strategies. This article will explore each diagnostic term, outlining typical clinical and radiographic characteristics and providing illustrative case examples. Remember, pulpal and periapical diseases are dynamic, and their presentation can vary based on the disease stage and individual patient factors. A comprehensive endodontic diagnosis necessitates evaluating both pulpal and periapical status for each tooth.
Examination and Diagnostic Procedures: Piecing Together the Puzzle
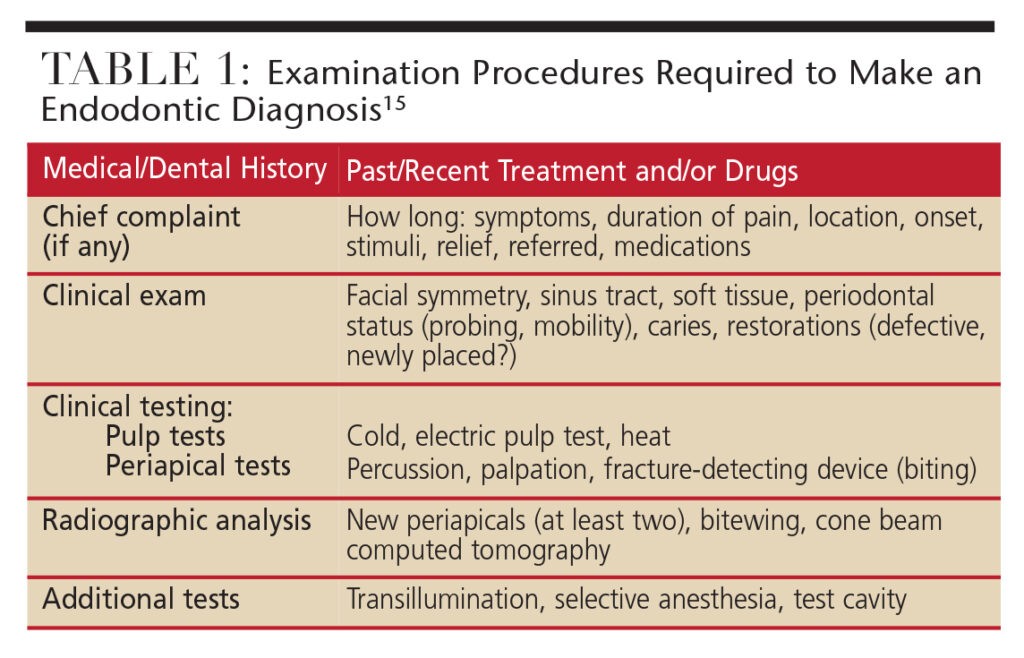
Endodontic diagnosis is a comprehensive process, much like assembling a jigsaw puzzle. No single piece of information is sufficient for a definitive diagnosis. As illustrated in Figure 1, a systematic approach to information gathering is essential. This involves a detailed medical and dental history, clinical and radiographic examinations, a thorough periodontal evaluation, and specific pulp and periapical tests. A preliminary diagnosis should begin to form during history taking, especially when a chief complaint is present. Clinical and radiographic findings, coupled with testing, serve to confirm or refine this initial assessment. In cases where examinations yield inconclusive or conflicting results, definitive diagnoses may be elusive. It is paramount to avoid treatment without a clear diagnosis. In such situations, patient reassessment or referral to an endodontist is advisable.
 Diagnostic Procedures
Diagnostic Procedures
Figure 1: A systematic approach to endodontic diagnosis is crucial, incorporating patient history, clinical examination, radiographic assessment, and pulp/periapical testing.
AAE Endodontic Diagnostic Terminology: Pulpal Diagnoses Explained
The AAE and American Board of Endodontics have established specific diagnostic terms for pulpal conditions, providing a clear framework for assessment and treatment planning. Below is a breakdown of these pulpal diagnoses, forming a core component of the AAE endo diagnosis chart.
Normal Pulp
Normal Pulp signifies a clinically healthy pulp, free from symptoms and exhibiting normal responsiveness to pulp testing. While histologically the pulp might not be perfectly normal, clinically, it presents with a mild and transient response to thermal (cold) testing, lasting no more than 1-2 seconds after stimulus removal. Crucially, diagnosis requires comparison with adjacent and contralateral teeth to establish a baseline normal response for the patient.
Reversible Pulpitis
Reversible Pulpitis indicates pulp inflammation that is expected to resolve, allowing the pulp to return to its normal state once the causative factor is addressed. Patients typically experience discomfort upon stimulation (e.g., cold or sweet), which subsides quickly within seconds of stimulus removal. Common causes include exposed dentin (dentinal sensitivity), caries, or recent restorations. Radiographically, the periapical region appears normal, and pain is not spontaneous. After managing the cause (e.g., caries removal and restoration), re-evaluation is necessary to confirm pulp normalization. Dentinal sensitivity, though not strictly inflammatory, often mimics reversible pulpitis symptoms.
