I. Understanding Abdominal Bloating and Distention
Abdominal bloating is a widespread complaint affecting individuals across all demographics. Characterized by a subjective sensation of fullness, tightness, or trapped gas in the abdomen, bloating is a frequent symptom reported by patients seeking medical advice. It is particularly prevalent in conditions like irritable bowel syndrome (IBS), where it affects the vast majority of patients, and is also observed in various other functional and organic gastrointestinal (GI) disorders. Bloating can significantly impact a patient’s quality of life, causing considerable discomfort and frustration for both patients and healthcare providers due to the often limited and inconsistent effectiveness of available treatments.
While the terms “bloating” and “abdominal distention” are often used interchangeably in clinical practice, it is crucial to recognize that they likely represent distinct underlying physiological processes. Abdominal distention refers to an objective, measurable increase in abdominal girth, whereas bloating is a subjective perception that does not necessarily correlate with visible distention. Both bloating and distention are complex symptoms whose exact mechanisms are not fully elucidated, though significant progress has been made in recent years to better understand these common and often debilitating conditions. This article aims to provide a detailed review of the pathophysiology, comprehensive evaluation, and current treatment strategies for abdominal bloating and distention, with a particular focus on Abdominal Bloating Differential Diagnosis.
II. Defining Bloating and Abdominal Distention: Nuances in Terminology
Bloating, in a clinical context, is best defined as the subjective sensation of trapped gas, abdominal fullness, or a feeling of being swollen. It is important to emphasize that this sensation exists irrespective of any objective, measurable abdominal distention. The Rome IV criteria, the current standard for diagnosing functional gastrointestinal disorders, provide a framework for functional bloating, defining it as a recurrent feeling of bloating or visible distention experienced at least three days per month. The onset of these symptoms must be at least six months prior to diagnosis, with symptom presence for at least three months. Critically, these symptoms should not meet the diagnostic criteria for other functional GI disorders such as IBS or functional dyspepsia.
Abdominal distention, on the other hand, should be reserved to describe a visible and measurable increase in abdominal girth. Ambulatory monitoring studies using abdominal inductance plethysmography have demonstrated natural fluctuations in abdominal girth throughout the day in healthy individuals, typically increasing postprandially and decreasing overnight. These fluctuations are often exaggerated in patients with IBS, who also tend to be more symptomatic in relation to these changes in girth. Therefore, while bloating is a symptom, abdominal distention is a physical sign that may or may not accompany bloating. Understanding this distinction is important in approaching the differential diagnosis of abdominal bloating.
Table 1. Rome IV Criteria for Functional Bloating
| – Recurrent feeling of bloating or visible distention for at least 3 days per month |
| – Onset of symptoms at least 6 months prior to diagnosis |
| – Presence of symptoms for at least 3 months |
| – Insufficient criteria to diagnose irritable bowel syndrome, functional dyspepsia, or any other functional gastrointestinal disorder |
Modified from Drossman DA, et al. Rome IV. Bristol, UK: Rome Foundation; 2016.
Burping and belching, while often associated with bloating, are distinct phenomena. These actions represent the expulsion of excess gas primarily from the stomach. It’s important to differentiate these from bloating and distention during patient consultations. Belching and burping are often linked to aerophagia, or air swallowing, which can be a conscious or subconscious habit, rather than the complex intestinal processes that contribute to bloating and abdominal distention. Therefore, a detailed patient history is crucial to accurately categorize and understand the patient’s specific complaints, guiding the abdominal bloating differential diagnosis process.
III. Epidemiology and Natural History of Bloating
Epidemiological studies reveal that a significant portion of the general population experiences bloating symptoms. Surveys conducted in the United States have indicated that 15% to 30% of adults report experiencing bloating. While early studies were limited by demographic diversity, more recent research in Asian populations using similar validated questionnaires has shown comparable prevalence rates, suggesting that bloating is a global health concern.
