Recent epidemiological studies highlight a concerning rise in the prevalence of gastroesophageal reflux disease (GERD) across the globe, including the United States. A significant complication of GERD is Barrett’s esophagus (BE), occurring in 10–15% of GERD patients. BE is characterized by the transformation of the normal squamous epithelium of the distal esophagus into columnar-lined intestinal metaplasia (IM). Several factors increase the risk of developing BE, including long-term GERD, male sex, central obesity, and being over 50 years of age. The primary concern with BE is its potential to progress to esophageal adenocarcinoma (EAC), a cancer with increasing incidence since the 1970s. Therefore, screening and surveillance programs for BE are crucial for identifying individuals at risk of EAC progression.
This guideline aims to provide a comprehensive review of BE, covering its definition, epidemiology, screening methods, surveillance strategies, and current treatment options. These options include medical, endoscopic, and surgical approaches. To ensure the rigor of our recommendations, we have employed the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system. This system classifies the level of evidence from “high” (high confidence in effect estimate) to “very low” (very uncertain effect estimate). Recommendation strength is categorized as “strong” (desirable effects clearly outweigh undesirable effects) or “conditional” (uncertainty about tradeoffs). Our evidence review prioritized meta-analyses and systematic reviews, followed by clinical trials and observational studies. Data from high-evidence papers were inputted into the GRADE program (www.gradepro.org) to construct GRADE tables and rate evidence for each recommendation. Recommendations are structured using the PICO (patient, intervention, comparison, outcome) format where feasible. A summary of aggregate recommendation statements is provided in Table 1.
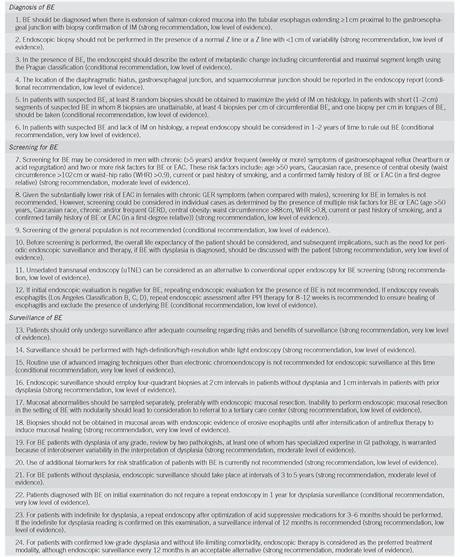
Table 1: ACG guideline recommendation statements on Barrett’s Esophagus diagnosis and management.
Table 1: Continued ACG guideline recommendations for clinical practice in Barrett’s Esophagus.
The development of this guideline involved a comprehensive literature search using Ovid MEDLINE (1946–present), EMBASE (1988–present), and SCOPUS (1980–present). Key search terms included “Barrett esophagus,” “Barrett oesophagus,” “epithelium,” “goblet cells,” “metaplasia,” “dysplasia,” “precancerous conditions,” “adenocarcinoma,” “radiofrequency,” “catheter ablation,” “early detection of cancer,” “mass screening,” and “esophagoscopy.” The detailed literature search strategy is available in Supplementary Appendix 1 online.
DIAGNOSIS OF BE
Recommendations
-
- Diagnosis of Barrett’s Esophagus: BE should be diagnosed when salmon-colored mucosa extends ≥1 cm into the tubular esophagus, proximal to the gastroesophageal junction (GEJ), and is confirmed by biopsy showing intestinal metaplasia (IM) (strong recommendation, low level of evidence). This is a critical step in the clinical guideline diagnosis of Barrett’s esophagus.
-
- Biopsy in Normal Z-line: Endoscopic biopsy should not be performed if the Z-line is normal or shows only irregularity, as per ACG clinical guidelines for Barrett’s esophagus diagnosis.
-
- Prague Classification: In cases of BE diagnosis, endoscopists should use the Prague classification to describe the extent of metaplastic change, including circumferential and maximal segment length (conditional recommendation, low level of evidence). Accurate Prague classification is essential for diagnosis and management of Barrett’s esophagus according to clinical guidelines.
-
- Reporting Endoscopic Landmarks: Endoscopy reports should include the location of the diaphragmatic hiatus, GEJ, and squamocolumnar junction (conditional recommendation, low level of evidence). Precise reporting of these landmarks is vital for consistent Barrett’s esophagus diagnosis and management.
-
- Biopsy Protocol for Suspected BE: For suspected BE, at least 8 random biopsies should be taken to maximize IM detection. For short BE segments (1–2 cm) where 8 biopsies are not feasible, obtain at least 4 biopsies per cm of circumferential BE and one biopsy per cm in BE tongues (conditional recommendation, low level of evidence). This biopsy protocol is recommended by ACG clinical guidelines to improve diagnostic yield in Barrett’s esophagus.
-
- Repeat Endoscopy for Suspected BE without IM: If suspected BE lacks IM on initial histology, consider repeat endoscopy in 1–2 years to rule out BE (conditional recommendation, very low level of evidence). Repeat endoscopy is a diagnostic strategy in the management of Barrett’s esophagus when initial biopsies are negative for IM.
Summary of Evidence
Establishing a Diagnosis of BE
Barrett’s esophagus is traditionally defined by the presence of at least 1 cm of metaplastic columnar epithelium replacing the normal stratified squamous epithelium in the distal esophagus. This 1 cm threshold is significant because segments of this length or greater are associated with an increased risk of esophageal adenocarcinoma.
The definition of BE has varied, particularly regarding the requirement for intestinal metaplasia (IM) on biopsy. In the United States, IM has been a standard diagnostic criterion for BE. Conversely, guidelines from the United Kingdom have considered visual evidence of columnar-lined epithelium (CLE) on endoscopy, with biopsy confirmation of columnar metaplasia (regardless of IM presence), sufficient for BE diagnosis. This divergence stems from differing views on the EAC risk associated with CLE with and without IM. Population-based studies suggest a considerably lower EAC risk in columnar metaplasia without IM compared to that with IM. However, not all studies concur. While DNA abnormalities may be similar in both types of metaplastic epithelium, some research indicates cancer is more frequent in columnar metaplasia with goblet cells (IM) than without.
Despite the debated EAC risk in non-IM CLE and the challenge of sampling error leading to IM misclassification, these ACG clinical guidelines continue to recommend that BE diagnosis requires CLE containing IM. This is based on the apparent difference in cancer risk between CLE with and without IM. Until more evidence indicates a significantly elevated EAC risk in non-IM CLE patients, diagnosing these patients with BE is not advisable due to potential negative impacts on insurance and quality of life.
Cardiac intestinal metaplasia is a common finding, present in up to 20% of asymptomatic individuals undergoing routine endoscopy. Studies suggest that cardiac IM is not more prevalent in BE patients than in controls and is linked to Helicobacter pylori infection, not EAC. Therefore, biopsies of a normal or slightly irregular esophagogastric junction (EGJ) are not routinely recommended in the diagnosis and management of Barrett’s esophagus, according to these guidelines.
