Attention-deficit hyperactivity disorder (ADHD) is a prevalent neurodevelopmental condition impacting a significant portion of the adult population. As awareness of ADHD grows, so does the demand for accurate and timely diagnosis. However, traditional diagnostic pathways often face bottlenecks due to a shortage of specialists and time-consuming assessment processes. Artificial intelligence (AI) offers a promising solution to streamline and enhance ADHD diagnosis, potentially revolutionizing mental healthcare accessibility and efficiency. This article delves into the cutting-edge advancements in Ai Adhd Diagnosis, exploring a hybrid AI algorithm designed to assist clinicians, improve diagnostic accuracy, and address the growing needs of adults seeking ADHD assessment.
Understanding ADHD and Diagnostic Bottlenecks
ADHD in adults is characterized by persistent patterns of inattention, hyperactivity, and impulsivity that significantly impair daily functioning across various life domains. These symptoms can manifest as difficulties in executive functions, emotional regulation, and motivation, impacting relationships, employment, and overall well-being. The global need for ADHD diagnostic services is escalating, driven by increased public awareness and potentially exacerbated by factors such as the recent pandemic. In the UK, where the research discussed in this article is being trialed, ADHD affects an estimated 2% of adults, highlighting the substantial population requiring support.
Timely and accurate diagnosis is crucial because delayed intervention for ADHD can have detrimental consequences. Untreated ADHD is linked to a higher risk of broader mental health conditions, relationship problems, employment instability, substance misuse, and even increased mortality rates. Recognizing and addressing ADHD early can significantly improve outcomes and quality of life for affected individuals.
However, the current diagnostic landscape faces significant challenges. The scarcity of clinicians adequately trained in adult ADHD diagnosis creates a major bottleneck in healthcare systems. This shortage leads to excessively long waiting times for assessment, often stretching to years, placing a considerable economic strain on healthcare services and society as a whole. The substantial annual cost per person associated with untreated ADHD underscores the urgent need for more efficient and accessible diagnostic solutions.
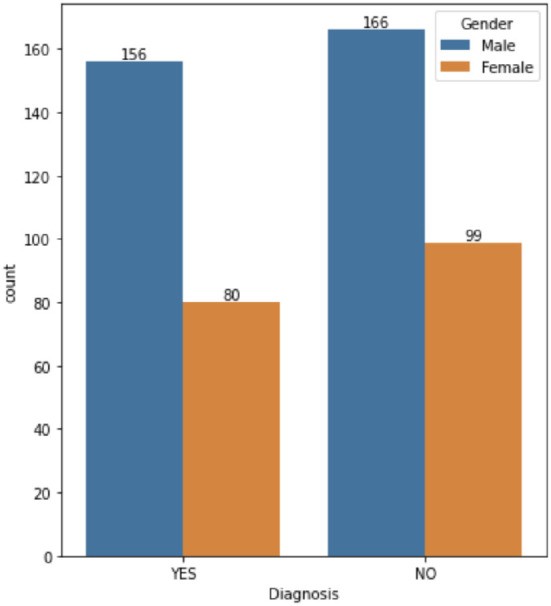
Figure 1: Gender distribution in ADHD cases, illustrating the prevalence across both male and female populations.
The Rise of AI in Mental Health and ADHD Diagnosis
Artificial intelligence is increasingly recognized for its transformative potential across various medical fields, including mental health. In the context of ADHD diagnosis, AI offers the opportunity to overcome existing limitations by automating aspects of the diagnostic process, improving accuracy, and prioritizing complex cases for specialist attention. Machine learning (ML) algorithms, a core component of AI, can analyze vast datasets of clinical information to identify patterns and predict diagnostic outcomes. Knowledge-based systems, another AI approach, can incorporate expert clinical knowledge into rule-based frameworks, providing interpretable and transparent decision-making processes.
The integration of AI in healthcare is particularly promising for conditions like ADHD, where subjective assessments and clinician expertise play a crucial role. AI systems can act as decision support tools, augmenting clinician capabilities rather than replacing them entirely. This collaborative approach can lead to more efficient workflows, reduced diagnostic delays, and ultimately, improved patient care.
NeuroIntel: An AI System for Adult ADHD Diagnosis
In response to the growing challenges in ADHD diagnosis, an innovative AI system named NeuroIntel has been developed. This system is designed to function as a decision support tool within clinical pathways, aiming to automate initial diagnostic assessments and prioritize patients based on the complexity of their cases. NeuroIntel utilizes a hybrid AI algorithm, combining the strengths of both machine learning and knowledge-based models. The development of NeuroIntel leverages clinical data collected from a UK National Health Service (NHS) adult ADHD service, ensuring alignment with established clinical guidelines and best practices.
