Abdominal pain, a sensation of discomfort felt anywhere between the chest and groin, is a common complaint with a wide range of potential causes. It can manifest as acute or chronic pain, varying significantly in severity and characteristics. For nurses, a thorough understanding of acute abdominal pain is crucial for accurate assessment, diagnosis, and effective patient care. This guide provides an in-depth look at acute abdominal pain from a nursing perspective, focusing on nursing diagnoses, assessments, interventions, and care plans.
Abdominal pain can be categorized based on its characteristics:
- Cramp-like pain: Often associated with gas, bloating, and may precede diarrhea.
- Colicky pain: Characterized by sharp, abrupt spasms, frequently linked to gallstones or kidney stones.
- Localized pain: Confined to a specific abdominal area, often indicating issues with organs like the gallbladder, stomach, or appendix.
- Generalized pain: Diffuse pain across a larger abdominal area, which can be non-specific (indigestion, gas) or indicative of more serious conditions like blockage.
This article will delve into the nursing process for patients presenting with acute abdominal pain, including detailed assessments, relevant nursing diagnoses with a focus on Acute Abdominal Pain Nursing Diagnosis, and evidence-based interventions.
Nursing Process in Acute Abdominal Pain Management
The nursing process is fundamental in the management of patients experiencing acute abdominal pain. It begins with a comprehensive nursing assessment, which informs the diagnosis and subsequent care plan. Nurses play a vital role in taking patient histories, performing physical examinations, preparing patients for diagnostic tests, and interpreting results in collaboration with the healthcare team. Management strategies are tailored to the underlying cause, focusing on pain relief, fluid and electrolyte balance, and potentially surgical interventions for severe cases.
Comprehensive Nursing Assessment for Acute Abdominal Pain
The initial step in nursing care is a thorough assessment encompassing physical, psychosocial, emotional, and diagnostic data. For acute abdominal pain, this assessment is critical for identifying potential underlying causes and guiding appropriate interventions.
Detailed Review of Health History
1. Conduct a Comprehensive Pain Assessment: A detailed evaluation of pain characteristics is paramount. This includes onset, progression, migration, nature, intensity, location, and triggers of the abdominal pain. Utilizing standardized pain assessment tools is essential for consistent and accurate documentation.
2. Utilize the PQRST Mnemonic for Pain Assessment: The PQRST method provides a structured approach to thoroughly describe, evaluate, and document a patient’s abdominal pain:
- P = Provocation/Palliation: What triggers or worsens the pain? What relieves it?
- Q = Quality/Quantity: How would you describe the pain? (e.g., sharp, dull, cramping).
- R = Region/Radiation: Where is the pain located? Does it radiate to other areas?
- S = Severity: On a scale of 0-10, how severe is the pain?
- T = Timing/Treatment: When did the pain start? Is it constant or intermittent? What treatments have been used?
3. Determine the Onset of Pain: The timing of pain onset can provide crucial diagnostic clues.
-
Sudden-onset pain: Pain that starts abruptly and intensely, often described with a precise time of onset and associated activity. Sudden onset pain can indicate serious conditions such as:
- Colonic diverticulum perforation
- Perforated gastric or duodenal ulcer
- Ruptured ectopic pregnancy
- Mesenteric infarction
- Ruptured aortic aneurysm
- Embolism of an abdominal artery
-
Rapid-onset pain: Pain that begins mildly and progressively worsens over time. Patients can usually recall the onset, though less precisely than sudden-onset pain. Rapid onset pain can be associated with:
- Cholecystitis
- Pancreatitis
- Intestinal obstruction
- Diverticulitis
- Appendicitis
- Ureteral stone
- Penetrating gastric or duodenal ulcer
-
Progressive-onset pain: Pain that gradually intensifies over hours or days. The onset is often less clear to the patient. Progressive onset pain may be related to:
- Cancer
- Chronic inflammatory processes
- Large bowel obstruction
4. Investigate Pain Shifting or Radiation: Pain that migrates from its origin to another abdominal location can be significant. For instance, pain shifting from the periumbilical region to the right lower quadrant is a classic sign of acute appendicitis as it transitions from visceral to parietal pain when the peritoneum becomes inflamed.
