Introduction
Arrhythmogenic right ventricular cardiomyopathy (ARVC), also known as arrhythmogenic right ventricular dysplasia, is a genetic myocardial disorder characterized by the progressive replacement of normal heart tissue with fibrofatty tissue, primarily in the right ventricle. However, it is increasingly recognized that ARVC can involve both ventricles or predominantly the left ventricle. This condition typically manifests in individuals during their second to fourth decades of life. Early and accurate Arvc Heart Diagnosis is paramount to guide patients in avoiding activities that can exacerbate the condition and to implement timely interventions. Common presenting symptoms include palpitations, syncope, ventricular tachycardia, and, in severe cases, sudden cardiac death.
This article delves into the essential aspects of ARVC heart diagnosis, encompassing diagnostic criteria, clinical presentations, key diagnostic modalities, and current therapeutic interventions. Clinicians will gain valuable insights into risk stratification for antiarrhythmic therapy and implantable cardioverter-defibrillator (ICD) placement. Notably, cardiac magnetic resonance imaging (CMR) has emerged as the gold standard imaging modality for ARVC heart diagnosis. Effective interprofessional communication strategies are also highlighted to ensure comprehensive patient care and optimize outcomes for individuals living with ARVC.
Objectives:
- Understand the complex pathophysiology of arrhythmogenic right ventricular cardiomyopathy using the most up-to-date knowledge.
- Recognize the diverse clinical presentations of arrhythmogenic right ventricular cardiomyopathy to facilitate accurate ARVC heart diagnosis.
- Apply evidence-based treatment management options for patients diagnosed with arrhythmogenic right ventricular cardiomyopathy.
- Foster effective collaboration with a multidisciplinary healthcare team to ensure coordinated and comprehensive care for patients with arrhythmogenic right ventricular cardiomyopathy.
Etiology of ARVC
ARVC is fundamentally a genetic disorder affecting the heart muscle. The condition stems from genetic mutations that disrupt the normal structure and function of cardiomyocytes, leading to progressive myocardial loss and fibrofatty replacement in one or both ventricles. Inheritance patterns are typically autosomal dominant with variable penetrance, meaning the disease can manifest differently even within the same family. Familial disease is a significant diagnostic criterion in ARVC heart diagnosis.
Genetic testing plays a crucial role in ARVC heart diagnosis, with approximately two-thirds of ARVC patients exhibiting positive genetic findings. To date, eight genes have been identified as primarily responsible for ARVC pathogenesis. These genes are broadly categorized into desmosomal genes (PKP2, DSP, DSG2, DSC2, and JUP) and non-desmosomal genes (TMEM43, DES, and PLN). Mutations in desmosomal genes are found in 50% to 60% of ARVC cases, with PKP2 being the most frequently mutated gene (20% to 46% of cases), followed by DSP and DSG2 (each accounting for approximately 10%). Patients presenting with left ventricular or biventricular involvement are more likely to harbor non-desmosomal gene mutations.
Naxos disease, an autosomal recessive condition caused by JUP mutations, highlights the diverse clinical spectrum of ARVC. This mutation disrupts plakoglobin, a protein crucial for cell adhesion within desmosomes, leading to both cardiac and dermatological manifestations, including palmoplantar keratosis and woolly hair. Carvajal syndrome, another autosomal recessive cardiomyopathy phenotypically similar to Naxos disease, typically presents earlier in childhood.
Epidemiology of ARVC
The estimated prevalence of ARVC in the general population ranges from 1 in 5000 to 1 in 2000, with higher rates reported in certain European regions like Italy and Germany. Men are slightly more frequently affected and tend to experience more severe disease, potentially due to hormonal influences or differences in exercise patterns. While ARVC is considered a relatively rare condition, it accounts for a significant proportion of sudden cardiac deaths in young individuals, underscoring the importance of timely ARVC heart diagnosis.