The EGJ location is defined anatomically as where the distal tubular esophagus meets the proximal gastric folds. This location can vary with respiration, air insufflation, and esophageal motility. Some Japanese endoscopists use the distal limit of lower esophageal palisade vessels to define the EGJ. However, this method often places the palisade vessel lower than the EGJ, resulting in short CLE segments without IM. Comparative studies indicate that the proximal extent of gastric folds is a more accurate EGJ marker than palisade vessels. The diaphragmatic hiatus is identified endoscopically as an indentation of gastric folds during inspiration.
Segments of BE longer than 3 cm are classified as long-segment BE, while shorter segments are short-segment BE. Uniform classification is recommended, though its impact on patient management remains unproven. The Prague classification, introduced in 2006, assesses the circumferential (C) and maximum (M) extent of endoscopically visualized BE, using endoscopic landmarks (Figure 1). Prospective application shows high reliability for BE segments >1 cm, EGJ location, and diaphragmatic hiatus, but less so for segments <1 cm. For suspected BE, guidelines recommend 4 biopsies every 2 cm of segment length, or at least 8 biopsies if the segment is <2 cm to increase diagnostic accuracy.
Figure 1: Prague Classification for Barrett’s esophagus (BE). C indicates circumferential extent, M indicates maximal extent of metaplasia. Schema shows a C2M5 segment with GEJ below the squamocolumnar junction. Reprinted with permission (24).
In suspected BE cases without IM confirmation despite adequate biopsies, repeat endoscopy in 1–2 years can be considered. Longitudinal studies show that approximately 30% of these patients may demonstrate IM on repeat examination, supporting the diagnostic recommendation in these clinical guidelines for Barrett’s esophagus.
EPIDEMIOLOGY AND NATURAL HISTORY OF BE
Summary Statements
What are the risk factors for BE according to ACG clinical guidelines?
-
Established risk factors for Barrett’s Esophagus include:
- Chronic (>5 years) GERD symptoms
- Older age (>50 years)
- Male gender
- Tobacco use
- Central obesity
- Caucasian race
-
Alcohol consumption is not a risk factor for BE. Wine consumption may be protective.
-
BE is more prevalent in first-degree relatives of individuals with known BE, highlighting familial risk factors in Barrett’s esophagus.
What are the risk factors for dysplasia and EAC development in BE patients?
- Known risk factors for neoplasia development in BE include:
- Older age
- Increased BE length
- Central obesity
- Tobacco use
- Lack of nonsteroidal anti-inflammatory drug (NSAID) use
- Lack of proton pump inhibitor (PPI) use
- Lack of statin use.
What is the cancer risk in BE based on dysplasia grade?
- Annual cancer progression risk in nondysplastic BE is ∼0.2–0.5%.
- Annual cancer progression risk in low-grade dysplasia (LGD) is ∼0.7%.
- Annual neoplastic progression risk in high-grade dysplasia (HGD) is ∼7%.
- Most (>90%) BE patients die from causes other than EAC, emphasizing the overall context of Barrett’s esophagus and mortality.
Summary of Evidence
Risk Factors for BE
Barrett’s esophagus is detected in about 15% of patients with chronic GERD and in approximately 1–2% of the general population. A Swedish population-based study found severe and chronic GERD as EAC risk factors; however, 40% of esophageal cancer patients reported no prior GERD symptoms. GERD symptom duration is a BE risk factor. A cohort study showed that 11% of GERD patients had BE on endoscopy, with longer GERD duration correlating with higher BE prevalence. Meta-analysis confirmed a significant association between GERD symptoms and BE, particularly long-segment BE.
Table 2: Risk factors for Barrett’s Esophagus (BE) as estimated from available meta-analyses, guiding clinical guideline risk assessment.
Increasing age is a BE risk factor. A database study showed BE yield in white men with GERD increasing from 2% in the third decade to 9% in the sixth. Early GERD onset is also associated with BE. A VA study found the highest BE risk in patients with weekly GERD symptoms starting before age 30, with risk increasing linearly with earlier symptom onset and cumulative GERD duration.
Male gender is consistently identified as a BE and EAC risk factor. Meta-analysis showed a 2:1 male/female ratio in BE prevalence. EAC risk is also significantly higher in men. A SEER database study reported women comprising only 12% of EAC cases, with EAC risk in women with GERD symptoms being similar to breast cancer risk in men.
Tobacco use is a BE risk factor, as shown in a meta-analysis of 39 studies. Any history of smoking was associated with increased BE risk compared to non-GERD controls, but not significantly compared to chronic GERD patients, suggesting tobacco’s BE risk may be mediated through increased GERD.
In contrast to tobacco, alcohol consumption is not significantly linked to BE risk. Some data suggest wine consumption may be protective, with odds ratios indicating reduced BE risk among wine drinkers.
Obesity is an independent risk factor for BE and EAC. Central obesity, rather than overall BMI, is the primary risk factor. Meta-analysis showed centrally obese patients having twice the BE risk compared to those with normal body habitus, even after adjusting for BMI and GERD, indicating a reflux-independent role for central obesity in BE pathogenesis. Overall body fat content is not associated with BE risk. Central obesity is a BE risk factor in both men and women.
Family history of BE is a potential risk factor. A cohort study showed BE significantly more common in first- or second-degree relatives of BE patients compared to controls. Screening first-degree relatives of BE patients yielded a 20% BE diagnosis rate. Single-nucleotide polymorphisms on gene loci may increase BE susceptibility.
Caucasian race is a strong BE risk factor. Lower BE prevalence in African Americans compared to Caucasians is consistent. However, studies comparing BE incidence in Hispanics and non-Hispanic whites are inconsistent, likely due to Hispanic population heterogeneity.
Other reported BE risk factors include metabolic syndrome, type 2 diabetes, and sleep apnea. H. pylori infection, particularly Cag A+ strains, is associated with decreased BE risk in some studies.
Risk Factors Associated with Dysplasia and EAC in BE Patients
Older age and longer BE segment length are known risk factors for dysplasia in BE patients. A multicenter study of BE patients found age and BE segment length over 3 cm as risk factors for prevalent dysplasia, emphasizing the importance of BE segment length in risk stratification.
In BE patients, certain medications are associated with reduced dysplasia and/or EAC risk, including PPIs, aspirin, NSAIDs, and statins. Meta-analysis showed a 71% reduced risk of HGD and/or EAC in PPI users. H2RA use showed no significant effect. Another meta-analysis found cyclooxygenase inhibitors, including aspirin and nonaspirin NSAIDs, associated with reduced HGD and EAC risk, independent of therapy duration. Statins, with their antiproliferative, proapoptotic, antiangiogenic, and immunomodulatory effects, may prevent cancer development. Meta-analysis showed statin use associated with a 41% EAC risk reduction, highlighting potential chemopreventive strategies in the management of Barrett’s esophagus.
Cancer Risk in BE Based on Dysplasia Grade
A 2012 meta-analysis reported lower nondysplastic BE progression risk than previously estimated. The pooled annual EAC incidence was 0.33%. In short-segment BE patients, annual cancer risk was 0.19%.