While population-based studies have not definitively established a sex predisposition for bloating, investigations within IBS cohorts consistently demonstrate a higher prevalence of bloating among women compared to men. In IBS studies, bloating prevalence ranges from 66% to 90%, with women often reporting this symptom more frequently. Furthermore, individuals with constipation-predominant IBS are more likely to experience bloating compared to those with diarrhea-predominant IBS.
The impact of bloating on patient well-being is significant, regardless of gender or underlying cause. In individuals experiencing bloating without IBS, over 75% characterize their symptoms as moderate to severe, and more than half report limiting their daily activities due to bloating. In IBS patients, bloating has been identified as an independent predictor of IBS severity, highlighting its clinical importance.
The long-term course of bloating is not well-defined. A longitudinal study following patients with functional dyspepsia over five years showed only a modest correlation in self-reported bloating symptoms over time, suggesting the fluctuating and potentially episodic nature of bloating for some individuals. Further research is needed to fully understand the natural history of bloating and its progression.
IV. Pathophysiology: Unraveling the Mechanisms of Bloating
The pathophysiology of bloating and intestinal gas is intricate and multifactorial. A comprehensive understanding requires considering the gut microbiota, gas production dynamics, intestinal transit, gas propulsion, and visceral sensory function. It is also important to consider behavioral factors, such as eating disorders and aerophagia, which can contribute to gas and bloating symptoms and should be included in the differential diagnosis of abdominal bloating (Table 2).
Table 2. Differential Diagnosis of Abdominal Gas, Bloating, and Distention
| – Aerophagia |
| – Anorexia and bulimia |
| – Gastroparesis |
| – Gastric outlet obstruction (partial or complete) |
| – Functional bloating |
| – Functional dyspepsia |
| – Dietary factors |
| – Lactose intolerance |
| – Fructose intolerance |
| – Fructan consumption |
| – Consumption of sorbitol or other nonabsorbable sugars |
| – Carbohydrate intake |
| – Gluten sensitivity |
| – Celiac disease |
| – Chronic constipation |
| – Irritable bowel syndrome |
| – Disturbances in colonic microflora |
| – Small intestinal bacterial overgrowth (SIBO) |
| – Abnormal small intestinal motility (e.g., scleroderma) |
| – Small bowel diverticulosis |
| – Abnormal colonic transit |
| – Evacuation disorders of the pelvic floor |
A. The Gut Microbiota: A Key Player in Gas Production
The gut microbiota, or microbiome, refers to the vast community of microorganisms, predominantly bacteria, residing in the intestinal tract. These microorganisms and their metabolic byproducts exert significant influence on GI function and overall health. The colon alone harbors an estimated 500 different bacterial species, primarily anaerobes. The composition of the gut microbiota is highly individualized, influenced by factors such as diet, antibiotic exposure, and infant feeding methods. The sheer number of bacteria in the GI tract is staggering, exceeding the total number of human cells in the body.
Research over the past decade has underscored the crucial role of the gut microbiota in various physiological processes, including immune function, mucosal barrier integrity, drug metabolism, and the production of short-chain fatty acids and vitamins. Even subtle disruptions in the gut microbiota, termed dysbiosis, can lead to significant alterations in gut function, including changes in gas production. While the total volume of gas produced may not vary dramatically between individuals, the composition of the gas (e.g., methane, hydrogen, carbon dioxide) can differ significantly, potentially impacting intestinal transit and visceral sensation. These microbial factors are important considerations within the abdominal bloating differential diagnosis.
B. Normal Intestinal Gas Dynamics
Under normal physiological conditions, the average person carries approximately 100 to 200 cc of gas within their GI tract at any given time. The volume of intestinal gas naturally increases after meals, particularly in the pelvic colon. Postprandial gastric distention and small bowel stimulation facilitate gas transit. Conversely, intraluminal lipids tend to slow gas transit, primarily in the proximal small intestine.