Symptomatic Irreversible Pulpitis
Symptomatic Irreversible Pulpitis describes a vital, inflamed pulp incapable of healing, necessitating root canal treatment. Key characteristics include sharp pain upon thermal stimulus, lingering pain (often 30 seconds or longer post-stimulus), spontaneous pain (unprovoked), and referred pain. Pain may be exacerbated by postural changes. Over-the-counter analgesics are usually ineffective. Common causes include deep caries, extensive restorations, or fractures exposing the pulp. Diagnosis can be challenging as periapical involvement may be absent initially, resulting in no percussion pain. Patient history and thermal testing are paramount in assessing pulpal status in these cases.
Asymptomatic Irreversible Pulpitis
Asymptomatic Irreversible Pulpitis is diagnosed when a vital, inflamed pulp is deemed incapable of healing, requiring root canal treatment, but without clinical symptoms. Thermal testing responses are usually normal, but a history of trauma or deep caries suggests likely pulp exposure upon caries removal.
Pulp Necrosis
Pulp Necrosis indicates pulp death, mandating root canal treatment. The pulp is unresponsive to pulp testing and asymptomatic. Necrosis alone doesn’t cause apical periodontitis unless infection is present. False-negative pulp tests can occur due to calcification, recent trauma, or general patient non-responsiveness. Comparative testing with other teeth is essential to account for patient-specific factors.
Previously Treated
Previously Treated denotes a tooth that has undergone endodontic treatment with canals obturated with filling materials (excluding intracanal medicaments). These teeth typically do not respond to thermal or electric pulp testing.
Previously Initiated Therapy
Previously Initiated Therapy applies to teeth with partial endodontic treatment, such as pulpotomy or pulpectomy. Pulp testing responses may vary depending on the extent of the prior treatment.
AAE Endodontic Diagnosis Chart: Apical Diagnoses Defined
Just as crucial as pulpal diagnosis is the assessment of periapical tissues. The AAE’s standardized terminology extends to apical conditions, completing the AAE endo diagnosis chart.
Normal Apical Tissues
Normal Apical Tissues are characterized by no sensitivity to percussion or palpation. Radiographically, the lamina dura is intact, and the periodontal ligament space is uniform. Comparative testing with normal teeth is essential for percussion and palpation assessments.
Symptomatic Apical Periodontitis
Symptomatic Apical Periodontitis represents inflammation of the apical periodontium, causing painful responses to biting, percussion, and/or palpation. Radiographic changes may or may not be present depending on the disease stage. Severe percussion/palpation pain strongly suggests pulp degeneration and the need for root canal treatment.
Asymptomatic Apical Periodontitis
Asymptomatic Apical Periodontitis involves inflammation and destruction of the apical periodontium of pulpal origin. It is identified by an apical radiolucency but lacks clinical symptoms like percussion or palpation pain.
Chronic Apical Abscess
Chronic Apical Abscess is an inflammatory reaction to pulpal infection and necrosis, characterized by gradual onset, minimal discomfort, and intermittent pus discharge through a sinus tract. Radiographic signs of osseous destruction (radiolucency) are typical. Tracing a sinus tract with a gutta-percha cone and radiograph helps identify the source.
Acute Apical Abscess
Acute Apical Abscess is an inflammatory response to pulpal infection and necrosis with rapid onset, spontaneous pain, extreme tenderness to pressure, pus formation, and tissue swelling. Radiographic signs may be absent initially. Systemic symptoms like malaise, fever, and lymphadenopathy can occur.
Condensing Osteitis
Condensing Osteitis is a localized bony reaction to a low-grade inflammatory stimulus, appearing radiographically as a diffuse radiopaque lesion at the tooth apex.
Diagnostic Case Examples: Applying the AAE Endo Diagnosis Chart
To illustrate the practical application of the AAE endo diagnosis chart, consider these diagnostic case examples:
Case 1 (Figure 2): A mandibular first molar exhibits no response to thermal testing but is tender to biting and percussion. Radiographs show diffuse radiopacities around the root apices.
Figure 2: Radiographic presentation of condensing osteitis around the apex of a mandibular molar.
Diagnosis: Pulp necrosis; symptomatic apical periodontitis with condensing osteitis. Treatment: Nonsurgical root canal therapy is indicated.
Case 2: A maxillary second molar, recently crowned, presents with lingering pain to cold stimulus (12 seconds). Percussion and palpation are normal, and radiographs show no osseous changes.
Diagnosis: Symptomatic irreversible pulpitis; normal apical tissues. Treatment: Nonsurgical root canal treatment is needed.