Table 3: Cancer risk based on degree of dysplasia in Barrett’s Esophagus, according to clinical guideline data.
For LGD patients, meta-analysis showed pooled annual incidence rates of 0.5% for EAC alone and 1.7% for HGD/EAC combined. However, heterogeneity existed, and when stratified by LGD/BE ratio (as a pathology quality surrogate), EAC incidence was 0.76% per year for a ratio of 0.15, suggesting lower progression risk when LGD diagnosis is more liberally made.
HGD patients’ EAC risk was examined in a meta-analysis showing a weighted annual incidence rate of 7%. However, the AIM-Dysplasia trial reported a much higher 19% yearly progression rate in the HGD surveillance arm, similar to another randomized trial requiring expert pathologist confirmation of HGD. These findings suggest that the rigor of histologic validation significantly impacts subsequent EAC risk assessment in Barrett’s esophagus clinical guidelines.
Common Causes of Death in BE Subjects
Most BE patients die from causes other than EAC. Meta-analysis of mortality rates in BE patients showed a pooled fatal EAC incidence rate of 3 per 1,000 person-years. Cause-specific mortality data showed 7% of deaths due to EAC and 93% from other causes. The most common causes were cardiac disease (35%), pulmonary disease (20%), and other malignancies (16%). This emphasizes the importance of considering overall health and comorbidities in the management of Barrett’s esophagus.
SCREENING FOR BE
Recommendations
-
- Screening for BE in High-Risk Men: BE screening may be considered for men with chronic (>5 years) and/or frequent (weekly or more) GERD symptoms (heartburn or acid regurgitation) and two or more risk factors for BE or EAC. Risk factors include: age >50 years, Caucasian race, central obesity (waist circumference >102 cm or waist–hip ratio >0.9), current or past smoking history, and confirmed family history of BE or EAC in a first-degree relative (strong recommendation, moderate level of evidence). These criteria help define targeted screening in ACG clinical guidelines for Barrett’s esophagus.
-
- Screening Considerations for Women: Given the lower EAC risk in women with chronic GERD symptoms, routine BE screening is not recommended for women. However, screening may be considered in individual cases with multiple BE/EAC risk factors: age >50 years, Caucasian race, chronic/frequent GERD, central obesity (waist circumference >88 cm, waist–hip ratio >0.8), current/past smoking history, and confirmed family history of BE or EAC in a first-degree relative (strong recommendation, low level of evidence). This recommendation acknowledges gender-specific risk in Barrett’s esophagus screening guidelines.
-
- General Population Screening Not Recommended: Screening the general population for BE is not recommended (conditional recommendation, low level of evidence). Population-wide screening is not supported by current evidence in ACG clinical guidelines for Barrett’s esophagus.
-
- Consider Life Expectancy and Implications: Before screening, consider patient life expectancy and implications of BE diagnosis, such as periodic surveillance and therapy if dysplasia is found. Discuss these with the patient (strong recommendation, very low level of evidence). Informed consent and consideration of patient-specific factors are crucial in Barrett’s esophagus screening decisions.
-
- Unsedated Transnasal Endoscopy (uTNE) as Alternative: uTNE can be considered as an alternative to conventional upper endoscopy for BE screening (strong recommendation, low level of evidence). uTNE offers a less invasive screening option in ACG clinical guidelines for Barrett’s esophagus.
-
- Limited Repeat Endoscopy After Negative Initial Evaluation: If initial endoscopy is negative for BE, repeat endoscopy for BE screening is not generally recommended. If endoscopy reveals esophagitis (Los Angeles Classification B, C, D), repeat endoscopy after 8–12 weeks of PPI therapy is recommended to ensure esophagitis healing and exclude underlying BE (conditional recommendation, low level of evidence). This recommendation addresses appropriate follow-up after initial negative endoscopy or esophagitis diagnosis in Barrett’s esophagus management.
Summary of Evidence
Survival rates for EAC with regional or distant spread remain poor. The metaplasia-dysplasia-carcinoma sequence in BE suggests that BE screening, dysplasia surveillance, and endoscopic intervention can reduce EAC incidence. Screening can detect both BE and prevalent dysplasia or carcinoma treatable with endoscopic therapy. However, evidence supporting this hypothesis primarily comes from retrospective studies potentially subject to biases. Over 90% of EAC cases are diagnosed in patients without prior BE diagnosis, despite increasing endoscopy use.
Widespread population screening could incur substantial economic costs from diagnostic tests and subsequent surveillance. Economic modeling studies suggest BE screening (by endoscopy) followed by surveillance in high-risk groups (e.g., 50-year-old men with GERD symptoms) can be cost-effective, with acceptable cost-effectiveness ratios. Estimates vary due to differing assumptions. Some studies suggest video capsule endoscopy or uTNE screening is cost-effective compared to no screening, but standard endoscopy is preferred over capsule endoscopy. These models often assume near-100% participation and accuracy rates, likely overestimates given reported lower participation (18–49%) and endoscopy accuracy rates (80%). A significant proportion of community BE diagnoses are reversed, likely due to incorrect landmark identification and biopsy targeting. Repeat endoscopy after an initial negative BE endoscopy has low yield (2.3%), with esophagitis and male gender predicting BE diagnosis at subsequent endoscopy. However, studies report 9–12% BE prevalence on repeat endoscopy after PPI treatment for esophagitis, making repeat endoscopy advisable after healing more severe erosive esophagitis.
BE screening faces challenges. Symptomatic GERD, while a BE/EAC risk factor, is neither sensitive nor specific. Only 5–15% of patients with chronic and frequent reflux have BE, and up to 50% of BE/EAC patients do not report chronic reflux symptoms. Studies report substantial BE prevalence in asymptomatic individuals. Reflux symptoms are associated with long-segment BE but less consistently with short-segment BE. Thus, GERD symptom-based BE screening is likely inadequate. Women, even with daily reflux symptoms, have low EAC incidence, comparable to men without reflux symptoms. This may relate to lower EAC progression risk in women with BE and should influence BE screening thresholds in women, as reflected in these ACG clinical guidelines for Barrett’s esophagus.
Recent reports describe BE prediction/risk scores using combined risk factors, potentially improving screening efficiency by targeting high-risk populations. Accuracy for BE prediction, while improved from GERD-only models, remains modest (AUC 0.73–81), but may improve with additional variables like circulating cytokine levels. Validation in larger, unselected populations is crucial before widespread use.
Several techniques are available for BE screening. Conventional endoscopy is the gold standard, despite accuracy limitations. uTNE shows comparable performance to endoscopy for BE diagnosis (sensitivity 98%, specificity 100%). Feasibility and safety of community uTNE screening are demonstrated. Esophagoscopes with disposable sheaths may be a viable alternative. uTNE limitations include nasopharyngeal intubation difficulty and discomfort, but these are infrequent, and most patients are willing to repeat the procedure. Nonphysician providers can be trained to perform uTNE, further reducing costs. Esophageal video capsule endoscopy is well-tolerated and noninvasive, but inadequate accuracy (pooled sensitivity 78%, specificity 73%) currently precludes its recommendation for BE screening. The Cytosponge, a novel gelatin-coated sponge for esophageal cytology, combined with trefoil factor 3 marker, shows promising sensitivity (73%) and specificity (94%) for BE diagnosis. Despite low participation rates, it is safe and well-tolerated. Its nonendoscopic nature may allow cheaper, office-based BE screening if validated further and is considered in emerging Barrett’s esophagus screening technologies. Modeling studies suggest Cytosponge is cost-effective compared to no screening or sedated endoscopy.