Colonic gas production is primarily a result of bacterial fermentation of undigested food products. Carbohydrates that escape digestion in the small intestine, such as lactose (in lactase deficiency), fructose, sorbitol, legumes (containing stachyose and raffinose), fiber, and complex carbohydrates (e.g., wheat), are broken down by colonic bacteria, leading to gas production. Other sources of intestinal gas include swallowed air, diffusion from the bloodstream, and chemical reactions within the GI tract.
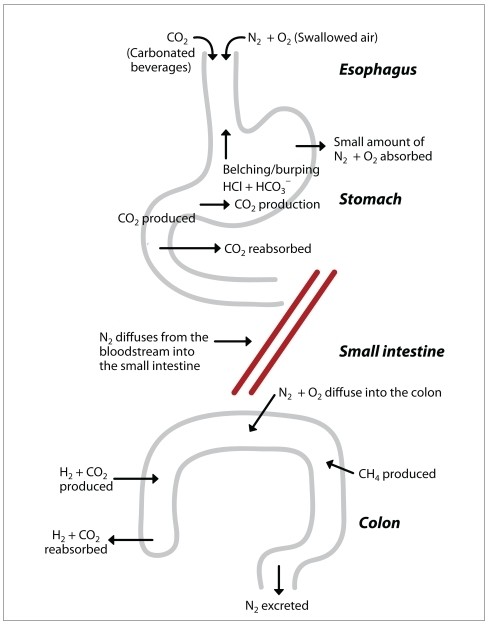
The five most abundant gases in the GI tract are nitrogen (N2), oxygen (O2), hydrogen (H2), carbon dioxide (CO2), and methane (CH4), along with trace amounts of other gases. Nitrogen and oxygen in the upper GI tract largely originate from swallowed air. Carbon dioxide can come from swallowed air, carbonated beverages, or the neutralization of acids and bases in the upper GI tract. CO2 is readily absorbed in the small intestine. Studies have shown that a healthy individual produces around 700 cc of gas per day, primarily CO2 and H2 in the colon.
Many individuals also harbor methanogenic bacteria in their colon. These bacteria consume hydrogen and produce methane, as well as small amounts of sulfur-containing gases like hydrogen sulfide and methanethiol. Conversely, numerous colonic bacterial species consume both hydrogen and carbon dioxide, effectively reducing the overall gas content in the large intestine. Healthy individuals typically pass flatus 14 to 18 times daily, with a total volume ranging from 214 mL on a low-fiber diet to 705 mL on a high-fiber diet over 24 hours. It’s important to note that, contrary to common belief, IBS patients do not typically produce more intestinal gas than healthy individuals.
Figure 1. The Physiology of Intestinal Gas
Physiology of intestinal gas, primarily derived from ingested food and swallowed air. Large amounts of carbon dioxide (CO2) are produced in the small intestine as a digestive byproduct, with significant reabsorption in the small intestine. Hydrogen (H2) and CO2 are produced in substantial quantities in the colon, with a portion being reabsorbed. Methanogenic bacteria consume H2 and release methanethiol and hydrogen sulfide.
CH4=methane; HCl=hydrochloric acid; HCO3–=hydrogen carbonate; N2=nitrogen; O2=oxygen.
C. Abnormal Intestinal Gas: Defining the Deviation
Defining what constitutes “abnormal” intestinal gas is challenging due to several factors. There is a lack of standardized definitions and reliable diagnostic tests to differentiate normal from abnormal gas production levels. While abdominal radiographs are often used, they provide limited information about gas production, composition, or evacuation. Breath hydrogen tests, while commonly used, have limitations in specificity and sensitivity. Furthermore, as bloating is primarily a sensory phenomenon, its objective measurement in clinical practice is inherently limited. Therefore, when considering abdominal bloating differential diagnosis, it’s crucial to move beyond simply quantifying gas volume and focus on the patient’s symptomatic experience and potential underlying mechanisms.