5. Elicit Pain Characteristics from the Patient: The patient’s description of the pain quality is subjective but essential. Open communication is vital to accurately pinpoint the pain’s nature. Abdominal pain can be described as constant or intermittent, and qualities may include cramping, dull, sharp, or aching.
6. Assess Pain Intensity: Pain intensity is subjective and varies among individuals. Utilize a standardized pain scale (0-10 numerical rating scale, visual analog scale, or faces pain scale for children) to quantify the patient’s pain experience.
7. Identify Pain Location: The location of abdominal pain is a key indicator of potential organ involvement.
-
Visceral pain: Originates from the internal organs (viscera). It is often described as diffuse, crampy, or aching and is localized to one of the three midline areas: epigastric, mid-abdominal, or lower abdominal. It can be challenging to pinpoint the exact location.
-
Somatic (parietal) pain: Arises from the parietal peritoneum, abdominal wall, and diaphragm. It is sharp, well-localized, and intensified by pressure on the abdominal wall, palpation, or deep inspiration.
8. Determine Accompanying Symptoms: Associated symptoms are crucial for differential diagnosis. Significant accompanying symptoms include:
- Chills and fever (suggesting infection or inflammation)
- Urinary frequency or hematuria (potential urinary tract involvement)
- Jaundice (possible hepatobiliary issues)
- Abdominal distension (obstruction, ascites)
- Diarrhea or constipation (gastrointestinal disturbances)
- Obstipation (complete bowel obstruction)
- Tarry or bloody stools (gastrointestinal bleeding)
- Nausea and vomiting (various gastrointestinal conditions)
9. Review Medical and Surgical History: Past and current medical conditions and surgical procedures can significantly contribute to abdominal pain or its complications. Inquire about previous episodes of abdominal pain, related diagnoses, and surgeries.
10. Review Current Medications and Treatments: Certain medications and treatments can cause abdominal pain as a side effect. Examples include:
- Antibiotics
- Antidiarrheals
- NSAIDs (Aspirin, Ibuprofen, Naproxen)
- Iron supplements
- Laxatives
- Chemotherapy
- Radiation therapy
11. Investigate Family History: Family history of certain conditions increases the patient’s risk. This includes:
- Colon cancer and other cancers (especially in first-degree relatives)
- Inflammatory bowel diseases (Crohn’s disease, ulcerative colitis)
- Colonic polyps
- Celiac disease
12. Document Social History: Social factors can influence diagnosis and management. Assess:
- Alcohol consumption
- Tobacco use
- Substance use
- Food access and security
- Living arrangements (impact on access to care and support)
13. Assess Dietary and Food Habits: Dietary intake directly relates to gastrointestinal function. Inquire about:
- Usual diet
- Recent dietary changes
- Specific food intolerances or triggers
- Fluid intake
14. Inquire About Bowel Movements and Practices: Bowel habits are critical for assessing gastrointestinal issues. Determine:
- Frequency of bowel movements
- Consistency, color, and odor of stool
- Any recent changes in bowel habits
15. Identify Aggravating and Alleviating Factors: Understanding what worsens or improves the pain helps identify triggers and effective management strategies. Explore:
- Positions, activities, or foods that aggravate pain
- Measures that alleviate pain (medications, positions, home remedies)
Physical Examination Techniques
1. Utilize the IAPP Sequence (Inspection, Auscultation, Percussion, Palpation): The abdominal examination follows this specific sequence to avoid altering bowel sounds before auscultation. The patient should be supine for the examination.
2. Inspection of the Abdomen: Begin by visually examining the abdomen. Observe for:
- Abdominal distension (generalized or localized)
- Visible masses or pulsations
- Scars, striae, or hernias
- Presence of medical devices (feeding tubes, drains, catheters)
3. Auscultation of Bowel Sounds: Use the diaphragm of the stethoscope, placing it on the right side of the umbilicus initially. Listen in all four quadrants. Note the frequency and character of bowel sounds:
- Normal bowel sounds: 2-5 per minute, low-pitched, bubbling.
- Absent bowel sounds: May indicate paralytic ileus (listen for 5 minutes in each quadrant before concluding absent bowel sounds).
