Arthrogryposis Multiplex Congenita (AMC) is a condition characterized by multiple joint contractures present at birth, affecting at least two different areas of the body. Prenatal diagnosis of arthrogryposis is crucial for appropriate management and counseling. This article delves into the sonographic findings that are vital for Arthrogryposis Diagnosis In Utero, highlighting those indicators that carry significant prognostic value. By understanding these prenatal markers, healthcare professionals can better predict the course of the condition and provide enhanced support for expectant parents.
Understanding Arthrogryposis Multiplex Congenita (AMC)
Arthrogryposis Multiplex Congenita, often abbreviated as AMC, is not a single disease but rather a descriptive term for a range of conditions that result in congenital joint contractures. The term itself originates from Greek words: “arthron” (joint), “grypos” (curved), “multiplex” (multiple), “congenita” (congenital), and “-osis” (disease). AMC occurs in approximately 1 in 3,000 to 1 in 5,100 live births and signifies an underlying process that limits fetal movement, leading to joint stiffness. Over 300 to 400 distinct disease entities can cause AMC.
The underlying cause of AMC often involves reduced fetal movement over a period of three weeks or more during gestation. This reduced movement, regardless of the primary etiology, leads to joint stiffening and muscle atrophy. Moessinger introduced the concept of “fetal akinesia deformation sequence” (FADS) in 1983, demonstrating that restricted fetal movement in animal models resulted in similar anomalies seen in AMC, such as intrauterine growth restriction (IUGR), contractures, retrognathia, lung hypoplasia, and polyhydramnios. This underscores the critical role of normal fetal movement in typical intrauterine development.
Associated features, beyond joint contractures, can include craniofacial dysmorphia (retrognathia), lung hypoplasia, absent stomach filling (due to impaired swallowing), scoliosis, nuchal edema, hydrops fetalis, pterygia, polyhydramnios, and intrauterine growth restriction (IUGR). These additional findings can provide clues to the underlying cause and prognosis of AMC.
AMC is broadly classified into three types according to the Munich classification, modified by Hall:
- Type I: Primarily joint involvement, with amyoplasia being the most common cause.
- Type II: AMC accompanied by other system anomalies.
- Type III: Neuromuscular involvement, including severe or lethal forms and conditions associated with intellectual disability, such as FADS.
Prenatal ultrasound detection rates for AMC are reported to be around 25%, and the wide range of underlying causes contributes to varied outcomes, making counseling for parents complex. Therefore, identifying additional sonographic markers that indicate prognosis is vital for improving prenatal counseling and management.
The Role of Prenatal Ultrasound in Arthrogryposis Diagnosis
Prenatal ultrasound is the primary tool for arthrogryposis diagnosis in utero. While the detection rate is not exceptionally high, advancements in ultrasound technology and expertise allow for earlier and more accurate diagnoses. Suspicion of AMC often arises during routine prenatal screenings in the second or third trimester, or when investigating suspected fetal anomalies.
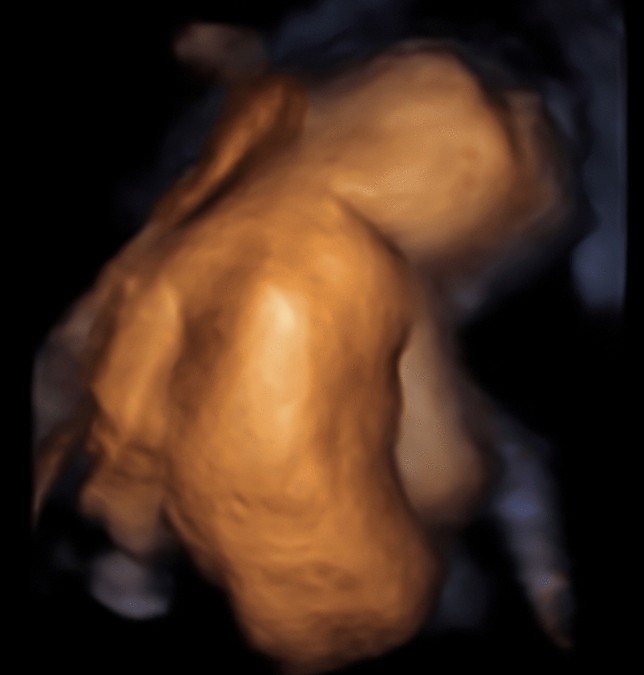
Fig. 1.
Sonographic image demonstrating scoliosis in a fetus at 26 weeks gestation, a significant finding in arthrogryposis diagnosis in utero.
The diagnosis of AMC via ultrasound relies on identifying joint fixations in at least two body areas and often includes observing fetal hypokinesia. Detailed fetal scans, supplemented by pulse-wave Doppler and 3D ultrasound, are crucial for comprehensive assessment. In some cases, invasive procedures like amniocentesis or chorionic villous sampling (CVS) may be performed for genetic testing to further elucidate the underlying cause.
Experienced Fetal Medicine Specialists play a critical role in evaluating fetal motor activity. A meticulous examination, sometimes lasting up to 45 minutes, is required to carefully observe fetal movements and assess for hypokinesia, a key indicator of potential arthrogryposis.
Study Methodology for Identifying Prognostic Sonographic Markers
A retrospective study was conducted involving 41 pregnancies with suspected AMC, diagnosed at a tertiary referral center between 1999 and 2017. The study aimed to identify additional sonographic abnormalities beyond joint contractures that are associated with unfavorable prognoses in fetuses with AMC types I-III.