D. Concomitant Symptoms: Unpacking Bloating and Distention
Healthy individuals generally tolerate intestinal gas without significant symptoms due to efficient gas propulsion and evacuation mechanisms. Several theories attempt to explain why some individuals develop bloating and distention.
1. Increased Gas Production: A Largely Discounted Theory
The notion that excessive gas production is the primary cause of bloating has been largely refuted. Studies employing various techniques, such as argon washout and labeled sulfur hexafluoride, have consistently failed to demonstrate significant differences in gas production between healthy individuals and IBS patients. Moreover, infusing substantial amounts of gas (2160 mL) into the intestines of healthy volunteers results in only minimal changes in abdominal girth (less than 2 cm). In contrast, IBS patients often exhibit more pronounced abdominal girth changes even without gas infusion, suggesting factors beyond simple gas volume are at play.
2. Impaired Gas Transit: A Significant Contributor
Research over two decades ago highlighted the role of impaired intestinal transit in some IBS patients, potentially contributing to bloating and gas symptoms. This is particularly relevant in constipation-predominant IBS, where bloating is highly prevalent. While a small study investigating intestinal gas infusions did not reveal differences in small bowel motility between IBS patients and healthy controls, IBS patients reported significantly more pain during both actual and sham gas infusions, indicating heightened visceral sensitivity. A larger study demonstrated that a significantly higher proportion of IBS patients experienced intestinal gas retention compared to healthy controls, and abdominal distention correlated with gas retention. Furthermore, IBS patients exhibited impaired gas clearance from the proximal colon compared to healthy individuals, mirroring earlier findings of impaired small intestinal gas clearance. This impaired transit may reflect abnormalities in intrinsic reflexes or heightened sensitivity to lipids.
3. Impaired Evacuation: Difficulty in Gas Expulsion
Some individuals experience difficulty in effectively evacuating intestinal gas, leading to prolonged gas retention and symptoms of bloating and pain. Patients with IBS, functional bloating, and constipation are less efficient at evacuating infused gas and are more prone to developing abdominal distention. Some of these patients appear to have deficits in the normal rectal reflex involved in gas propulsion.
4. Abnormal Abdominal-Diaphragmatic Reflexes: A Musculoskeletal Component
Over six decades ago, the concept of an abnormal abdominal wall reflex in bloating patients was proposed. In healthy individuals, intestinal gas infusion triggers increased abdominal wall muscle activity. However, in bloating patients, gas infusion leads to a paradoxical decrease in abdominal wall muscle contraction coupled with inappropriate relaxation of the internal oblique muscles. This abnormal viscerosomatic reflex activity results in abdominal wall relaxation rather than contraction in response to gaseous distention, accentuating luminal gas. In contrast to healthy individuals, the diaphragms of bloating patients descend while their ventral abdominal wall muscles relax, contributing to an increase in abdominal girth.
5. Abnormalities in Posture: A Less Substantiated Factor
Anecdotal reports suggest that some patients with significant bloating and distention may unconsciously adopt a more lordotic posture. However, research in IBS patients has not consistently supported this observation, suggesting posture is not a primary factor in most cases.
6. Abnormal Sensation or Perception: Visceral Hypersensitivity
Patients with IBS exhibit heightened sensitivity to intestinal stretch and distention compared to healthy individuals. Studies have shown that IBS patients with bloating alone have lower pain thresholds to abdominal stimuli compared to those with both bloating and distention. In clinical terms, impaired gas transit and ineffective evacuation can lead to intestinal distention in a hypersensitive individual, triggering significant bloating and pain disproportionate to the actual amount of trapped gas. This visceral hypersensitivity is a critical element in understanding the differential diagnosis of abdominal bloating, particularly in functional disorders.
V. Psychosocial Aspects of Bloating
In women with IBS, bloating is frequently reported as the most prominent and severe symptom. The prevalence and severity of bloating are associated with increased healthcare utilization and reduced quality of life, particularly in women with IBS. Bloating is also a common and often severe complaint in patients with gastroparesis, and its severity is inversely correlated with patient-reported quality of life.