Pathophysiology of ARVC
ARVC pathogenesis primarily targets the intercalated discs, critical structures for cardiomyocyte interaction and cardiac function. These discs facilitate cell-to-cell communication and mechanical coupling. Damage to intercalated discs, often due to genetic mutations, leads to structural cardiomyocyte instability, particularly under mechanical stress. Proteins like plakoglobin and desmoplakin, essential components of desmosomes, provide structural support during mechanical stress. Intercalated discs also mediate electrical coupling through ion channels. Defects in sodium channels can reduce the action potential upstroke velocity. This combination of structural and electrical abnormalities leads to the hallmark features of ARVC: progressive cardiomyopathy and ventricular arrhythmias.
Pathologically, ARVC is characterized by myocyte loss in the right ventricle with fibrofatty replacement. This process typically begins in the subepicardium and midmyocardium, progressing to transmural fibrosis in advanced stages. Endurance sports and strenuous exercise have been implicated in promoting ARVC development and progression by increasing ventricular load and mechanical stress. While ARVC commonly presents in late adolescence or early adulthood, pediatric cases are increasingly recognized, emphasizing the importance of family history in ARVC heart diagnosis.
The 2020 revised diagnostic criteria for ARVC heart diagnosis acknowledge the significance of left-sided ventricular involvement and emphasize cardiac magnetic resonance imaging (CMR) as the preferred diagnostic modality. The criteria are categorized into six groups:
I. Structural alterations/function
II. Tissue characterization
III. Repolarization abnormalities
IV. Depolarization/conduction abnormalities
V. Arrhythmias
VI. Family history
Each category includes major and minor criteria. ARVC heart diagnosis is established based on fulfilling specific combinations of these criteria:
- Two major criteria
- One major plus two minor criteria
- Four minor criteria from different categories
Crucially, at least one criterion must be met from groups I or II, demonstrating structural or tissue abnormalities. The 2020 criteria also include specific criteria for diagnosing left ventricle phenotype ARVC, recognizing the challenges in differentiating it from other cardiomyopathies like dilated cardiomyopathy due to the non-specific nature of left ventricular dysfunction.
Table 1. 2020 International Criteria for Diagnosis of Arrhythmogenic Right Ventricular Cardiomyopathy.
Histopathology of ARVC
A major diagnostic criterion for ARVC heart diagnosis is fibrofatty replacement of the myocardium, predominantly affecting the subepicardial layer. Microscopic examination reveals desmosomal abnormalities and loss, confirmed by ultrastructural studies of endomyocardial biopsy (EMB) samples. Intercalated disc remodeling is also observed in EMB samples from ARVC patients.
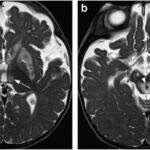
Skin biopsies in patients with DSP variants may show irregular desmoplakin and plakoglobin distribution in epidermal layers. However, cardiac magnetic resonance imaging (CMR) is increasingly replacing EMB in ARVC heart diagnosis. The 2020 criteria classify transmural late gadolinium enhancement or fibrosis on CMR, affecting at least one right ventricular region in two orthogonal views, as a major structural criterion, even with or without fatty tissue replacement. CMR tissue characterization demonstrates high concordance with EMB in identifying myocardial fibrosis, solidifying its role in ARVC heart diagnosis.
History and Physical Examination in ARVC
ARVC heart diagnosis is typically made between the ages of 20 and 40 years. Palpitations and syncope during exercise are common presenting symptoms. Studies indicate that common complaints include palpitations (30%-60%), lightheadedness (20%), and syncope (10%-30%), all linked to ventricular arrhythmias. Alarmingly, up to 60% of patients experiencing cardiac arrest may have had no prior symptoms, and sudden cardiac death can be the first manifestation of ARVC in up to 20% of diagnosed patients.
ARVC progression is often described in three stages:
- Concealed stage: Few overt structural abnormalities, often asymptomatic, but sudden cardiac arrest can still occur.