SURVEILLANCE OF BE
Recommendations
-
- Counseling on Surveillance Risks and Benefits: Patients should undergo surveillance only after adequate counseling on risks and benefits (strong recommendation, very low level of evidence). Informed consent is crucial in Barrett’s esophagus surveillance, as emphasized in clinical guidelines.
-
- High-Definition White Light Endoscopy: Surveillance should use high-definition/high-resolution white light endoscopy (strong recommendation, low level of evidence). High-definition endoscopy is the recommended standard for Barrett’s esophagus surveillance to optimize dysplasia detection.
-
- Limited Routine Use of Advanced Imaging: Routine use of advanced imaging techniques other than electronic chromoendoscopy is not recommended for surveillance (conditional recommendation, very low level of evidence). While promising, advanced imaging beyond electronic chromoendoscopy requires further validation for routine surveillance in Barrett’s esophagus.
-
- Biopsy Protocol for Surveillance: Endoscopic surveillance should employ four-quadrant biopsies at 2 cm intervals in patients without dysplasia and 1 cm intervals in patients with prior dysplasia (strong recommendation, low level of evidence). Systematic biopsy protocols are crucial for effective dysplasia detection during Barrett’s esophagus surveillance.
-
- Sampling Mucosal Abnormalities: Mucosal abnormalities should be sampled separately, preferably with endoscopic mucosal resection (EMR). Referral to a tertiary center is recommended if EMR is not feasible for nodular BE (strong recommendation, low level of evidence). Targeted EMR of mucosal abnormalities is essential for accurate staging and management of Barrett’s esophagus.
-
- Avoid Biopsies in Active Esophagitis: Biopsies should not be taken from mucosal areas with endoscopic evidence of erosive esophagitis until antireflux therapy induces mucosal healing (strong recommendation, very low level of evidence). Inflammation can confound dysplasia assessment, so healing esophagitis is a prerequisite for accurate Barrett’s esophagus surveillance.
-
- Pathology Review for Dysplasia: For BE patients with any grade of dysplasia, review by two pathologists, with GI pathology expertise, is warranted due to interobserver variability in dysplasia interpretation (strong recommendation, moderate level of evidence). Second-opinion pathology review is critical for dysplasia grading accuracy in Barrett’s esophagus management.
-
- Biomarkers Not Routinely Recommended: Routine use of additional biomarkers for risk stratification in BE patients is currently not recommended (strong recommendation, low level of evidence). Biomarkers are not yet validated for routine clinical use in Barrett’s esophagus risk stratification according to clinical guidelines.
-
- Surveillance Intervals for Nondysplastic BE: For nondysplastic BE patients, endoscopic surveillance should occur at 3 to 5-year intervals (strong recommendation, moderate level of evidence). Extended surveillance intervals are appropriate for nondysplastic Barrett’s esophagus due to its low progression risk.
-
- No Routine 1-Year Repeat Endoscopy After Initial BE Diagnosis: Patients diagnosed with BE on initial examination with adequate surveillance biopsies do not require a repeat endoscopy in 1 year for dysplasia surveillance (conditional recommendation, very low level of evidence). Routine 1-year repeat endoscopy after initial BE diagnosis is not supported by evidence in clinical guidelines for Barrett’s esophagus.
-
- Management of Indefinite for Dysplasia: For indefinite for dysplasia findings, repeat endoscopy after 3–6 months of optimized acid suppression is recommended. If indefinite for dysplasia persists, a 12-month surveillance interval is recommended (strong recommendation, low level of evidence). Specific management strategies are advised for indefinite for dysplasia findings in Barrett’s esophagus surveillance.
-
- Endoscopic Therapy Preferred for Confirmed LGD: For patients with confirmed LGD without life-limiting comorbidity, endoscopic therapy is preferred, though annual surveillance is an acceptable alternative (strong recommendation, moderate level of evidence). Endoscopic therapy is increasingly favored over surveillance for confirmed LGD in Barrett’s esophagus management guidelines.
-
- Endoscopic Therapy for Confirmed HGD: Patients with BE and confirmed HGD should be managed with endoscopic therapy unless they have life-limiting comorbidity (strong recommendation, high level of evidence). Endoscopic therapy is the standard of care for confirmed HGD in Barrett’s esophagus to prevent progression to EAC.
Summary of the Evidence
Rationale for Surveillance
EAC survival is stage-dependent, with early spread before symptom onset being characteristic. Lymph node metastases are a key factor in decreased survival. Early cancer detection at a curable stage is crucial for improved EAC survival.
Observational studies suggest that EAC detected during BE surveillance programs is diagnosed at an earlier stage with improved survival compared to non-surveilled patients. Nodal involvement is less likely in surveilled patients. As esophageal cancer survival is stage-dependent, these studies suggest surveillance may enhance survival. Recent population-based studies confirm a survival advantage for EAC patients receiving adequate endoscopic surveillance compared to those not surveilled. Similarly, studies show enhanced survival, lower tumor stage, and lower tumor grade in EAC patients with prior BE diagnosis compared to those without. These findings persist, though attenuated, even after correcting for lead time and length time bias. However, a case-control study found no evidence that endoscopic surveillance improved EAC survival. While prospective clinical trial data demonstrating surveillance benefit are lacking, the heterogeneous evidence base supports continued endoscopic surveillance for BE patients, as per ACG clinical guidelines for Barrett’s esophagus.
However, current endoscopic surveillance has shortcomings. Dysplasia may be endoscopically invisible, and dysplasia/cancer distribution is variable. Even thorough biopsy protocols can have sampling errors. Surveillance programs are costly and time-consuming. Adherence to guidelines is problematic and worsens with longer segment lengths. These shortcomings likely diminish surveillance benefits, emphasizing the need to adhere to published standards for surveillance performance.
Counseling for Surveillance
Before surveillance, patients should be counseled on risks and benefits, including surveillance endoscopy limitations and the importance of adhering to surveillance intervals. Other considerations include age, 5-year survival likelihood, and tolerance for interventions like endoscopic therapy, surgery, and cancer treatments.
Early outpatient consultation to review BE significance is increasingly important. Internet access allows patients unfiltered BE/EAC information. Studies show patients both over- and under-estimate their cancer risk. Given the low progression risk for most BE patients and that most die from other causes, counseling should be part of ongoing care to inform therapeutic decisions, aligning with patient-centered approaches in Barrett’s esophagus management.
