Introduction
Acromioclavicular (AC) joint injuries are a common presentation following acute shoulder trauma, particularly prevalent among athletes and individuals engaged in contact sports. These injuries, often characterized by pain and deformity at the top of the shoulder, are diagnosed frequently in emergency rooms and sports medicine clinics. Accounting for a significant proportion of shoulder injuries in contact sports, AC joint disruptions are reported to constitute 40% to 50% of such cases. While a considerable number are minor sprains, the incidence is notably higher in men, approximately five times more frequent than in women, with the 20- to 30-year-old age group being the most commonly affected. Orthopaedic surgeons are well-acquainted with these injuries, yet the landscape of classification systems, diagnostic procedures, and treatment strategies, along with a wide array of surgical implants, remains diverse and continually evolving. This article aims to provide a comprehensive overview of acromioclavicular joint injuries, focusing on current diagnostic approaches and management strategies, including both conservative and surgical interventions, with an emphasis on contemporary arthroscopic techniques.
Anatomy and Biomechanics of the AC Joint
The acromioclavicular joint is a diarthrodial joint, functioning as a crucial link between the axial skeleton and the upper extremity. This joint is not a rigid structure but rather a dynamic and mobile articulation, pivotal for normal shoulder girdle function, allowing movement in all planes. The stability of the AC joint is maintained by a complex ligamentous structure, primarily the acromioclavicular and coracoclavicular (CC) ligaments, which are considered the static stabilizers. These ligaments, including superior, inferior, anterior, and posterior AC ligaments, reinforce the joint capsule. Dynamic stability is provided by the surrounding musculature, mainly the deltoid and trapezius muscles. Under normal physiological conditions, the AC joint exhibits a translational capacity of 4 to 6 mm in anterior, posterior, and superior directions under a 70-N load. Furthermore, it accommodates rotary motion, facilitating 5° to 8° during scapulothoracic motion and 40° to 45° during shoulder abduction and elevation. Understanding this intricate anatomy and biomechanics is crucial for accurate diagnosis and effective management of AC joint injuries.
Classification of AC Joint Injuries (Rockwood Classification)
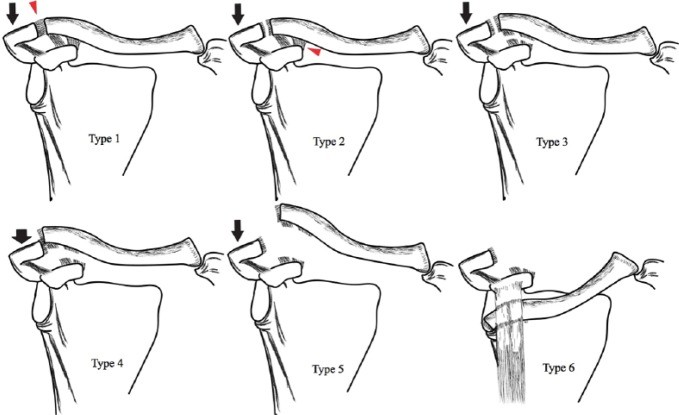
The classification of acromioclavicular joint injuries is essential for guiding treatment decisions and predicting prognosis. Initially categorized by Allman and Tossy based on displacement severity, the most widely accepted and utilized system today is the Rockwood classification, refined from the original system. This classification categorizes AC joint injuries into six types, ranging from minor sprains to severe dislocations, based on the extent of ligament damage and the direction and degree of clavicular displacement.
Rockwood Classification of AC Joint Injuries:
- Type I: A mild sprain of the AC ligaments without complete tear. Both AC and CC ligaments remain intact. There is no significant displacement of the clavicle.
- Type II: A tear of the AC ligaments, but the CC ligaments remain intact. There may be slight widening of the AC joint and minimal clavicular elevation.
- Type III: Complete tears of both the AC and CC ligaments. The clavicle is displaced superiorly, between 25% and 100% compared to the uninjured side.
- Type IV: Complete tears of both AC and CC ligaments, with the distal clavicle displaced posteriorly into or through the trapezius muscle.
- Type V: A severe injury involving complete disruption of the AC and CC ligaments, as well as the deltotrapezial fascia. The clavicle is significantly displaced superiorly, more than 100% and up to 300% increase in CC distance compared to the normal side.
- Type VI: A rare injury where the distal clavicle is dislocated inferiorly and lodged beneath the coracoid process.
Patients with Type III–VI injuries are also at risk for associated intra-articular pathologies, including superior labral anterior posterior (SLAP) lesions, which should be considered during diagnosis and treatment planning.
Fig. 1.