- Clinically overt stage: Detectable ventricular morphological abnormalities and presence of ventricular arrhythmias (premature ventricular complexes, non-sustained or sustained ventricular tachycardia, ventricular fibrillation). Atrial arrhythmias like atrial fibrillation are also more frequent. Hemodynamically stable ventricular tachycardia can be the initial presentation in up to 60% of patients.
- Right, left, or biventricular failure: Approximately half of ARVC patients progress to this stage, with exertional dyspnea being the most common heart failure symptom. Heart failure is a major indication for heart transplantation in ARVC and strongly associated with sudden cardiac death.
Another presentation can mimic myocarditis, with chest pain and elevated cardiac enzymes but no coronary artery disease. This is more common in certain genetic variants and in children with ARVC. Pediatric myocarditis, especially with a positive family history, should prompt consideration of ARVC heart diagnosis.
Patients with Naxos disease (JUP mutation) may exhibit woolly hair and alopecia. Alopecia is also seen in DSP variant carriers. Desmoplakin mutations can also manifest with woolly hair and keratotic skin lesions. Other cutaneous findings include eczema, fragile skin, ulcers, and pemphigus-like lesions. Dental and nail abnormalities have also been reported. Severe neonatal epidermolysis has been reported in homozygous JUP and DSP mutation carriers. Recognizing these extra-cardiac signs can aid in ARVC heart diagnosis, particularly in syndromic forms of the disease.
Evaluation for ARVC Heart Diagnosis
A comprehensive evaluation is crucial for accurate ARVC heart diagnosis, incorporating various diagnostic modalities:
Electrocardiogram (ECG): ECG is rarely normal in ARVC. T-wave inversions in right precordial leads (V1-V4) are common, and extension to V5-V6 may suggest left-sided involvement. Incomplete right bundle branch block is seen in about 15% of patients. Ventricular tachycardia with a left bundle branch block pattern is a significant arrhythmia in ARVC. Epsilon waves, due to delayed right ventricular activation, are present in around 50% of cases but downgraded to a minor criterion in the 2020 criteria.
Holter Monitoring: Long-term ECG monitoring (24 hours or more) is essential for detecting intermittent ventricular arrhythmias, especially in symptomatic patients, aiding in ARVC heart diagnosis.
Echocardiography: Echocardiography may reveal right ventricular enlargement, hypokinesia, or a thin right ventricular free wall. Systolic akinesia, dyskinesia, or diastolic bulging may also be present. Left ventricular and septal involvement can occur. End-stage disease can lead to right ventricular or biventricular pump failure. Wall motion abnormalities should be confirmed in two orthogonal planes. Serial echocardiograms (every 1-3 years) are recommended for monitoring disease progression.
Cardiac Magnetic Resonance (CMR): CMR is the preferred imaging modality for ARVC heart diagnosis. It can visualize fatty infiltration (diffuse brightness on T1), right ventricular volumes, systolic function, and regional wall motion abnormalities. CMR provides superior visualization of the right ventricle compared to other imaging techniques. In patients with contraindications to CMR, CT scans can offer some similar measurements but with lower resolution.
Electrophysiologic Studies (EPS): EPS are rarely indicated for routine ARVC heart diagnosis. They may be used to differentiate ARVC from idiopathic right ventricular outflow tract tachycardia, a benign condition.
Endomyocardial Biopsy (EMB): Transvenous right ventricular biopsy can be highly specific for ARVC but has a high false-negative rate due to patchy disease distribution, requiring sampling of affected myocardium. EMB is not routinely required if ARVC criteria are met by other modalities.
Cardiac Catheterization: Cardiac catheterization is rarely performed in ARVC heart diagnosis, primarily used to rule out congenital heart disease with left-to-right shunts. It may be performed prior to EMB in some cases.
Treatment and Management of ARVC
The primary goals of ARVC management are to reduce the risk of sudden cardiac death, slow disease progression, and improve quality of life by minimizing arrhythmia burden and heart failure symptoms. Management strategies encompass clinical measures, pharmacological therapy, catheter ablation, ICD implantation, and, in select cases, cardiac transplantation.