Surveillance Technique
Endoscopic surveillance should use high-resolution/high-definition white light endoscopy to optimize mucosal detail visualization. Recent data suggest superiority over standard-definition endoscopy for dysplasia detection. This should be combined with mucosal debris removal and careful lumen insufflation/desufflation. Retroflexed GEJ view should be included. Data show a direct correlation between Barrett’s segment inspection time and HGD/EAC detection. Barrett’s segment inspection should focus on the right hemisphere (12 to 6 o’clock position), where early cancer appears to preferentially develop.
Surveillance aims to detect dysplasia, classified using a five-tier system: (i) negative for dysplasia, (ii) indefinite for dysplasia, (iii) LGD, (iv) HGD, and (v) carcinoma. Active inflammation makes dysplasia differentiation from reparative changes difficult. Surveillance biopsies should be performed after GERD-related inflammation is controlled with antisecretory therapy. Ongoing erosive esophagitis is a relative contraindication for surveillance biopsies. Once inflammation is controlled, systematic four-quadrant biopsies at 2 cm intervals along the entire Barrett’s segment remain standard for nondysplastic BE surveillance, as recommended by ACG clinical guidelines for Barrett’s esophagus.
Systematic biopsy protocols detect more dysplasia and early cancer than ad hoc random biopsies. Subtle mucosal abnormalities (ulceration, erosion, plaque, nodule, stricture, or luminal irregularity) should also be sampled, as they are associated with underlying cancer. Mucosal abnormalities in patients with known dysplasia should undergo EMR. EMR changes diagnosis in ∼50% of cases compared to biopsies due to larger tissue samples, improving pathologist agreement. Systematic biopsy protocols are safe. Routine cytologic sampling adds little to surveillance biopsies. Computer-assisted or wide-field brush biopsy for increasing dysplasia yield is under investigation. Subsquamous BE finding on surveillance biopsies does not currently change patient management, based on the most advanced histology from targeted and random biopsies.
Advanced Endoscopic Imaging Techniques
Various enhancements to white light endoscopy have been studied for detailed Barrett’s segment inspection. Electronic chromoendoscopy allows detailed mucosal and vascular pattern imaging without dye sprays, using narrow band imaging (NBI) or postprocessing software. Most literature examines NBI with magnification endoscopy. Randomized trials comparing NBI to high-definition white light endoscopy show no difference in dysplasia/neoplasia detection, but NBI requires fewer biopsies. Meta-analysis suggests electronic chromoendoscopy may increase dysplasia detection. Other image enhancement techniques (methylene blue, acetic acid, indigo carmine staining, autofluorescence endoscopy, confocal laser endomicroscopy, volumetric laser endomicroscopy, spectroscopy, and molecular imaging) are not yet ready for widespread clinical use in routine Barrett’s esophagus surveillance.
Importance of Dysplasia Confirmation
Dysplasia remains the best clinical marker of cancer risk in BE patients. However, interobserver variability exists in dysplasia interpretation, both in community and academic settings. Interobserver agreement is reasonable for IM without dysplasia and HGD/EAC. Interpretation of indefinite for dysplasia and LGD is more challenging. LGD diagnosis confirmation is crucial. Studies show that expert GI pathologist review downgrades a significant proportion of community LGD diagnoses to no dysplasia or indefinite for dysplasia. Other studies suggest community pathologists have difficulties interpreting both nondysplastic BE and dysplasia. Current evidence supports confirming all dysplasia readings by a second pathologist with extensive experience in Barrett’s associated neoplasia, as emphasized in ACG clinical guidelines for Barrett’s esophagus.
Surveillance Intervals
Surveillance intervals are based on dysplasia presence and grade, guided by expert opinion. Given the low BE progression risk to EAC, 3- to 5-year intervals are reasonable for nondysplastic BE patients.
Data guiding management of indefinite for dysplasia BE patients are limited. Double-dose PPI therapy to reduce inflammation is reasonable. Retrospective studies suggest indefinite for dysplasia has a similar cancer progression risk to LGD, or a higher risk in the first year after diagnosis but similar to nondysplastic BE thereafter. Multifocal indefinite for dysplasia may have higher progression risk than focal. Surveillance for these patients should follow LGD recommendations.
If LGD is found, diagnosis confirmation by a second expert pathologist is essential. Aggressive PPI therapy for reflux is recommended to minimize inflammation/regeneration changes. Repeat endoscopy after acid suppression optimization may downgrade LGD reading. If LGD is confirmed and endoscopic therapy is not performed, annual surveillance is recommended until two consecutive examinations are dysplasia-negative, then surveillance intervals for nondysplastic BE can be followed. Four-quadrant biopsies at 1 cm intervals are advisable, given dysplasia’s mosaic pattern and small surface area involvement. EMR should be performed for any mucosal abnormality.
If HGD is found, diagnosis confirmation by a second expert GI pathologist is crucial. EMR is warranted for any mucosal abnormality to maximize staging accuracy. If HGD is confirmed, endoscopic intervention is indicated, as per ACG clinical guidelines for Barrett’s esophagus. Figure 2 summarizes recommended actions for nonnodular BE surveillance.
Figure 2: Management algorithm for nonnodular Barrett’s esophagus (BE) surveillance according to ACG clinical guidelines. Endoscopic eradication therapy is preferred for dysplasia, but 1-year surveillance endoscopy is an alternative for LGD. Algorithm assumes T1a EAC has favorable characteristics for endoscopic therapy. EGD, esophagogastroduodenoscopy; HGD, high-grade dysplasia; LGD, low-grade dysplasia; PPI, proton pump inhibitor.
Biomarkers of Increased Risk
Given endoscopic surveillance and histologic dysplasia limitations as risk stratification tools, molecular markers for identifying high-risk patients are studied. DNA content abnormalities, chromosomal abnormalities, gene mutations, methylation changes, and clonal diversity measurements define patients at increased progression risk. These genetic abnormalities appear early in disease development.
Promising research suggests aberrant p53 expression (absent or increased by immunohistochemistry) is associated with increased neoplastic progression risk. However, no single biomarker is adequate for risk stratification. A panel of biomarkers may be required due to the complexity and diversity of alterations in the progression sequence. Currently, no biomarkers or panels are ready for clinical practice in Barrett’s esophagus management guidelines. Biomarker validation requires large prospective cohorts, challenging given the low overall BE progression to HGD/EAC rate.
THERAPY
Recommendations
Chemoprevention
-
- PPI Therapy for BE Patients: Patients with BE should receive once-daily PPI therapy. Routine twice-daily dosing is not recommended unless needed for reflux symptom or esophagitis control (strong recommendation, moderate level of evidence). PPI therapy is recommended for all BE patients in ACG clinical guidelines, primarily at once-daily dosing.
-
- No Routine Aspirin/NSAIDs for Chemoprevention: Aspirin or NSAIDs should not be routinely prescribed to BE patients for antineoplastic strategy. Other putative chemopreventive agents also lack sufficient evidence for routine administration (conditional recommendation, high level of evidence). Routine chemoprevention with aspirin/NSAIDs or other agents is not recommended in Barrett’s esophagus management guidelines.