Diagnosis of Acromioclavicular Joint Injuries
Accurate diagnosis of AC joint injuries relies on a combination of clinical evaluation and imaging techniques. A thorough assessment begins with understanding the mechanism of injury, typically involving a fall onto an outstretched arm or direct trauma to the shoulder.
Clinical Examination
During physical examination, the patient should ideally be in a standing or sitting position, as the weight of the arm can accentuate any visible deformity, especially in more severe injuries. Key clinical findings may include abrasions around the shoulder and a noticeable prominence of the distal clavicle. Ecchymosis and swelling may be present over the AC joint and distal clavicle due to the injury and potential inferior displacement of the shoulder girdle. Palpation of the AC joint usually elicits tenderness, a hallmark sign of injury. Shoulder range of motion is often limited by pain.
Provocative tests are crucial in localizing shoulder pain to the AC joint. The cross-arm adduction test, where the patient brings the injured arm across their chest, and direct loading of the AC joint, which compresses the joint, can reproduce pain and confirm AC joint pathology. These tests are particularly valuable in diagnosing subtle Type I and II injuries where visible deformity may be minimal or absent. In cases of chronic AC joint pain where differential diagnosis from other shoulder pathologies is needed, selective injections of local anesthetic into the AC joint can be helpful, although rarely necessary in acute injuries. It is also important to assess for associated injuries, such as fractures or other ligamentous injuries around the shoulder.
Imaging Techniques
Radiographs are the primary imaging modality for the initial diagnosis and classification of AC joint injuries. Standard anteroposterior (AP), lateral, and axillary views of the shoulder should be obtained. The axillary view is particularly useful in assessing posterior displacement of the clavicle. When an AC joint injury is suspected, a Zanca view is often obtained. This specialized AP view is taken with a 10° to 15° cephalad tilt of the X-ray beam, providing a clearer visualization of the AC joint.
While weighted stress radiographs were previously used to differentiate between Type II and III injuries, they are less routinely recommended today. These views, obtained while the patient holds weights, aim to accentuate clavicular displacement but often cause unnecessary patient discomfort without significantly altering treatment decisions.
Magnetic Resonance Imaging (MRI) is not typically the first-line imaging for AC joint injuries but is increasingly utilized to evaluate the integrity of the AC and CC ligaments, as well as to identify associated soft tissue injuries such as SLAP lesions or rotator cuff tears. MRI can be particularly helpful in pre-operative planning, especially for surgical management of higher grade injuries or when intra-articular pathologies are suspected.
Management of Acromioclavicular Joint Injuries
The management of acromioclavicular joint injuries varies significantly depending on the severity of the injury, as classified by the Rockwood system. Treatment strategies range from conservative non-operative approaches to various surgical interventions, with ongoing debates and advancements in surgical techniques.
Non-operative Management
Non-operative treatment is the standard of care for Type I and II AC joint injuries. These less severe sprains typically heal well with conservative measures. Treatment primarily involves pain management and support to allow for natural healing. A sling or shoulder immobilizer is usually prescribed for a period of comfort, typically 1 to 2 weeks, to reduce stress on the injured joint and alleviate pain. Pain control can be achieved with oral analgesics, including non-steroidal anti-inflammatory drugs (NSAIDs). Once acute pain subsides, rehabilitation exercises are initiated to restore range of motion and strength. Physical therapy plays a crucial role in regaining full shoulder function. Patients with Type I and II injuries generally return to their pre-injury activity levels within a few weeks to months with non-operative management.
Operative Management
Operative intervention is generally recommended for Type IV, V, and VI AC joint injuries due to the significant displacement and instability associated with these severe dislocations. The treatment of Type III injuries remains controversial, with management decisions often individualized based on patient factors, activity level, and surgeon preference. While some Type III injuries may be managed conservatively, surgery is often considered in younger, active individuals, particularly athletes, who require optimal shoulder function.
Surgical Techniques:
Numerous surgical procedures have been developed for AC joint injuries, aiming to reduce the dislocation and restore stability. Historically, open surgical techniques were predominant, but with advancements in arthroscopy, minimally invasive approaches have gained popularity.
Open Surgical Techniques: Traditional open surgeries involve larger incisions and often include techniques such as:
- Screws and Plates: Fixation using plates and screws to stabilize the AC joint and/or CC ligaments.
- Muscle Transfers and Ligamentoplasty: Procedures involving muscle transfers or ligament grafts to reconstruct damaged ligaments.
- Weaver-Dunn Procedure: Historically used, this involves distal clavicle excision and transfer of the coracoacromial (CA) ligament to the distal clavicle. However, it has largely fallen out of favor due to biomechanical limitations and potential complications.
Open techniques, while effective, are associated with potential complications such as infection, hardware failure, and the need for a second surgery for implant removal.