Machine Learning Model
The machine learning component of NeuroIntel employs decision tree algorithms, chosen for their robust performance and inherent interpretability. Decision trees learn from data by recursively partitioning it based on the most informative features, creating a set of IF-THEN rules that mimic clinical reasoning. This transparency is crucial in healthcare settings, allowing clinicians to understand the AI’s decision-making process and build trust in its recommendations.
The ML model is trained on a comprehensive dataset comprising demographic information, self-report questionnaires, and clinical interview results routinely collected during ADHD assessments. These features include measures from the Mood Disorder Questionnaire (MDQ), HELPS brain injury screening tool, Drug Abuse Screening Test (DAST-10), GAD-7 anxiety scale, Patient Health Questionnaire (PHQ-9) depression scale, Iowa Personality Disorder Screen (IOWA), Alcohol Use Disorders Identification Test (AUDIT), and Conner’s ADHD Rating Scales (CAARS). The model’s output is a binary diagnostic outcome: “Yes” (ADHD likely) or “No” (ADHD unlikely).
Figure 2: Age distribution of patients in the dataset, highlighting the range of ages seeking ADHD diagnosis.
Knowledge-Based Model
Complementing the machine learning model, NeuroIntel incorporates a knowledge-based model that encodes the expertise of an international ADHD specialist. This model utilizes IF-THEN rules derived from interviews with the expert, capturing their deep understanding of ADHD assessment tools and diagnostic criteria. The knowledge model prioritizes the Diagnostic Interview for ADHD in Adults (DIVA) scores, recognizing their significance in ADHD diagnosis. It also considers potential comorbidities, such as substance abuse, personality disorders, and mood disorders, which can present with overlapping symptoms.
The knowledge model operates by setting thresholds for various clinical measures and prioritizing rules to emulate clinical decision-making. Unlike the ML model’s binary output, the knowledge model provides three possible outcomes: “Yes,” “No,” or “Expert Referral.” The “Expert Referral” outcome is triggered when the model identifies complex cases requiring further in-depth clinical evaluation by a specialist.
Hybrid Model
The NeuroIntel system culminates in a hybrid model that integrates the outputs of both the machine learning and knowledge-based models. This integration leverages the data-driven insights of machine learning with the expert knowledge and interpretability of the rule-based system. The hybrid model provides a “Yes” or “No” diagnosis only when both the ML and knowledge models are in agreement, ensuring a higher level of confidence in the outcome. In cases of disagreement or when the knowledge model flags a case as “Expert Referral,” the hybrid model appropriately refers the patient for specialist review.
The hybrid approach offers several advantages. It maximizes diagnostic accuracy by combining different AI methodologies. It enhances transparency by incorporating expert-derived rules. Crucially, it ensures patient safety by directing complex cases to experienced clinicians, maintaining human oversight in the diagnostic process. This framework aims to optimize resource allocation, allowing AI to handle clear-cut cases while reserving specialist time for those requiring more nuanced assessment.
Figure 4: Visual representation of the diagnostic pathway, highlighting (A) current bottlenecks and (B) how AI integration can streamline the process.
Evaluating AI Performance: Results and Discussion
The performance of NeuroIntel’s AI models has been rigorously evaluated using a dataset of 501 anonymized adult ADHD assessments. The study focused on assessing the accuracy of the machine learning model, the knowledge-based model, and the hybrid model in predicting ADHD diagnosis. Furthermore, the research investigated the effectiveness of diagnostic assessments without relying on the DIVA interview, which is known to be resource-intensive due to its requirement for specially trained senior clinicians.
Performance with Full Data (including DIVA)
When utilizing all available clinical data, including DIVA scores, the machine learning model achieved a test accuracy of 75.03%. This indicates that the ML model correctly classified approximately three out of every four cases. The hybrid model, combining the ML and knowledge-based components, demonstrated significantly higher accuracy, reaching 93.61%. This substantial improvement highlights the synergistic effect of integrating data-driven learning with expert clinical knowledge.
The machine learning model employed in this analysis was a decision tree, selected after comparing various algorithms, including logistic regression, support vector machines, and neural networks. Decision trees offer a balance of accuracy and interpretability, making them well-suited for clinical applications. While more complex models like Random Forest and Extreme Gradient Boosting achieved perfect accuracy on training data, indicating potential overfitting, the decision tree provided robust generalization to unseen data.
Figure 6: Correlation analysis of top 20 attributes, showing DIVA scores as highly correlated with ADHD diagnosis.