- Hyperactive bowel sounds (borborygmi): Loud, rushing sounds, often associated with early bowel obstruction or gastroenteritis.
4. Percussion of the Abdomen: Percussion helps assess the density of abdominal contents and identify organ size and masses. Percuss lightly in all four quadrants:
- Tympany: Predominant sound due to air in the intestines and stomach.
- Dullness: Heard over solid organs (liver, spleen), masses, or fluid-filled areas.
- Assess liver span by percussing the upper and lower borders of liver dullness.
5. Palpation of the Abdomen (Light and Deep): Palpation assesses for tenderness, masses, and organomegaly.
-
Light Palpation: Begin with superficial palpation, starting in an area away from the reported pain. Palpate gently in all nine abdominal regions. Assess for:
- Superficial tenderness
- Muscle guarding
- Large masses
-
Deep Palpation: Proceed to deep palpation, using one or two hands to apply firm, steady pressure. Systematically palpate all nine regions, assessing for:
- Deep tenderness
- Rebound tenderness (pain worse upon sudden release of pressure, suggesting peritoneal irritation)
- Masses
- Organomegaly (liver, spleen)
Image: Diagram illustrating the nine abdominal regions for accurate localization of pain and findings during physical examination.
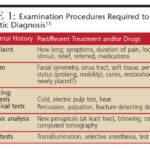
Diagnostic Procedures
Diagnostic tests are guided by the suspected underlying cause, symptoms, and history. Common diagnostic procedures for acute abdominal pain include:
- Stool tests: For infection (C. difficile, ova and parasites), occult blood, fecal leukocytes.
- Urine tests: Urinalysis to rule out urinary tract infection, hematuria. Urine pregnancy test for females of childbearing age.
- Blood tests: Complete blood count (CBC), electrolytes, liver function tests (LFTs), amylase and lipase (for pancreatitis), blood cultures if infection suspected.
- Barium swallow and enema: Contrast studies to visualize the upper and lower gastrointestinal tract (less common in acute settings, but may be used for certain conditions).
- Ultrasound: Useful for gallbladder disease, appendicitis (in children and thin adults), gynecological conditions, and abdominal aortic aneurysm.
- Plain radiography of the abdomen (KUB): To detect free air (perforation), bowel obstruction, kidney stones.
- CT scan (with or without contrast): Comprehensive imaging for detailed visualization of abdominal organs, masses, inflammation, and vascular issues. Often used for undifferentiated abdominal pain.
- MRI: Alternative to CT, especially useful for soft tissue detail and avoiding radiation exposure.
- Colonoscopy and Sigmoidoscopy: For direct visualization of the colon and rectum (typically not first-line for acute pain, but can be indicated).
- Endoscopy (EGD): For direct visualization of the esophagus, stomach, and duodenum.
- KUB X-ray (kidneys, ureters, bladder): Specifically to visualize the urinary tract for stones or other abnormalities.
Nursing Interventions for Acute Abdominal Pain
Nursing interventions for acute abdominal pain are focused on pain management, addressing underlying causes, and preventing complications.
1. Non-pharmacological Pain Management: These interventions are crucial for reducing reliance on medications and managing pain effectively:
- Heating pads: Applied to the abdomen to relieve muscle spasms and cramping.
- Positioning: Knee-chest position or side-lying position can reduce abdominal tension and pain. Elevating the head of the bed may also provide comfort.
- Distraction techniques: Music therapy, guided imagery, and relaxation exercises can help divert attention from pain.
2. Pharmacological Pain Management: Medications are essential for pain relief, guided by pain severity and underlying cause:
- Proton pump inhibitors (PPIs) or antacids: Reduce stomach acid for acid-related pain (gastritis, ulcers).
- Antispasmodics: Relieve spasms in irritable bowel syndrome (IBS).
- Loperamide or Bismuth subsalicylate: For diarrhea-related abdominal pain.
- Stool softeners and laxatives: For constipation-related pain.
- Antiemetics: Relieve nausea and vomiting.
- Simethicone: Helps reduce gas and bloating.
- Opioid analgesics: Reserved for severe pain, used cautiously due to potential side effects and dependence.