Psychosocial distress can amplify the perceived severity of bloating. Women with moderate to severe bloating are more likely to report a history of major depression and experience more severe depression and anxiety. Studies have shown that patients with moderate to severe bloating have significantly higher scores for anxiety, depression, and somatization on psychological symptom checklists. However, other studies have not consistently found a strong link between bloating and psychological distress, and the association may be less pronounced in functional dyspepsia. Despite some inconsistencies, it is clear that addressing psychological comorbidities is likely crucial for effective management strategies for bloating. Considering psychosocial factors is therefore an integral part of a comprehensive abdominal bloating differential diagnosis and treatment plan.
VI. Diagnosis: A Stepwise Approach to Identifying the Cause
While bloating can be a distressing symptom, it often represents a benign condition. The diagnostic process for bloating should begin with a thorough history and physical examination to rule out underlying organic disorders. Clinicians should inquire about alarm symptoms such as anemia and unintentional weight loss, which may indicate malabsorption or other serious conditions. If alarm symptoms are present, initial investigations may include a complete blood count, celiac serology, and upper endoscopy with duodenal biopsies.
Patients presenting with bloating alongside other symptoms should be evaluated accordingly. For example, coexisting nausea and vomiting may warrant small bowel imaging and gastric emptying studies, while diarrhea may necessitate stool studies and colonoscopy. Beyond excluding obstructive processes or conditions predisposing to bacterial overgrowth, routine imaging has limited value in diagnosing bloating. Studies have shown that CT scans do not reliably differentiate bloating patients from healthy controls in terms of intestinal gas volume.
Often, clinicians initiate treatment at this stage in the evaluation. However, concerns about small intestinal bacterial overgrowth (SIBO) frequently lead to empiric antibiotic therapy. The role of SIBO in bloating and its diagnosis remains a complex and debated topic, warranting careful consideration within the abdominal bloating differential diagnosis.
A. Small Intestinal Bacterial Overgrowth (SIBO): A Controversial Diagnosis
The diagnosis of SIBO remains controversial, with varying diagnostic approaches and interpretations. Many consider small intestinal culture obtained via orojejunal tube or sterile endoscopic aspiration as the gold standard. Historically, bacterial counts exceeding 105 colony-forming units (CFU)/mL have been considered diagnostic, although thresholds ranging from 104 to 107 CFU/mL have been used. However, small bowel aspiration is invasive, time-consuming, costly, and not routinely performed in many labs. Therefore, non-invasive methods are widely used for SIBO diagnosis in clinical practice.
1. Imaging: Small bowel imaging is often recommended to identify structural abnormalities that could predispose to SIBO, such as small bowel diverticula, which have been shown to increase the odds of SIBO significantly. Gastric emptying scans can identify gastroparesis in bloating patients.
2. Endoscopy: Routine endoscopy plays a limited role in SIBO diagnosis, except for obtaining sterile small bowel aspirates. Duodenal biopsies may show villous blunting, but this finding is neither sensitive nor specific for SIBO.
3. Laboratory Evaluation: No serologic test definitively diagnoses SIBO. However, vitamin levels can offer clues. SIBO can cause malabsorption of vitamin B12 and vitamin D, making it reasonable to check these levels. Elevated folate levels may also suggest SIBO, as upper intestinal bacteria can synthesize folate.
4. Breath Testing: Breath testing is the most commonly used non-invasive diagnostic test for SIBO. It is based on the principle that bacterial fermentation of non-absorbed carbohydrates produces hydrogen (H2) and methane (CH4) gas, which are then exhaled. Patients ingest a carbohydrate load, typically lactulose or glucose, and exhaled breath gases are analyzed at intervals. With lactulose, a normal response is a delayed rise in breath H2 and/or CH4 when the carbohydrate reaches the colon. With glucose, which should be absorbed in the small intestine, an early peak in breath H2 or CH4 suggests SIBO. Diagnostic criteria for a positive breath test vary, but an increase in H2 of 20 parts per million within 60-90 minutes is generally considered indicative of SIBO. Elevated fasting H2 and CH4 levels are also highly specific, but less sensitive, for SIBO. It is important to note that some individuals are non-hydrogen producers, but these individuals often produce methane. Therefore, analyzing both H2 and CH4 improves the sensitivity of breath testing.
