Demographic Data and AMS Prevalence
Altered Mental Status (AMS), a critical medical condition frequently encountered in emergency departments (EDs), is indicated by the medical abbreviation AMS. While studies suggest AMS may present in 4%–10% of all ED patients, with higher rates among specific populations such as the elderly, our recent research at xentrydiagnosis.store reveals a significantly lower incidence. Our findings showed AMS in only 0.93% of total emergency patients and 2.38% within the elderly subgroup (patients over 65). This notable difference from previous reports could stem from stricter inclusion criteria applied in our study. Additionally, a segment of patients with intellectual disabilities, often identified through the Mini-Mental State Examination (MMSE), might not have been fully captured due to the MMSE’s infrequent use in acute emergency settings.
Interestingly, our analysis of age distribution among AMS patients revealed a bimodal pattern, with peaks around 33 years and 72 years of age. This distribution underscores the diverse underlying causes of AMS across different age demographics. Further investigation into the etiology of AMS revealed distinct patterns between elderly and non-elderly groups. In younger individuals, AMS was more frequently associated with metabolic disorders, trauma, and poisoning. Conversely, older patients presented with AMS more often due to cerebrovascular diseases and organ or systemic failures. This age-related variance in AMS etiology aligns with existing research on acute AMS.
Emergency Assessment and Diagnostic Challenges of AMS
The emergency assessment of Altered Mental Status (AMS), a critical aspect of patient care signified by the medical abbreviation AMS, presents considerable challenges. Emergency physicians often face hurdles due to incomplete or inaccurate patient histories, particularly as focus is often directed towards acute physical ailments, potentially overlooking subtle yet crucial details of acute mental status changes. Compounding this issue is the alarming rate of misdiagnosis in AMS patients. Studies indicate that misdiagnosis can be as high as 75% in elderly patients over 65 presenting with delirium, a condition closely related to AMS. Reports also highlight instances where patients initially admitted to psychiatric wards require emergency medical transfers, underscoring the need for enhanced AMS assessment skills among emergency medical professionals.
Research emphasizes that a thorough medical history and physical examination are paramount in the diagnostic process of AMS, often outweighing the immediate reliance on laboratory tests and imaging. Physical examinations are instrumental not only in initial diagnosis but also in monitoring the progression of the condition. A comprehensive approach, incorporating medical history, physical examination, past medical records, and patient responses to initial treatments, is crucial for effectively determining the underlying causes of AMS. Our data from xentrydiagnosis.store supports this, indicating that utilizing these four fundamental assessment tools can lead to a clear diagnosis of the AMS cause in approximately 60% of emergency cases. While Computed Tomography (CT) scans are valuable for identifying intracranial space-occupying lesions, hemorrhages, and structural brain damage, a significant proportion of AMS patients exhibit negative CT findings.
In our study, the diagnostic yield of CT scans in determining AMS etiology was only 15%. Over-reliance on CT imaging in AMS diagnosis carries the risk of negatively impacting the timely assessment and treatment of non-neurological factors contributing to AMS, such as hypoglycemia. However, the importance of CT head scans should not be dismissed entirely. Even with negative reports, CT scans can be crucial in specific AMS cases, particularly in acute poisoning scenarios, to rule out concurrent brain injuries. Our findings, showing a high negative rate for CT head scans in AMS diagnosis, suggest that emergency physicians are increasingly recognizing the limitations of CT scans as a primary diagnostic tool for AMS, thereby avoiding delays in assessment and treatment while awaiting CT results.
The role of Electroencephalography (EEG) in emergency AMS assessment remains less defined. In our study, EEG application in AMS patients was notably low at just 1%, considerably less than previously reported rates. Studies investigating cerebrospinal fluid (CSF) analysis in acute AMS, particularly in the elderly, have shown positive rates of 24% in febrile patients and 18% in afebrile patients. Overall, the diagnostic landscape for AMS remains complex, demanding that emergency physicians skillfully integrate the four basic assessment tools with judicious selection of advanced diagnostic methods like imaging, blood biochemistry, CSF analysis, and EEG to accurately diagnose AMS. Further research and refinement of diagnostic protocols are essential to improve AMS assessment in emergency settings.