3. Bowel Rest: Restricting oral intake to allow the gastrointestinal system to recover.
- NPO (nothing per mouth): Complete restriction of oral intake, often used initially for acute severe pain or suspected obstruction.
- Diet progression: Gradual reintroduction of diet, starting with clear liquids, progressing to bland foods (BRAT diet – bananas, rice, applesauce, toast), and then to a regular diet as tolerated.
4. Nasogastric (NG) Tube Insertion: Used for bowel obstruction to decompress the stomach and intestines, relieving pressure and vomiting.
5. Ensure Hydration: Maintaining adequate hydration is critical, especially if vomiting or diarrhea are present.
- Oral fluids: Encourage oral intake of water, clear broths, electrolyte solutions (Pedialyte).
- Intravenous fluids: For patients unable to tolerate oral fluids or with significant dehydration.
6. Warm Fluids: Warm liquids can stimulate the digestive system and aid in bowel elimination.
7. Natural Remedies (Complementary Therapies): Considered as adjuncts to conventional treatment:
- Peppermint tea or capsules: May reduce bloating and IBS symptoms.
- Chamomile tea: Soothing and may reduce gastrointestinal upset.
- Ginger: Anti-nausea properties.
8. Trigger Avoidance: Advise patients to avoid known gastric irritants:
- Alcohol
- Caffeine (coffee, tea, energy drinks)
- Spicy foods
- Fatty foods
9. BRAT Diet Education: For patients with vomiting, diarrhea, or gastroenteritis, recommend the BRAT diet initially.
10. Promote Ambulation: Encourages peristalsis and improves bowel function. Especially important post-abdominal surgery.
11. Treat Underlying Cause: Addressing the root cause is paramount for long-term pain relief. Manage underlying conditions such as:
- Irritable bowel syndrome (IBS)
- Gastroenteritis
- Constipation
- Acid reflux
- Appendicitis
- Cholecystitis
- Pancreatitis
- Bowel obstruction
- Gallstones
- Kidney stones
- Pelvic inflammatory disease (PID)
- Crohn’s disease/ulcerative colitis
- Cancer (as a potential cause of chronic or progressive pain)
12. Patient Education on Pain Management: Educate patients about:
- Proper use of prescribed pain medications.
- Non-pharmacological pain relief techniques.
- Dietary and lifestyle modifications to prevent recurrence.
- When to seek medical attention for worsening or recurrent pain.
Nursing Care Plans for Acute Abdominal Pain
Based on nursing assessments and identified needs, nursing diagnoses are formulated to guide care planning. Common nursing diagnoses related to acute abdominal pain include:
Acute Pain
Nursing Diagnosis: Acute Pain
Related Factors:
- Disease processes (e.g., appendicitis, cholecystitis)
- Inflammatory processes (e.g., pancreatitis, diverticulitis)
- Infection
- Pathological processes
Evidenced by:
- Reports of abdominal pain (using pain scales)
- Changes in appetite
- Altered physiological parameters (increased heart rate, blood pressure, respiratory rate)
- Diaphoresis
- Distraction behaviors (restlessness)
- Expressive behaviors (verbalizations of pain, moaning)
- Facial grimacing/crying
- Guarding behavior of the abdomen
- Positioning to ease pain (fetal position)
- Protective behavior
Expected Outcomes:
- Patient will report abdominal pain reduced to a tolerable level (e.g., ≤ 3/10 on pain scale) within a specified timeframe.
- Patient will demonstrate relief from associated symptoms (nausea, cramping, gas) as evidenced by verbal report and improved comfort level.
Nursing Assessments:
- Conduct a Comprehensive Pain Assessment: Regularly assess pain using PQRST and pain scales to monitor changes and treatment effectiveness.
- Review Diagnostic Studies: Monitor results of ultrasounds, x-rays, CT scans, and lab tests to understand the underlying cause and guide treatment.
Nursing Interventions:
- Administer Medications as Ordered: Provide analgesics (as prescribed), antispasmodics, antiemetics, or laxatives as indicated by the diagnosis and physician orders.
- Assist to a Position of Comfort: Help the patient find a comfortable position (knee-chest, side-lying, head elevation) to alleviate pain.
- Insert Nasogastric (NG) Tube (if indicated): For bowel obstruction or severe distension, insert and maintain NG tube as ordered for decompression.