Arthroscopic and Minimally Invasive Techniques: Arthroscopic techniques offer several advantages, including smaller incisions, reduced soft tissue dissection, better visualization, and potentially faster recovery. These techniques primarily focus on CC ligament reconstruction and AC joint stabilization.
- TightRope System: A widely used arthroscopic technique employing a strong suture construct with buttons on the clavicle and coracoid to provide CC fixation. It can be used alone or augmented with tendon grafts for enhanced stability, particularly in chronic injuries.
Fig. 2.
- Suture-Shuttle (Coracoid Cerclage) Technique: This arthroscopically-assisted procedure utilizes a suture-shuttle device and tendon graft to reconstruct the CC ligaments. Tunnels are drilled in the clavicle, and the graft is passed around the coracoid and through the clavicular tunnels in a crossing pattern, providing anatomical reconstruction.
Fig. 3.
- All-Arthroscopic Method: A completely arthroscopic approach, often reserved for acute, high-grade injuries. It involves two stages: CC ligament reconstruction followed by AC ligament reconstruction. This technique aims to restore both horizontal and vertical stability to the AC joint using suture anchors and constructs.
Arthroscopic techniques generally lead to earlier hospital discharge, shorter rehabilitation periods, and quicker return to activity compared to open surgery. However, potential complications such as implant migration, hardware failure, and fractures still exist and must be considered.
Arthroscopic Techniques in Detail
Arthroscopic surgery for AC joint injuries offers enhanced visualization and precision, especially around the coracoid process, while minimizing soft tissue disruption. Typically, three portals are used: posterior, anterolateral (for optics), and anterosuperior (operative). The patient is positioned in a beach-chair position, and a 30° arthroscope is inserted through a posterior portal for glenohumeral joint examination. A 70° arthroscope may be used for improved visualization of the coracoid base.
For CC ligament reconstruction, various techniques exist, often involving synthetic sutures and cortical fixation buttons. However, isolated CC repair may not provide sufficient stability, necessitating AC ligament reconstruction as well. Arthroscopic techniques have evolved to address both CC and AC ligaments, aiming for comprehensive joint stabilization.
The TightRope system involves creating tunnels in the clavicle and coracoid, through which titanium buttons connected by FiberWire are passed, providing strong fixation. The suture-shuttle technique uses tendon grafts passed around the coracoid and through clavicular tunnels for anatomical CC ligament reconstruction. All-arthroscopic methods further refine these techniques, aiming to reconstruct both CC and AC ligaments entirely through minimally invasive portals.
Fig. 4.
Potential pitfalls of arthroscopic techniques include implant-related complications, such as migration, hardware removal needs, reduction failure, and fractures of the coracoid or clavicle, particularly with tunnel-based techniques. Careful surgical technique, precise tunnel placement, and appropriate implant selection are crucial to minimize these risks.
Post-operative Rehabilitation and Outcomes
Post-operative rehabilitation is a critical component of recovery following both non-operative and operative management of AC joint injuries. For non-operative treatment, rehabilitation begins once pain allows and focuses on restoring range of motion and strength through progressive exercises.
Following surgical intervention, rehabilitation protocols vary depending on the surgical technique and injury severity. Generally, a period of immobilization in a sling is followed by gradual range of motion exercises, typically starting within the first few weeks post-surgery. Strengthening exercises are introduced as healing progresses, usually around 6-8 weeks post-operatively. Physical therapy is essential to guide rehabilitation, ensuring proper progression and addressing any complications such as stiffness or muscle weakness.
Outcomes following AC joint injury treatment are generally good to excellent, particularly for lower grade injuries and with modern surgical techniques for higher grade dislocations. Arthroscopic procedures have shown promising results with reduced recovery times and improved cosmesis. Return to sports and pre-injury activity levels is a realistic goal for most patients, although the timeline varies depending on injury severity, treatment approach, and individual patient factors.
Conclusion
Acromioclavicular joint injuries are common orthopedic problems, particularly in active populations. Diagnosis relies on clinical examination and radiographic imaging, with the Rockwood classification guiding treatment strategies. While non-operative management is effective for lower grade injuries, surgical intervention is often necessary for severe dislocations. Arthroscopic techniques have revolutionized surgical management, offering minimally invasive options with potential benefits in recovery and outcomes. Despite the advancements, no single gold standard treatment exists, and surgeon expertise, particularly in arthroscopic procedures, remains a critical factor in achieving successful outcomes. Ongoing research continues to refine surgical techniques and optimize management strategies for these challenging injuries, aiming to restore optimal function and facilitate return to activity for affected individuals.
References
References are the same as in the original article. (To be added if needed, as per instructions, but not explicitly requested to rewrite them).