The researchers reviewed prenatal sonograms, pediatric charts, genetic test results, and autopsy reports to confirm AMC diagnosis and analyze pregnancy outcomes. Cases were categorized into the three AMC types based on the Munich classification. Sonographic findings were categorized into typical joint contractures (flexion/extension) and additional malformations such as nuchal edema, hydrops, scoliosis, lung hypoplasia, absent gastric filling, and others.
The gestational age at first detection was also analyzed by dividing cases into groups based on detection before 20 weeks, between 20-24 weeks, and after 24 weeks of gestation. Statistical analysis was performed to determine the significance of sonographic findings in relation to pregnancy outcomes, including abortion, termination of pregnancy (TOP), live births, and neonatal death.
Key Sonographic Findings and Their Prognostic Significance
The study identified several sonographic findings beyond joint contractures that are significant predictors of prognosis in arthrogryposis diagnosis in utero.
Hydrops Fetalis and Nuchal Edema
Hydrops fetalis and nuchal edema emerged as strong indicators of unfavorable outcomes. Hydrops was present in 50% of fetuses who died postnatally and in 53% of cases resulting in termination of pregnancy, compared to 0% in surviving children. Similarly, nuchal edema was significantly more prevalent in cases with adverse outcomes.
Fig. 2.
Ultrasound image at 13 weeks gestation showing prefrontal edema and retrognathia (indicated by arrows), additional sonographic markers considered in arthrogryposis diagnosis in utero.
Absent Stomach Filling
Absent stomach filling, suggestive of impaired swallowing ability, was found in 67% of children who experienced neonatal death. This finding, while not always directly indicative of prognosis on its own, becomes more significant when considered alongside other markers.
Scoliosis
Scoliosis, a spinal deformity, was significantly associated with unfavorable outcomes and often indicated a neurological etiology. It was notably absent in surviving children in this study and present in a significant portion of antepartum deaths.
Fig. 3.
Sonographic depiction of scoliosis at 18 weeks gestation, highlighting its importance as a prognostic indicator in arthrogryposis diagnosis in utero.
Polyhydramnios
Polyhydramnios, or excessive amniotic fluid, was also significantly more common in pregnancies ending in prenatal death. While polyhydramnios can have various causes, its presence in the context of suspected AMC adds to the concern for a poorer prognosis.
AMC Type and Prognosis
Subcategorization into AMC types revealed crucial prognostic differences. Hydrops was observed in only 8% of the limb-involvement-only group (Type I), compared to 100% in the system anomaly group (Type II) and 70% in the neuromuscular dysfunction cohort (Type III). The absence of hydrops and nuchal edema was significantly associated with AMC Type I, as was less frequent absent stomach filling. Scoliosis and absent stomach filling were more indicative of a neurological etiology, commonly seen in AMC Type III.
Gestational Age at Detection
Findings detected earlier in gestation, particularly before 20 weeks, such as hydrops, scoliosis, and absent gastric filling, were more often associated with adverse outcomes. This suggests that early detection of these markers during arthrogryposis diagnosis in utero can provide critical prognostic information.
Discussion and Clinical Implications
This study underscores the importance of specific sonographic findings in predicting outcomes for fetuses diagnosed with AMC. The presence of hydrops, nuchal edema, scoliosis, and absent stomach filling are strong indicators of a less favorable prognosis, often pointing towards a neuromuscular etiology (AMC Type III or FADS). Conversely, the absence of these signs, especially in cases with isolated limb contractures (AMC Type I), suggests a more favorable outlook.
These findings align with existing literature that emphasizes the heterogeneous nature of AMC and the broad spectrum of underlying etiologies. While profile abnormalities were less frequent in this study compared to some reports, the consistent association of hydrops, nuchal edema, and scoliosis with poorer outcomes reinforces their clinical significance in arthrogryposis diagnosis in utero.
Fig. 4.
Another ultrasound image at 13 weeks gestation demonstrating prefrontal edema and retrognathia, reinforcing the importance of profile assessment during arthrogryposis diagnosis in utero.
The study’s limitations include its retrospective nature and the relatively small sample size. Additionally, the genetic testing methods evolved over the study period, potentially affecting the diagnostic yield for underlying genetic causes. Despite these limitations, the study provides valuable insights into the prognostic significance of sonographic markers in AMC.
Clinically, these findings are crucial for patient counseling. When arthrogryposis diagnosis in utero is made, the presence or absence of these prognostic sonographic markers should be carefully assessed and discussed with parents. Interdisciplinary counseling involving geneticists, pediatricians, obstetricians, and orthopedists is essential to provide comprehensive information about prognosis, potential underlying causes, and management options.
While a high termination rate was observed in this study, it is important to note that the decision for termination is complex and influenced by parental perspectives and counseling, not solely by prognosis. Continued data collection and research are essential to further refine prognostic indicators and improve counseling for families facing an arthrogryposis diagnosis in utero.
Conclusion: Enhancing Prenatal Counseling and Management
This study successfully identified key sonographic findings that carry prognostic significance in fetuses with suspected AMC. Hydrops, nuchal edema, scoliosis, and absent stomach filling are particularly associated with unfavorable outcomes, often indicating neuromuscular involvement. These findings are critical for refining arthrogryposis diagnosis in utero and enhancing prenatal counseling.
Understanding these prognostic markers allows healthcare providers to offer more informed and tailored counseling to expectant parents. While severe forms of AMC carry significant challenges, it is equally important to recognize that milder forms, often characterized by isolated limb contractures and the absence of adverse sonographic markers, have a good prognosis for survival and independent living. Early and accurate arthrogryposis diagnosis in utero, coupled with interdisciplinary care, is paramount to optimizing outcomes and supporting families affected by this condition.
References