Case 3: A maxillary first molar with occlusal-mesial caries shows hypersensitivity to cold but no lingering pain or percussion tenderness.
Diagnosis: Reversible pulpitis; normal apical tissues. Treatment: Caries excavation and permanent restoration.
Case 4 (Figure 3): A mandibular lateral incisor with a history of trauma and slight discoloration shows an apical radiolucency. It is non-responsive to pulp testing, but adjacent teeth respond normally. No percussion or palpation tenderness is present.
Figure 3: Apical radiolucency associated with a mandibular incisor, indicative of asymptomatic apical periodontitis.
Diagnosis: Pulp necrosis; asymptomatic apical periodontitis. Treatment: Nonsurgical root canal therapy, followed by bleaching if desired.
Case 5: A mandibular first molar exhibits a large apical radiolucency, furcation involvement, and a draining sinus tract. It is non-responsive to pulp testing, and percussion/palpation are normal.
Diagnosis: Pulp necrosis; chronic apical abscess. Treatment: Crown removal, nonsurgical root canal treatment, and new crown placement.
Case 6 (Figure 4): A maxillary first molar, previously treated endodontically, presents with biting pain and apical radiolucencies. Percussion tenderness is noted.
Figure 4: Periapical radiolucencies around a previously treated maxillary molar, suggesting symptomatic apical periodontitis.
Diagnosis: Previously treated; symptomatic apical periodontitis. Treatment: Nonsurgical endodontic retreatment.
Case 7: A maxillary lateral incisor with an apical radiolucency is asymptomatic and non-responsive to pulp testing. Adjacent teeth respond normally, and no percussion/palpation tenderness is present.
Diagnosis: Pulp necrosis; asymptomatic apical periodontitis. Treatment: Nonsurgical root canal therapy.
Conclusion: Mastering the AAE Endo Diagnosis Chart for Optimal Patient Care
Utilizing the AAE endo diagnosis chart and standardized terminology is essential for accurate pulpal and periapical diagnosis, directly impacting appropriate clinical treatment decisions. This universal system, endorsed by leading endodontic organizations, promotes clear communication and consistent patient care. However, remember that pulpal and periapical diseases are dynamic. Clinicians must integrate this diagnostic framework with careful clinical judgment, recognizing the limitations of diagnostic tests and the progressive nature of these conditions. Accurate diagnosis is built upon comprehensive data, not isolated findings. When diagnostic uncertainty arises, referral to an endodontic specialist is always the prudent course of action, ensuring patients receive expert evaluation and care.
References
- Glickman GN. AAE consensus conference on diagnostic terminology: background and perspectives. J Endod. 2009;35:1619.
- Seltzer S, Bender IB, Ziontz M. The dynamics of pulp inflammation: correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol. 1963;16:846–871;969–977.
- Berman LH, Hartwell GR. Diagnosis. In: Cohen S, Hargreaves KM, eds. Pathways of the Pulp, 11th ed. St. Louis, MO: Mosby/Elsevier; 2011:2–39.
- Schweitzer JL. The endodontic diagnostic puzzle. Gen Dent. 2009;57(6):560–567.
- AAE Consensus Conference Recommended Diagnostic Terminology. J Endod. 2009;35:1634.
- American Association of Endodontists. Glossary of Endodontic Terms. 8th ed. 2012.
- Glickman GN, Bakland LK, Fouad AF, Hargreaves KM, Schwartz SA. Diagnostic terminology: report of an online survey. J Endod. 2009;35:1625.
- Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part I: general information and thermal tests. Int Endod J. 2010;43:738–762.
- Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part II: electric pulp tests and test cavities. Int Endod J. 2010;43:945–958.
- Newton CW, Hoen MM, Goodis HE, Johnson BR, McClanahan SB. Identify and determine the metrics, hierarchy, and predictive value of all the parameters and/or methods used during endodontic diagnosis. J Endod. 2009;35:1635.
- Levin LG, Law AS, Holland GR, Abbot PV, Roda RS. Identify and define all diagnostic terms for pulpal health and disease states. J Endod. 2009;35:1645.
- Gutmann JL, Baumgartner JC, Gluskin AH, Hartwell GR, Walton RE. Identify and define all diagnostic terms for periapical/periradicular health and disease states. J Endod. 2009;35:1658.
- Rosenberg PA, Schindler WG, Krell KV, Hicks ML, Davis SB. Identify the endodontic treatment modalities. J Endod. 2009;35:1675.
- Green TL, Walton RE, Clark JM, Maixner D. Histologic examination of condensing osteitis in cadaver specimens. J Endod. 2013;39:977–979.
- Abbott PV, Yu C. A clinical classification of the status of the pulp and the root canal system. Aust Dent J. 2007;52(Endod Suppl):S17–S31.