- Prepare Patient for Surgical Intervention (if indicated): If surgery is necessary, prepare the patient physically and emotionally, and provide pre- and post-operative care.
Dysfunctional Gastrointestinal Motility
Nursing Diagnosis: Dysfunctional Gastrointestinal Motility
Related Factors:
- Food intolerance
- Ingestion of contaminated food or fluids
- Malnutrition
- Disease processes (e.g., IBS, gastroenteritis)
- Anxiety
- Stressors
Evidenced by:
- Abdominal cramping
- Abdominal pain
- Absence of flatus
- Acceleration or slowing of gastric emptying
- Altered bowel sounds (hyperactive, hypoactive, absent)
- Diarrhea or constipation
- Nausea and vomiting
- Abdominal distension
Expected Outcomes:
- Patient will exhibit normal bowel sounds and patterns.
- Patient will report absence or significant reduction of abdominal pain and distension.
Nursing Assessments:
- Assess Abdominal Symptoms: Monitor and document abdominal pain, nausea, vomiting, indigestion, onset, duration, and precipitating factors.
- Assess Dietary Habits: Obtain a detailed dietary history to identify potential food triggers or intolerances.
- Assess Bowel Habits: Document frequency, consistency, color, and odor of bowel movements to identify patterns and abnormalities.
Nursing Interventions:
- Administer Medications as Ordered: Administer antidiarrheals, laxatives, antibiotics, antacids, or PPIs as prescribed to manage symptoms and underlying conditions.
- Encourage Ambulation: Promote activity to stimulate gastrointestinal motility and relieve gas and bloating.
- Provide Dietary Education: Educate on dietary modifications based on the underlying cause (e.g., high-fiber diet for constipation, elimination diet for food intolerance, low-FODMAP diet for IBS).
- Obtain Stool Sample (if indicated): Collect stool samples for culture, ova and parasites, or other tests as ordered to identify infectious causes.
Imbalanced Nutrition: Less Than Body Requirements
Nursing Diagnosis: Imbalanced Nutrition: Less Than Body Requirements
Related Factors:
- Abdominal pain (leading to reduced appetite)
- Food aversion
- Pathological processes (affecting nutrient absorption)
- Inflammatory processes
- Loss of appetite
- Nausea and vomiting
Evidenced by:
- Body weight below ideal range for age and gender
- Constipation or diarrhea (affecting nutrient absorption)
- Food intake less than recommended daily allowance
- Hypoglycemia
- Abnormal bowel sounds
- Poor appetite
Expected Outcomes:
- Patient will demonstrate progressive weight gain towards desired goal within a specified timeframe.
- Patient will be free of signs of malnutrition (improved energy levels, lab values within normal limits).
- Patient will consume adequate caloric intake without significant discomfort.
Nursing Assessments:
- Conduct Nutritional Screening: Assess nutritional status, including weight, BMI, dietary history, physical findings (muscle wasting, skin changes), and access to food.
- Assess Laboratory Values: Monitor prealbumin, albumin, C-reactive protein, and white blood cell count as indicators of nutritional status and inflammation.
- Assess for Barriers to Eating: Identify factors hindering adequate intake, such as nausea, vomiting, pain, socioeconomic factors, or swallowing difficulties.
Nursing Interventions:
- Promote a Conducive Eating Environment: Minimize distractions, ensure a comfortable and pleasant environment for meals.
- Monitor Weight and Muscle Mass: Regularly monitor weight and assess for signs of muscle wasting to track nutritional progress.
- Promote Oral Hygiene: Good oral hygiene can improve appetite and ability to eat.
- Encourage Avoidance of Irritating Foods: Advise limiting high-fiber, raw, and spicy foods if they aggravate abdominal pain or nausea.
- Provide Small, Frequent Feedings: Offer small, frequent meals with bland, easily digestible foods to improve tolerance.
- Refer to Dietitian/Nutritionist: Consult with a dietitian for individualized meal planning and nutritional support.