-
Clinical Management: Restriction of physical activity is paramount as exercise can exacerbate arrhythmias and accelerate disease progression. This recommendation applies even to gene-positive, phenotype-negative individuals. Limiting exercise to less than 650 MET hours per year (approximately 30 minutes of brisk walking daily) is advised to potentially delay symptom onset in phenotype-negative individuals and reduce risk in diagnosed patients.
-
Pharmacological Treatment: Medications aim to suppress arrhythmias, prevent thrombus formation, and manage heart failure symptoms.
- Beta-blockers: Cardioselective, long-acting beta-blockers like metoprolol are recommended for all clinically affected ARVC patients to reduce arrhythmias and ventricular wall stress.
- Sotalol: A non-selective beta-blocker with class III antiarrhythmic properties, sotalol is considered the most effective antiarrhythmic agent in ARVC.
- Amiodarone and Flecainide: Amiodarone (class III) or adjunctive flecainide (class Ic) may be used for persistent ventricular arrhythmias despite sotalol. Flecainide is generally avoided in patients with reduced left ventricular ejection fraction.
- Heart Failure Medications: Standard heart failure therapies (ACE inhibitors, angiotensin receptor blockers, beta-blockers, diuretics) are used for right or left heart failure management in ARVC.
- Anticoagulants: Anticoagulation is reserved for patients with atrial fibrillation or thromboembolic complications.
-
Radiofrequency Catheter Ablation: Catheter ablation is an option for patients with refractory or incessant ventricular tachycardia despite medical therapy. It is recommended for recurrent ventricular tachycardia or ICD discharges. A combined endocardial/epicardial approach may be necessary if endocardial ablation fails. Recurrence rates of ventricular tachycardia post-ablation can be high (50%-75% over 3 years) due to disease progression.
-
Implantable Cardioverter-Defibrillator (ICD): ICD implantation is the most effective measure for preventing sudden cardiac death in high-risk ARVC patients. Single-chamber ICDs are preferred, with anti-tachycardia pacing programmed. ICD implantation is recommended in various scenarios:
- Cardiac arrest due to ventricular tachycardia or fibrillation.
- Symptomatic ventricular tachycardia refractory to medications.
- Inducible ventricular tachycardia on EPS.
- Severe right or left ventricular dysfunction with ventricular tachycardia intolerance.
- Non-sustained ventricular tachycardia with suspected arrhythmic syncope.
- Family history of sudden cardiac death in a first-degree relative.
ICD therapy provides a significant survival benefit (estimated 26%) but carries risks like lead infections and inappropriate shocks. Prophylactic ICD implantation is generally not recommended for healthy gene carriers or asymptomatic patients without risk factors.
- Cardiac Transplantation: Cardiac transplantation is reserved for patients with intractable arrhythmias or end-stage ventricular failure unresponsive to medical management. Post-transplant survival rates are comparable to non-ARVC transplant recipients and better than those transplanted for ischemic cardiomyopathy.
Differential Diagnosis of ARVC
ARVC heart diagnosis requires careful differentiation from other conditions with similar presentations. Key differential diagnoses include:
Right Ventricular Outflow Tract Tachycardia (RVOT-VT): RVOT-VT can mimic ARVC clinically, and the RVOT is a common arrhythmia origin site in ARVC. However, RVOT-VT is not inherited, lacks genetic mutations, and typically presents with monomorphic, non-sustained VT, whereas ARVC VT is often polymorphic. RVOT-VT is less likely to have precordial T-wave inversions. Imaging is crucial to distinguish ARVC by demonstrating fibrofatty infiltration, absent in RVOT-VT.