Endoscopic Therapy
-
- EMR for Nodular Lesions: Patients with nodularity in the BE segment should undergo EMR of nodular lesions as the initial diagnostic and therapeutic step. Histologic assessment of the EMR specimen should guide further therapy. For EMR specimens showing HGD or intramucosal carcinoma, ablative therapy of remaining BE should be performed (strong recommendation, high level of evidence). EMR is critical for nodular lesions in BE, guiding subsequent therapy based on histologic findings.
-
- Management of Deep Margin Neoplasia: In patients with EMR specimens showing neoplasia at a deep margin, residual neoplasia should be assumed, and surgical, systemic, or additional endoscopic therapies should be considered (strong recommendation, low level of evidence). Deep margin involvement in EMR specimens necessitates consideration of further aggressive therapy in Barrett’s esophagus management.
-
- Ablative Therapy Not for Nondysplastic BE: Endoscopic ablative therapies should not be routinely applied to nondysplastic BE patients due to low EAC progression risk (strong recommendation, very low level of evidence). Endoscopic eradication therapy is the procedure of choice for confirmed LGD and HGD (see points 24 and 25). Ablative therapy is not recommended for nondysplastic BE, but is preferred for dysplasia according to ACG clinical guidelines for Barrett’s esophagus.
-
- Endoscopic Therapy for T1a EAC: In patients with T1a EAC, endoscopic therapy is the preferred approach, being effective and well-tolerated (strong recommendation, moderate level of evidence). Endoscopic therapy is the primary treatment modality for T1a EAC in Barrett’s esophagus.
-
- Multidisciplinary Consultation for T1b EAC: In patients with T1b EAC, multidisciplinary surgical oncology team consultation should occur before endoscopic therapy. Endoscopic therapy may be an alternative to esophagectomy, especially for superficial (sm1) disease with well-differentiated neoplasm lacking lymphovascular invasion, and for poor surgical candidates (strong recommendation, low level of evidence). T1b EAC management requires a multidisciplinary approach, with endoscopic therapy as a potential alternative to surgery in select cases.
-
- EUS Before EMR Not Routinely Beneficial: Routine staging with endoscopic ultrasound (EUS) or other imaging before EMR for nodular BE has no demonstrated benefit. EUS findings should not preclude EMR performance to stage early neoplasia due to potential overstaging and understaging (strong recommendation, moderate level of evidence). Pre-EMR EUS is not routinely indicated for nodular BE according to clinical guidelines for Barrett’s esophagus.
-
- EUS Role in T1b Disease: In patients with known T1b disease, EUS may help assess and sample regional lymph nodes, given increased lymph node involvement prevalence in these patients compared to less advanced disease (strong recommendation, moderate level of evidence). EUS may be useful for staging lymph nodes in T1b EAC in Barrett’s esophagus management.
-
- Radiofrequency Ablation Preferred for Nonnodular Dysplastic BE: In patients with dysplastic BE undergoing ablative therapy for nonnodular disease, radiofrequency ablation (RFA) is currently the preferred endoscopic ablative therapy (strong recommendation, moderate level of evidence). RFA is the preferred ablative modality for nonnodular dysplastic BE in ACG clinical guidelines.
Surgical Therapy
-
- Antireflux Surgery Not for Antineoplastic Measure: Antireflux surgery should not be pursued in BE patients as an antineoplastic measure. However, it should be considered for those with incomplete reflux control on optimized medical therapy (strong recommendation, high level of evidence). Antireflux surgery is not indicated for cancer prevention in BE, but for GERD symptom control unresponsive to medical therapy.
-
- Esophagectomy for Submucosal Invasion (T1b sm2–3) EAC: In EAC cases with submucosal invasion, especially mid or deep submucosa (T1b sm2–3), esophagectomy, with neoadjuvant therapy consideration, is recommended in surgical candidates (strong recommendation, low level of evidence). Esophagectomy is the recommended treatment for T1b sm2–3 EAC in suitable patients according to Barrett’s esophagus management guidelines.
-
- Consider Surgical/Multimodality Therapy for Unfavorable T1a/T1b sm1 EAC: In patients with T1a or T1b sm1 EAC with poor differentiation, lymphovascular invasion, or incomplete EMR, surgical and/or multimodality therapies should be considered (strong recommendation, low level of evidence). Unfavorable features in early EAC may warrant surgical or multimodality approaches in Barrett’s esophagus management.
Summary of Evidence
Therapeutic aspects of BE management have significantly evolved since previous guidelines, particularly in effective endoscopic therapy for neoplastic BE. Chemoprevention, endoscopic intervention, and surgical evaluation are discussed below.
Chemoprevention
Data supporting chemoprevention in BE are limited, partly due to the low neoplasia progression rate in BE, making intervention studies challenging. Also, patients previously considered for chemoprevention, like those with LGD, are now candidates for endoscopic ablative therapy, reducing the patient pool benefiting from chemoprevention.
PPI therapy is common in BE patients, often for symptomatic GERD control. PPI use is supported by symptom control needs, making chemoprevention secondary. However, even in asymptomatic BE patients, PPI use deserves consideration. Cohort studies suggest PPI therapy in BE patients reduces neoplastic BE progression risk compared to no acid suppression or H2RA therapy. PPIs have a favorable risk profile and reduced cost due to generics. These factors, combined with the theoretical role of inflammation in BE pathogenesis and progression, justify PPI use in BE patients, even without GERD symptoms. Randomized PPI trials in BE are unlikely, making decisions reliant on retrospective data and expert opinion, as reflected in ACG clinical guidelines for Barrett’s esophagus.
Indirect evidence supports aspirin (ASA) as a chemopreventive agent in BE. ASA users appear less likely to develop esophageal cancer in epidemiological studies. ASA and NSAIDs may inhibit oncogenesis pathways. However, unlike PPIs, ASA’s side-effect profile is not benign, with potential for serious bleeding. Also, with level 1 evidence showing markedly reduced cancer risk in LGD patients undergoing endoscopic therapy, more LGD patients will likely opt for therapy over surveillance, lessening chemoprevention need. Nondysplastic BE has a very low progression risk, so any chemopreventive agent must be very safe to justify use. While awaiting results from an ASA vs. placebo trial in BE patients, current data do not justify routine ASA or NSAID use for BE chemoprevention. However, BE patients who are also candidates for ASA for cardioprotection may derive additional chemoprotective benefit.
Endoscopic Therapy
Endoscopic therapy advances have broadened the pool of BE patients eligible for intervention and reduced esophagectomy need. Endoscopists should apply evidence-based decision-making in utilizing these technologies.
Endoscopic therapy consideration starts with close BE mucosa inspection. Mucosal irregularities (nodularity, ulceration, flat but irregular contour) are key for detecting high-yield neoplasia areas. Narrow light spectrum imaging (NBI) may aid mucosal irregularity detection. If irregularities are found, EMR or endoscopic submucosal dissection (ESD) is the next step, for both therapy and lesion staging. While ESD may provide better lateral margin assessment, it is technically demanding and should be performed in expert centers. EMR is generally adequate for assessing invasion depth, the most clinically important variable in Barrett’s esophagus management guidelines.