Etiology of AMS: Unveiling the Underlying Causes
Understanding the diverse pathogenic factors that manifest as Altered Mental Status (AMS), a condition denoted by the medical abbreviation AMS, is critical because it directly influences clinical treatment strategies. The varied clinical presentations of AMS necessitate accurate etiological diagnosis for effective patient management. Much of the existing emergency medicine literature on AMS concentrates on specific subgroups, such as patients in a comatose state, where coma itself may be considered a severe form of AMS. Generally, the causes of emergency AMS are broadly categorized into primary nervous system disorders and non-neurological factors. Recent studies suggest that neurological events are significant contributors to AMS, accounting for approximately 28% of cases.
Our research at xentrydiagnosis.store found that primary nervous system factors were responsible for 35% of AMS cases, rising to nearly 50% in elderly patients. While neurological events are a leading cause, the majority of acute AMS cases – over half – originate from non-nervous system factors. Specifically in the elderly demographic, the most prevalent causes of AMS were cerebrovascular disease, systemic and organic failures, and infections. Conversely, in younger patients, the leading causes were drugs and toxic substances, systemic and organic failures, and metabolic and endocrine disorders.
Non-neurological causes of AMS encountered in the emergency department are extensive, encompassing drug and substance intoxication, infections, metabolic and endocrine imbalances, trauma, cancer, and system or organ dysfunction. Among these, acute alcoholism is frequently cited as a major non-neurological contributor to AMS. In our study, drugs and toxic factors (including both alcoholic and non-alcoholic substances) accounted for 23% of AMS cases overall, and a striking 34.9% in the non-elderly group. System and organ dysfunction also emerged as a significant cause of acute AMS, with respiratory and cardiovascular system failures being particularly prominent, contributing to 9.8% of AMS cases. Organ failure in AMS patients is a serious and potentially life-threatening factor.
Trauma and infection are also critical factors in acute AMS etiology. Studies have reported trauma as the second most common cause of emergency AMS, responsible for up to 39% of AMS-related deaths, with head trauma being the primary concern. However, the specific etiology of AMS can vary geographically. Infection is considered the most common cause of non-traumatic AMS, with cerebral malaria being a leading cause in regions like Ethiopia and Zambia. Therefore, when diagnosing AMS, clinicians must consider a broad spectrum of potential causes, including less common conditions such as acute fatty liver of pregnancy, environment-related illnesses, and adrenal insufficiency. These conditions are critical to recognize due to their potential for causing fatal yet reversible damage if identified and treated promptly.
Emergency Treatment Strategies for AMS
Acute Altered Mental Status (AMS), often identified by the medical abbreviation AMS, is a potentially life-threatening condition demanding immediate attention. AMS should be integrated into the comprehensive management protocols within emergency departments and serve as a key criterion for hospital admission. The Emergency Severity Index (ESI) triage system, a widely used tool in EDs, typically categorizes acute AMS as level 1 (non-responsive, the highest risk) or level 2 (lethargic, mentally confused, disoriented), reflecting the severity of the condition. Despite this recognized severity, our study at xentrydiagnosis.store revealed that only 4.9% of AMS patients triaged at level 1 were admitted to the critical care unit. This is juxtaposed with the actual case fatality rate of AMS, which was found to be 8.1%, closely mirroring the mortality rate of 8.9% in the ED critical care unit during the same period. This discrepancy suggests a potential underestimation of the seriousness of AMS among emergency physicians. Upon the initial signs of acute AMS, particularly in elderly patients, immediate treatment, close monitoring, and rapid assessment are paramount. The algorithm depicted in Figure 2 provides a clinical intervention strategy tailored for AMS patients, based on identified causes, risk factors, and necessary interventions.
Figure 2.