Performance without DIVA
Recognizing the practical challenges associated with DIVA administration, the study also evaluated the performance of the AI models when DIVA scores were excluded from the dataset. In this scenario, the best-performing machine learning model achieved an accuracy of 65.27%. While lower than the accuracy achieved with full data, this result is still significantly better than chance and suggests that AI can provide useful diagnostic support even without DIVA assessments.
The reduction in accuracy when DIVA is removed underscores the importance of DIVA in current diagnostic practice and the information it provides. However, an accuracy of 65.27% without DIVA is encouraging, particularly considering the potential for cost savings and increased accessibility if less resource-intensive screening methods can be effectively utilized with AI support. Further research is warranted to explore alternative clinical measures and AI techniques to enhance diagnostic accuracy in the absence of DIVA.
Figure 8: Correlation analysis of top 20 attributes excluding DIVA, showing lower correlation strengths compared to analysis including DIVA.
Hybrid Model Superiority
The consistently superior performance of the hybrid AI model compared to the machine learning model alone emphasizes the value of integrating expert knowledge into AI systems for ADHD diagnosis. The hybrid model’s ability to achieve over 93% accuracy with full data demonstrates the potential for AI to significantly enhance diagnostic precision and efficiency. Even without DIVA, the hybrid approach, if further developed with a DIVA-independent knowledge model, holds promise for improving diagnostic accuracy beyond what machine learning alone can achieve.
The findings suggest that AI, particularly hybrid systems like NeuroIntel, can play a crucial role in addressing the diagnostic challenges in adult ADHD. By automating initial assessments and prioritizing complex cases, AI can help reduce waiting times, improve resource allocation, and ultimately enhance access to timely and appropriate mental healthcare for adults with ADHD.
Ethical Considerations of AI ADHD Diagnosis
As AI becomes increasingly integrated into healthcare, ethical considerations are paramount. The development and deployment of AI systems for ADHD diagnosis must prioritize data protection, algorithmic fairness, and accountability. The NeuroIntel project has proactively addressed these ethical dimensions.
Data privacy is ensured through anonymization of patient records and adherence to strict data governance principles. Algorithmic fairness is addressed through careful dataset curation, cross-validation techniques to mitigate bias, and transparent model development. The use of interpretable decision tree models and rule-based systems enhances accountability by allowing clinicians to understand the AI’s reasoning.
Furthermore, NeuroIntel is designed as a decision support tool, not an autonomous diagnostic entity. Clinician oversight remains central to the diagnostic process, ensuring that AI recommendations are carefully reviewed and integrated into comprehensive clinical assessments. This human-in-the-loop approach is crucial for maintaining ethical standards and ensuring responsible AI implementation in mental healthcare.
Conclusion: AI as a Catalyst for Improved ADHD Care
This research demonstrates the significant potential of AI to revolutionize ADHD diagnosis in adults. The NeuroIntel hybrid AI system, leveraging both machine learning and expert knowledge, has shown impressive accuracy in assisting clinicians. The findings encourage the continued development and clinical implementation of AI-powered tools to address the growing demand for ADHD diagnostic services and improve patient outcomes.
Future research directions include expanding clinical trials to diverse healthcare settings, conducting in-depth ethical risk assessments, and further refining the knowledge-based model to enhance its flexibility and robustness. Developing a DIVA-independent knowledge model is a key priority to broaden the applicability and cost-effectiveness of AI-assisted ADHD diagnosis. Ultimately, the goal is to create AI solutions that are not only accurate and efficient but also ethically sound and seamlessly integrated into clinical workflows, empowering healthcare professionals to provide the best possible care for individuals with ADHD.
Data Availability Statement
The datasets presented in this article are not readily available because in the interests of protecting patients’ privacy, the data cannot be shared. Requests to access the datasets should be directed to MA, [email protected].
Ethics Statement
Ethical approval was waived by South West Yorkshire Partnership Foundation Trust (SWYPFT) Research and Development Department as data were gathered retrospectively. Written informed consent was not required in accordance with institutional requirements and national legislation.
Author Contributions
TC: formal analysis, literature research, methodology, validation, and writing—draft and review. IT: formal analysis, methodology, validation, and writing—draft and review. SB and EP: writing—review and editing. MA: conceptualization and methodology. GA: conceptualization, methodology, and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding Statement
This research was partially supported by the Federal Ministry of Education and Research (BMBF), Germany under the project LeibnizKILabor with Grant No. 01DD20003.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
[References from original article – kept for completeness]
Associated Data
Data Availability Statement
The datasets presented in this article are not readily available because in the interests of protecting patients’ privacy, the data cannot be shared. Requests to access the datasets should be directed to MA, [email protected].