EMR findings determine subsequent management. Nondysplastic BE patients with no dysplasia on EMR can resume surveillance. LGD or HGD patients with complete lesion resection should generally undergo ablative therapy post-EMR to eradicate remaining IM and reduce recurrent dysplasia risk. Figure 3 summarizes nodular BE management.
Figure 3: Management algorithm for nodular Barrett’s esophagus (BE) as per ACG clinical guidelines. Endoscopic submucosal dissection is an alternative to EMR. Favorable histology includes no lymphatic or vascular invasion and moderate- to well-differentiated disease. EAC, esophageal adenocarcinoma.
In nonnodular BE, ablative therapy utility is clearer. For BE with HGD, ablative therapy is preferred over esophagectomy or intensive surveillance due to proven efficacy and better side-effect profile than surgery. Recent data show that in BE with confirmed LGD, ablative therapy significantly reduces progression to HGD/EAC or EAC alone. In contrast, nondysplastic BE has lower progression rates than previously thought. Given low progression risk, low but real complication rate of endoscopic therapy, and associated costs, ablative therapy is not recommended for nondysplastic BE. Whether therapy is warranted in higher lifetime cancer risk groups (familial BE/EAC, young patients with long-segment BE) is unclear.
In EAC, invasion depth determines endoscopic therapy’s curative potential. Mucosa-confined lesions have very low lymphatic involvement, making them optimally treated by mucosal resection followed by ablative therapy for remaining BE. Superficial submucosal invasion (T1b sm1) has conflicting data on lymph node invasion likelihood, making surgery and/or multimodality therapy appropriate considerations. However, in patients at high esophagectomy complication risk, endoscopic therapy can be considered as an alternative, with encouraging outcomes in select patients. Well-differentiated tumors without lymphovascular invasion have the best prognosis for endoscopic therapy of T1b sm1 EAC. Mid or deep submucosal invasion (T1b sm2 or T1b sm3) is associated with high lymphatic involvement rates. Endoscopic therapy for these lesions should be considered palliative. Endoscopic therapy’s added value in multimodality therapy schemes (e.g., endoscopic therapy plus chemo/radiotherapy) is not well-described but warrants further study due to potential for local and systemic disease control.
Imaging modalities like EUS, PET, and CT scans have clearer roles. EUS can both over- and understage a significant minority of superficial EAC patients. Therefore, routine pre-EMR EUS is unwarranted, as clinical decisions are based on EMR findings. EUS may have limited role in endoscopic therapy of early esophageal neoplasia in T1b disease. For T1b disease patients considering endoscopic therapy, locoregional lymph node involvement evidence, especially if confirmed by FNA, indicates palliative endoscopic therapy and need for other modalities for curative intent. PET-CT has no demonstrated benefit in intramucosal (T1a) cancer or dysplastic BE due to low distant involvement likelihood. PET-CT may be valuable post-T1b disease diagnosis to detect distant involvement.
EMR alone is inadequate therapy for T1a or T1b EAC. Cohort studies show up to one-third of EMR-treated patients with complete primary lesion resection develop recurrent HGD or EAC. Whether these recurrences are metachronous lesions or a field effect is unclear. However, ablative treatment of remaining BE markedly decreases this risk. Therefore, all patients with successful T1a EAC resection, and select T1b lesions undergoing endoscopic therapy, should undergo subsequent ablation of the remaining BE segment, as per ACG clinical guidelines for Barrett’s esophagus.
Successful endoscopic ablative therapy is defined as complete eradication of all dysplasia and IM in the tubular esophagus. To demonstrate this, four-quadrant biopsies at the GEJ and every cm throughout the previous BE extent are taken. Cardia surveillance biopsies are also routinely performed due to neoplasia occurrence in the cardia/GEJ post-ablation. Due to random biopsy sampling error, some suggest two negative biopsy sessions before declaring complete eradication. However, no objective data define optimal complete eradication criteria regarding negative biopsy sessions.
Deciding when endoscopic ablative therapy “fails” depends on patient clinical situation, progress with initial ablation attempts, and failure mechanism. Cohort studies show that even patients undergoing four RFA sessions without complete IM eradication, >50% eventually achieve this goal with subsequent therapy, suggesting no concrete failure cutoff is advisable.
Regarding ablative modalities in BE, various modalities are effective for IM eradication. Level 1 evidence for cancer incidence prevention exists for photodynamic therapy (PDT) in HGD, RFA in HGD, and RFA in LGD. Given PDT costs and side-effect profile, and extensive data supporting RFA safety and efficacy, RFA appears preferred for most patients. This recommendation may evolve with further data. Cryotherapy shows promising cohort data with high rates of CEIM and neoplasia eradication.
Surgical Therapy
Several studies assessed antireflux surgery’s value in EAC prevention in BE. A small randomized trial showed no difference in progression outcomes between medical and surgical groups, but may have type II error. Meta-analyses reveal conflicting results, with some showing no cancer risk difference between medically and surgically managed patients, while others suggest improved outcomes in surgically treated patients. Given weak data and very low cancer incidence in nondysplastic BE, antireflux surgery should not be considered antineoplastic in BE. Indications for antireflux surgery in BE patients are the same as for general GERD patients—primarily GERD symptoms or esophagitis uncontrolled by medical therapy. PPI dosages beyond twice daily have not shown benefit in BE patients. Once-daily PPI therapy is recommended for BE patients unless GERD symptoms require twice-daily dosing for adequate symptom control, as per ACG clinical guidelines for Barrett’s esophagus.
Esophagectomy has a well-established role in BE and EAC care. It is the treatment of choice for fit candidates with T1b sm2–3 disease, alone or combined with radiation/chemotherapy. Surgical consultation should be obtained for T1a or T1b sm1 EAC patients with unfavorable prognostic factors like poor differentiation or lymphovascular invasion.
MANAGEMENT OF BE AFTER ENDOSCOPIC THERAPY
Recommendations
-
- Surveillance After CEIM: Endoscopic surveillance should continue after successful endoscopic therapy and CEIM to detect recurrent IM and/or dysplasia (strong recommendation, low level of evidence). Ongoing surveillance is crucial after endoscopic therapy for Barrett’s esophagus to detect recurrence.
-
- Surveillance Intervals After CEIM for HGD/Intramucosal Carcinoma: For patients with HGD or intramucosal carcinoma before ablation, surveillance post-CEIM is recommended every 3 months for the first year, every 6 months in the second year, and annually thereafter (conditional recommendation, low level of evidence). More frequent early surveillance is recommended for patients treated for HGD/intramucosal carcinoma.
-
- Surveillance Intervals After CEIM for LGD: For patients with LGD before ablation, surveillance post-CEIM is recommended every 6 months in the first year, and annually thereafter (conditional recommendation, low level of evidence). Surveillance intervals are less frequent for patients treated for LGD compared to HGD/intramucosal carcinoma.