Brugada Syndrome: Brugada syndrome, like ARVC, is inherited and associated with SCN5A gene mutations. ECG in Brugada syndrome shows right precordial ST elevations and T-wave inversions, with dynamic ECG patterns. ARVC ECG patterns are typically more stable. Cardiac imaging in Brugada syndrome is normal, unlike ARVC. Brugada syndrome is more prevalent in Southeast Asia, while ARVC is more common in Europe.
Cardiac Sarcoidosis: Cardiac sarcoidosis can be mistaken for ARVC on imaging. Features favoring sarcoidosis include mediastinal lymphadenopathy, older age, non-familial pattern, delayed gadolinium enhancement in the ventricular septum on CMR, intense myocardial FDG uptake on PET, and AV block. Endomyocardial biopsy may be needed for definitive differentiation in some cases.
Congenital heart diseases like Ebstein anomaly, left-to-right shunts, and Uhl anomaly can also mimic ARVC symptoms. Cardiac imaging is usually diagnostic.
Left-dominant ARVC shares imaging similarities with dilated cardiomyopathy, muscular dystrophies, myocarditis, cardiac sarcoidosis, congenital ventricular aneurysms, and Chagas heart disease. Subepicardial to transmural progression of fibrofatty infiltration is a key differentiating feature of ARVC.
Prognosis of ARVC
The mortality rate in ARVC ranges from 0.08% to 3.6% per year, but is less than 1% with treatment. Prognosis is largely determined by arrhythmia severity and ventricular dysfunction extent. Prior syncope from sustained ventricular tachycardia or cardiac arrest from ventricular fibrillation is the strongest predictor of recurrent life-threatening arrhythmias. Other risk factors include sustained or non-sustained ventricular tachycardia and reduced cardiac function.
Major risk factors for sudden cardiac death or life-threatening arrhythmia:
- Prior cardiac arrest due to ventricular arrhythmia.
- Unexplained syncope history.
- Non-sustained ventricular tachycardia during exercise stress test or Holter monitoring.
- Severe systolic dysfunction of right, left, or both ventricles.
Minor risk factors include frequent premature ventricular contractions (>1000/day), T-wave inversions in >3 ECG leads, known genetic mutations, younger age at presentation, and male sex. Risk stratification is essential in guiding management and ARVC heart diagnosis follow-up.
Complications of ARVC
Complications can arise from untreated ARVC, diagnostic procedures, and treatments. Untreated ARVC can lead to ventricular tachycardia, ventricular fibrillation, heart failure, sudden death, and thromboembolism. Genotype can influence complication risk; for example, PKP2 variants are associated with right ventricular involvement, while DSG2 variants may increase heart failure and transplant risk.
ICD therapy carries risks of inappropriate shocks and lead complications. Antiarrhythmic drugs can cause QT prolongation, and anticoagulation can lead to bleeding. EMB, while diagnostically valuable in specific cases, carries risks of cardiac perforation or valve/chordal damage. The 2020 criteria emphasize selective EMB use to minimize these risks in ARVC heart diagnosis.
Deterrence and Patient Education for ARVC
Accurate ARVC heart diagnosis is crucial due to the risk of sudden cardiac death. Risk stratification guides management. Asymptomatic ARVC patients should restrict exercise and undergo regular (1-2 year) re-evaluation. Patient education is vital regarding risks, prognosis, therapeutic options, and shared decision-making. Family member screening is essential. Educating patients about the risks of sudden cardiac death, antiarrhythmics, and ICDs (like inappropriate shocks) is critical for informed consent and adherence to management plans in ARVC heart diagnosis.
Enhancing Healthcare Team Outcomes in ARVC
Optimal care for ARVC patients requires a collaborative interprofessional team including physicians, nurses, pharmacists, radiology, and ECG technicians. Expertise in ARVC heart diagnosis, evaluation, and treatment is paramount, including ECG and CMR interpretation, complication recognition, and differential diagnosis. Evidence-based guidelines and individualized care plans are essential.