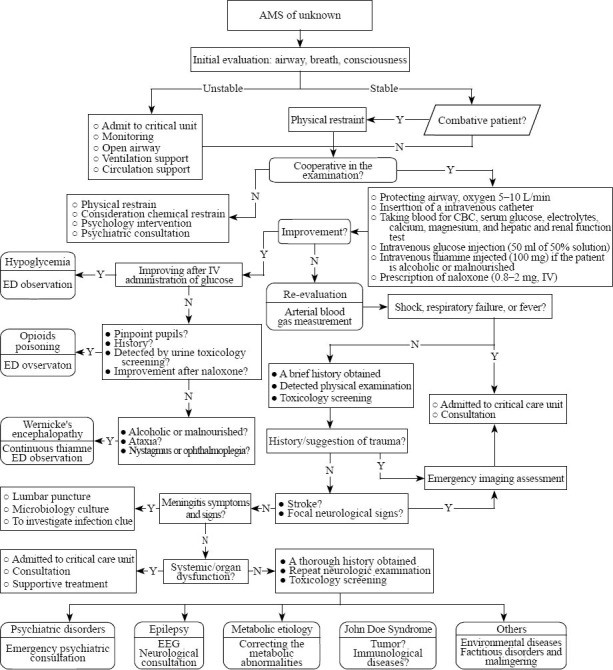 Algorithm for Diagnosing and Treating Altered Mental Status (AMS) in the Emergency Department
Algorithm for Diagnosing and Treating Altered Mental Status (AMS) in the Emergency Department
The etiology of AMS is often not immediately clear upon initial ED presentation. Conditions such as adrenal insufficiency, limbic encephalitis, and anti-NMDA receptor encephalitis, sometimes initially misdiagnosed as John Doe syndrome, can underlie AMS. These conditions are associated with high fatality and disability rates, yet are often responsive to rapid and effective treatments like glucocorticoids. Recent publications emphasize the critical need for clinicians to recognize anti-NMDA receptor encephalitis, especially when linked to ovarian teratomas, as timely teratoma removal can lead to patient recovery. However, delayed diagnosis can result in severe progression, including muscle weakness and respiratory failure, ultimately posing a life threat. Therefore, comprehensive emergency assessment and immediate, life-saving interventions remain crucial challenges for emergency physicians in managing AMS effectively.
Limitations of Current AMS Understanding and Research
Our analysis of Altered Mental Status (AMS), while insightful for understanding the diagnosis signified by the medical abbreviation AMS, is subject to certain limitations. Firstly, the inherent complexity of AMS clinical presentations can lead to a gap in understanding among emergency physicians. This complexity may result in missed AMS diagnoses, particularly in elderly patients who may also present with pre-existing chronic cognitive impairments. Secondly, our study was conducted at a single center, which may limit the generalizability of our findings to other emergency departments. The AMS patient demographics, diagnostic approaches, and treatment patterns observed in our setting may not fully reflect the broader spectrum of emergency care environments. Therefore, caution is advised when applying and interpreting our results in different clinical contexts. Thirdly, our data collection may not have comprehensively captured all risk factors contributing to mortality in AMS patients. Factors such as C-reactive protein levels and lactic acid levels, which are crucial indicators of acute illness severity, might have been under-evaluated due to an initial underestimation of the acute risk associated with AMS. Consequently, further research is necessary to more fully assess and understand the multifaceted risk factors for mortality in AMS patients.
In conclusion, a thorough examination of acute AMS patients reveals that the most common etiologies include primary neurological factors, drug and toxic exposures, system or organ dysfunction, and metabolic and endocrine imbalances. The underlying causes of AMS exhibit significant variations across different age groups, highlighting the need for age-sensitive diagnostic approaches. Considering the potentially reversible nature of many conditions causing AMS, coupled with the serious and potentially fatal outcomes associated with untreated AMS, timely assessment and rapid intervention targeting the likely causes and conditions are essential for improving patient outcomes in emergency settings.