-
- Detailed Endoscopic Inspection During Surveillance: During post-CEIM surveillance, careful tubular esophagus and GEJ inspection (antegrade and retrograde views) should be performed with high-resolution white light imaging and NBI to detect mucosal abnormalities indicating recurrent IM and/or dysplasia (strong recommendation, low level of evidence). Detailed endoscopic inspection with advanced imaging is crucial for recurrence detection during Barrett’s esophagus surveillance after therapy.
-
- Management of Recurrent Metaplasia/Dysplasia: Treatment of recurrent metaplasia and/or dysplasia should follow guidelines for metaplasia/dysplasia treatment in pre-ablation BE (strong recommendation, low level of evidence). Management of recurrence after endoscopic therapy follows the same principles as initial BE management.
-
- Reflux Control Post-CEIM: Post-CEIM medical antireflux therapy should aim for reflux control, defined by absence of frequent reflux symptoms (more than once a week) and/or esophagitis on endoscopy (conditional recommendation, very low level of evidence). Reflux control remains important after endoscopic therapy for Barrett’s esophagus to minimize recurrence risk and symptoms.
Summary of Evidence
Post-CEIM IM recurrence rate is not insignificant, with some cohorts showing ≥20% rates at 2–3 years. Most recurrences are nondysplastic, but up to a quarter may be dysplastic, including EAC. Recurrence rate variability may be due to differing recurrence definitions (tubular esophagus only vs. esophagus and GEJ/cardia). Recurrent IM without dysplasia at GEJ after CEIM is of unclear significance. Cohorts treated with combination therapy (EMR + ablation) or single modality therapy (EMR alone) show comparable recurrence rates. Recurrence rates also appear similar across different ablation modalities (cryotherapy, PDT).
Careful endoscopic surveillance with biopsies is recommended post-CEIM to detect recurrent IM. Careful tubular esophagus (previous BE segment region) and GEJ (antegrade and retroflexed views) inspection is important. Surveillance examination intervals and biopsy protocols are based on expert opinion and cohort study intervals. Surveillance every 3 months in the first year, 6 months in the second year, and annually thereafter is recommended for patients with baseline HGD. For baseline LGD, surveillance is recommended every 6 months in the first year and annually thereafter, as per ACG clinical guidelines for Barrett’s esophagus. Most studies use four-quadrant biopsies every cm throughout the previous BE segment with additional targeted biopsies of any abnormality, although this approach is not compared to other regimens. No evidence supports discontinuing surveillance after multiple negative endoscopies, given recurrent neoplasia reports years after CEIM in cohort studies.
Tubular esophagus and GEJ biopsies should be bottled separately for localization and treatment of recurrence. Optimal biopsy number for adequate surveillance is unknown. Despite concerns about biopsy depth post-ablation, subsquamous BE prevalence is variable after ablation (0.9% after RFA to 14.2% after PDT). Imaging techniques like OCT suggest higher subsquamous BE prevalence, particularly at GEJ, but its significance is unclear, despite subsquamous EAC case reports post-ablation. Some studies suggest post-ablation surveillance biopsies are too superficial to detect subsquamous BE, with most biopsies lacking lamina propria. This is not confirmed by other studies. It is unclear if large capacity forceps biopsies are more effective at sampling deeper neosquamous epithelium layers compared to regular forceps. While neosquamous epithelium may be more permeable than normal squamous epithelium, it does not appear to harbor genetic abnormalities.
Most recurrent metaplasia and dysplasia, when detected by surveillance, are amenable to endoscopic therapy, including EMR and additional ablation. However, a few cases requiring esophagectomy for invasive carcinoma are reported. Recurrence predictors are not well-defined, but some studies suggest older age, longer preablation BE segment, larger hiatal hernia, and higher preablation dysplasia grade are associated with higher recurrence rates.
Uncontrolled observational studies suggest incomplete reflux control may be associated with increased recurrence rates post-endotherapy. However, no conclusive evidence suggests high-dose PPI therapy or tight reflux control (ambulatory pH monitoring) lowers recurrence rates post-ablation. Most post-ablation follow-up cohorts continue patients on twice-daily PPI therapy. Reflux treatment post-ablation should follow the same principles as BE endoscopic therapy section. Medical treatment goal should be reflux symptom control and esophagitis prevention/healing.
ENDOSCOPIC ERADICATION THERAPY: TRAINING AND EDUCATION
Recommendation
-
- EMR Competency for Endoscopic Ablative Therapy Providers: Endoscopists planning to perform endoscopic ablative procedures should also offer EMR (strong recommendation, very low level of evidence). EMR competency is essential for endoscopists providing endoscopic ablative therapy for Barrett’s esophagus, according to clinical guidelines.
Summary of Evidence
Limited data exist on training and education thresholds for endoscopic ablative therapy of BE. Common sense and expert opinion suggest core competencies are needed before performing ablative therapy, which is only one component of BE patient management. Adequate training and expertise in recognizing mucosal lesions potentially harboring neoplasia is critical to target EMR. EMR of mucosal abnormalities alters pathologic stage in ∼50% of patients with clear management implications. Randomized RFA trials required EMR of mucosal abnormalities before RFA application. Post-RFA follow-up also shows nodular lesion development in some patients, warranting EMR. Expertise in recognizing and managing endoscopic therapy complications, notably bleeding, strictures, and perforation, is warranted. Offering or training in RFA for flat BE without EMR training is illogical.
Limited information exists on the learning curve for these skills. British Society of Gastroenterology guidelines recommend, based on expert opinion, a minimum of 30 supervised endoscopic resections and 30 ablations for competence. For RFA, a single endoscopist case series showed no difference in IM eradication, complications, and procedure time between early and later cases. However, a multicenter tertiary center consortium found variable CEIM rates among endoscopists, with a positive correlation between patient/RFA volume and complete remission of IM rate, but no threshold volume for success. For EMR, a Dutch multicenter study examining structured EMR training found no difference in complication rates, resection completeness, and time per resection between early and later resections. Only 29% of resections in this study used the multiband ligator approach, with the remainder using the cap technique.
CONCLUSION
BE patient care has rapidly evolved in the past decade. This analysis summarizes these advances and presents “best practices” for BE patient care, aligning with ACG clinical guideline diagnosis and management of Barrett’s esophagus. These recommendations are not practice standards or quality measures; clinical circumstances should guide optimal patient care.
These guidelines differ markedly from predecessors, notably in expanded endoscopic ablative therapy use, especially for LGD, based on high-quality evidence showing reduced progression risk post-treatment. Screening recommendations are refined based on data showing lower EAC risk in nondysplastic BE and better understanding of gender and anthropomorphic risk impacts. The most significant change is that routine screening for women with GERD symptoms is no longer recommended. Surveillance recommendations are attenuated to reflect the rare progression in nondysplastic BE and unclear benefit of endoscopic surveillance.
Several technologies will likely further evolve BE care. Key areas for paradigm shifts include biomarker development for BE risk prediction, advanced imaging/biomolecular technologies for neoplasia recognition within BE, and less invasive, cheaper BE screening modalities. These areas offer improved care at reduced costs. While the timeline is unpredictable, advances in these areas will likely markedly change future iterations of these guidelines for clinical guideline diagnosis and management of Barrett’s esophagus.