5. Empiric Antibiotics: A therapeutic trial of antibiotics, similar to proton pump inhibitor trials for reflux, can be considered a diagnostic approach for SIBO. Empiric antibiotic use is limited by potential adverse effects, including Clostridioides difficile infection, although the risk is reduced with poorly absorbed antibiotics like rifaximin. While limited trials have specifically evaluated empiric antibiotics for SIBO diagnosis, this approach can be reasonable in patients with SIBO-suggestive symptoms or predisposing conditions (e.g., scleroderma, ileocecal valve resection). However, potential for antibiotic resistance and other side effects must be weighed. Rifaximin, however, has demonstrated adverse effect profiles similar to placebo in studies.
VII. Treatment Strategies for Bloating
A standardized, evidence-based treatment algorithm for bloating and abdominal distention is lacking. Therefore, individualized treatment plans are crucial. A stepwise approach, developed collaboratively with the patient, is often most effective to enhance compliance. The initial step is to identify the predominant symptom: bloating, distention, or both. This may offer insights into underlying mechanisms. Patient education regarding potential pathophysiological processes is essential, followed by reassurance that these symptoms, while bothersome, are typically benign. Finally, realistic and specific treatment goals should be established. The following section outlines current evidence-based treatment options for bloating (Table 3). It is important to note that large, randomized controlled trials specifically focusing on functional bloating are limited, and much of the available data comes from IBS studies.
Table 3. Treatment Options for Bloating
| – Diet |
| – Exercise and posture |
| – Over-the-counter medications |
| – Probiotics |
| – Antibiotics |
| – Smooth muscle antispasmodics |
| – Osmotic laxatives |
| – Prokinetic agents |
| – Chloride channel activators |
| – Tricyclic antidepressants (TCAs) |
A. Dietary Modifications
A detailed dietary history is essential, focusing on fermentable foods such as dairy, fructose, fructans, fiber, and sorbitol. The low-FODMAP diet, restricting fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, has shown benefit in improving bloating in IBS patients. Dietary modifications are often implemented stepwise, removing one potential trigger at a time (e.g., dairy, then fructose, then fiber). Some patients with severe bloating may opt for a strict elimination diet initially, gradually reintroducing food groups. Some patients report symptom improvement with carbohydrate and gluten restriction, although robust evidence for these approaches is limited.
B. Exercise and Posture
Studies have shown that physical exercise, such as stationary cycling, can improve intestinal gas clearance and reduce bloating symptoms. As gas retention is worse in the supine position, patients should be advised to exercise and minimize prolonged recumbency during the day.
C. Over-the-Counter (OTC) Medications
Activated charcoal has not been shown to alter gas production or improve abdominal symptoms in studies. Simethicone, an antifoaming agent, may offer some relief for upper abdominal bloating in limited studies, but lacks robust evidence in Rome-classified patients. α-galactosidase may reduce gas and flatus production associated with oligosaccharide-rich meals, but its efficacy for bloating related to other fermentable carbohydrates is not established.
D. Probiotics
Probiotics, defined as live microorganisms conferring health benefits, are commonly used for bloating, but many lack rigorous evaluation in randomized, placebo-controlled trials. Some studies suggest benefit from specific probiotic strains. Lactobacillus acidophilus and Bifidobacterium lactis have shown improvement in bloating severity in patients with functional bowel disorders. Bifidobacterium infantis 35624 has demonstrated improvement in abdominal pain/discomfort and bloating in IBS patients, along with modulation of the IL-10/IL-12 ratio. VSL#3, a multi-strain probiotic formulation, has shown efficacy in reducing bloating in both children and adults with IBS in several placebo-controlled trials. Probiotic efficacy appears to be strain-specific, and further research is needed to define optimal strains and dosages for bloating.