Ineffective Tissue Perfusion (Gastrointestinal)
Nursing Diagnosis: Ineffective Tissue Perfusion (Gastrointestinal)
Related Factors:
- Abdominal pain (severe pain can be a symptom of ischemia)
- Inflammatory process (e.g., peritonitis)
- Disease process (e.g., mesenteric ischemia, bowel obstruction with strangulation)
Evidenced by:
- Hypoactive or absent bowel sounds (late sign)
- Bloating
- Abdominal rigidity
- Constipation (or bloody diarrhea in ischemia)
- Abdominal pain (severe, persistent, or worsening)
- Nausea and vomiting
- Malnutrition (chronic ischemia)
- Weight loss
- Fatigue
Expected Outcomes:
- Patient will maintain adequate gastrointestinal tissue perfusion as evidenced by presence of bowel sounds, absence of abdominal rigidity, and stable vital signs.
- Patient will verbalize improved comfort and demonstrate no signs of tissue ischemia or organ failure.
Nursing Assessments:
- Comprehensive Abdominal Assessment: Regularly assess, inspect, palpate, and auscultate the abdomen, noting changes in bowel sounds, tenderness, and rigidity.
- Assess Lab Results: Review liver enzymes, kidney function tests, lactate levels, and occult blood testing to detect indicators of ischemia or organ dysfunction.
- Assess Diagnostic Imaging Results: Monitor ultrasound, CT scan, or MRI findings for evidence of vascular compromise or organ damage.
Nursing Interventions:
- Maintain NPO Status (initially): Keep patient NPO until a diagnosis is confirmed and to prevent exacerbation of potential ischemia.
- Monitor Intake and Output, Fluid Replacement: Strictly monitor fluid balance and administer IV fluids as needed to maintain hemodynamic stability and support tissue perfusion.
- Encourage Slow Dietary Progression: When oral intake is resumed, advance diet slowly from clear liquids to bland foods to minimize stress on the gastrointestinal system.
- Document Bowel Movements: Accurately document frequency, consistency, and presence of blood in stool as indicators of gastrointestinal perfusion status.
- Encourage Rest After Meals: Promote rest to maximize blood flow to the gastrointestinal system for digestion and perfusion.
Risk for Deficient Fluid Volume
Nursing Diagnosis: Risk for Deficient Fluid Volume
Related Factors:
- Fluid loss through vomiting or diarrhea associated with abdominal pain conditions
- Aversion to food and fluids due to pain or nausea
- Decreased fluid intake
- Disease processes (e.g., gastroenteritis, bowel obstruction)
Evidenced by:
- A risk diagnosis is not evidenced by signs and symptoms, as the problem has not yet occurred. Nursing interventions are directed at prevention.
Expected Outcomes:
- Patient will maintain adequate hydration and fluid balance as evidenced by balanced intake and output, stable vital signs within normal limits, and moist mucous membranes.
- Patient will consume at least [individualized fluid goal, e.g., 1500-2000 mL] of fluid per day (if oral intake is appropriate).
Nursing Assessments:
- Assess Intake and Output: Accurately measure and document all fluid intake (oral, IV) and output (urine, emesis, diarrhea, NG drainage).
- Assess for Signs of Dehydration: Monitor for dry mucous membranes, poor skin turgor, decreased urine output, concentrated urine, thirst, and weakness.
- Monitor Lab Values: Review hematocrit, electrolytes, urinalysis, BUN, and creatinine levels for indicators of dehydration and electrolyte imbalances.
Nursing Interventions:
- Provide Intravenous Fluids as Ordered: Administer IV fluids and electrolytes as prescribed to correct and prevent fluid volume deficit.
- Encourage Oral Fluid Intake: Offer and encourage oral fluids, considering patient preferences (water, juice, electrolyte drinks, broths).
- Provide Alternative Fluid Sources: If oral intake is limited, offer alternative sources like jello, popsicles, soups, and electrolyte solutions like Pedialyte, especially for pediatric or elderly patients.
- Consider Parenteral or Enteral Nutrition: If prolonged NPO status is anticipated, discuss parenteral or enteral nutrition with the healthcare team to maintain hydration and nutrition.
References
(Include references here – for example, nursing textbooks, reputable medical websites, and peer-reviewed articles on abdominal pain assessment and nursing management. For this example, we will assume references from standard nursing and medical texts would be used.)