E. Prescription Medications
1. Antibiotics: Rifaximin, a poorly absorbed antibiotic, is among the best-studied medications for bloating. Multiple randomized, placebo-controlled trials have demonstrated rifaximin’s efficacy in improving global IBS symptoms, including bloating, compared to placebo. Rifaximin has shown sustained symptom improvement in a subset of patients even after treatment cessation. Pooled analyses of large IBS trials have confirmed rifaximin’s superior efficacy over placebo in providing adequate bloating relief.
2. Tricyclic Antidepressants (TCAs): TCAs are frequently used for functional abdominal pain and have also shown benefit for bloating. Studies comparing desipramine to cognitive behavioral therapy have demonstrated bloating improvement alongside pain reduction in functional abdominal pain patients. Ongoing research may further clarify the role of TCAs in bloating associated with functional dyspepsia.
3. Smooth Muscle Antispasmodics: While commonly used in Europe for IBS-related abdominal pain, smooth muscle antispasmodics are not widely available in the US and lack robust clinical trial data in this population. Theoretically, these agents could worsen bloating by promoting gas accumulation and delaying transit. Therefore, routine use for bloating is not generally recommended.
4. Osmotic Laxatives: Osmotic laxatives like polyethylene glycol (PEG) are effective for constipation and have been shown to improve bloating in patients with chronic constipation. However, their efficacy for bloating as a primary complaint is not well-established.
5. Prokinetic Agents:
Neostigmine: Intravenous neostigmine has shown promise in inducing rapid gas clearance in hospitalized patients with acute colonic pseudo-obstruction and bloating. However, limited studies and the need for supervised administration restrict its routine use for chronic bloating. Oral pyridostigmine showed only marginal bloating improvement in one small IBS study.
Cisapride: Cisapride, a mixed 5-HT3/5-HT2 antagonist and 5-HT4 agonist, was previously used for reflux, dyspepsia, gastroparesis, constipation, and IBS, but was withdrawn from the US market. It showed some bloating improvement in functional dyspepsia patients, but less benefit in IBS with constipation.
Domperidone & Metoclopramide: Domperidone and metoclopramide, dopamine antagonists used for dyspepsia and gastroparesis, may improve upper abdominal bloating associated with these conditions. However, robust evidence from randomized controlled trials for functional bloating is lacking. One study found metoclopramide ineffective for abdominal distention in dyspepsia.
Tegaserod: Tegaserod, a 5-HT4 agonist, was approved for IBS with constipation in women and demonstrated bloating improvement in studies. However, it was withdrawn from the US market but remains available for emergency use. Other 5-HT4 agonists like prucalopride may become available in the future.
6. Chloride Channel Activators:
Lubiprostone: Lubiprostone, a chloride channel activator, has demonstrated efficacy in improving overall IBS symptoms, including bloating, in women with constipation-predominant IBS in phase III trials.
Linaclotide: Linaclotide, a guanylate cyclase receptor agonist, has shown significant improvement in bloating, stool frequency, and abdominal pain in patients with chronic constipation and constipation-predominant IBS in multiple placebo-controlled studies.
VIII. Summary: Navigating the Complexities of Abdominal Bloating
Abdominal bloating and distention are highly prevalent and distressing symptoms. While often used interchangeably, they likely represent distinct entities with different underlying mechanisms. A thorough history, physical examination, and selective investigations can help differentiate bloating from distention and identify potential organic causes versus functional disorders. Reassurance, patient education, and a stepwise therapeutic approach incorporating dietary modifications, probiotics, and medications are crucial for managing these chronic conditions and improving patient outcomes. A focused approach on abdominal bloating differential diagnosis and tailored management strategies can significantly improve the quality of life for individuals suffering from this common and often debilitating symptom.