Ethical considerations arise in treatment decisions and respecting patient autonomy, particularly with ICDs and their potential complications. Open communication, shared decision-making, family screening, and regular follow-up are crucial. Effective interprofessional communication and care coordination minimize errors, delays, and enhance patient safety, ultimately improving outcomes and patient-centered care for those with ARVC.
Review Questions
(Note: Review questions are present in the original article but are not included in this rewritten version as per instructions.)
References
(References are maintained as in the original article.)
1.Corrado D, Zorzi A, Cipriani A, Bauce B, Bariani R, Beffagna G, De Lazzari M, Migliore F, Pilichou K, Rampazzo A, Rigato I, Rizzo S, Thiene G, Perazzolo Marra M, Basso C. Evolving Diagnostic Criteria for Arrhythmogenic Cardiomyopathy. J Am Heart Assoc. 2021 Sep 21;10(18):e021987. [PMC free article: PMC8649536] [PubMed: 34533054]
2.Ohno S. The genetic background of arrhythmogenic right ventricular cardiomyopathy. J Arrhythm. 2016 Oct;32(5):398-403. [PMC free article: PMC5063271] [PubMed: 27761164]
3.Te Riele ASJM, James CA, Calkins H, Tsatsopoulou A. Arrhythmogenic Right Ventricular Cardiomyopathy in Pediatric Patients: An Important but Underrecognized Clinical Entity. Front Pediatr. 2021;9:750916. [PMC free article: PMC8678603] [PubMed: 34926342]
4.Krahn AD, Wilde AAM, Calkins H, La Gerche A, Cadrin-Tourigny J, Roberts JD, Han HC. Arrhythmogenic Right Ventricular Cardiomyopathy. JACC Clin Electrophysiol. 2022 Apr;8(4):533-553. [PubMed: 35450611]
5.Li GL, Saguner AM, Fontaine GH. Naxos disease: from the origin to today. Orphanet J Rare Dis. 2018 May 10;13(1):74. [PMC free article: PMC5946438] [PubMed: 29747658]
6.Sun Q, Wine Lee L, Hall EK, Choate KA, Elder RW. Hair and skin predict cardiomyopathies: Carvajal and erythrokeratodermia cardiomyopathy syndromes. Pediatr Dermatol. 2021 Jan;38(1):31-38. [PubMed: 33275305]
7.Corrado D, Link MS, Calkins H. Arrhythmogenic Right Ventricular Cardiomyopathy. N Engl J Med. 2017 Jan 05;376(1):61-72. [PubMed: 28052233]
8.Cerrone M, Noorman M, Lin X, Chkourko H, Liang FX, van der Nagel R, Hund T, Birchmeier W, Mohler P, van Veen TA, van Rijen HV, Delmar M. Sodium current deficit and arrhythmogenesis in a murine model of plakophilin-2 haploinsufficiency. Cardiovasc Res. 2012 Sep 01;95(4):460-8. [PMC free article: PMC3422082] [PubMed: 22764151]
9.Corrado D, Wichter T, Link MS, Hauer RN, Marchlinski FE, Anastasakis A, Bauce B, Basso C, Brunckhorst C, Tsatsopoulou A, Tandri H, Paul M, Schmied C, Pelliccia A, Duru F, Protonotarios N, Estes NM, McKenna WJ, Thiene G, Marcus FI, Calkins H. Treatment of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia: An International Task Force Consensus Statement. Circulation. 2015 Aug 04;132(5):441-53. [PMC free article: PMC4521905] [PubMed: 26216213]
10.Pigors M, Schwieger-Briel A, Cosgarea R, Diaconeasa A, Bruckner-Tuderman L, Fleck T, Has C. Desmoplakin mutations with palmoplantar keratoderma, woolly hair and cardiomyopathy. Acta Derm Venereol. 2015 Mar;95(3):337-40. [PubMed: 25227139]
11.Wang W, James CA, Calkins H. Diagnostic and therapeutic strategies for arrhythmogenic right ventricular dysplasia/cardiomyopathy patient. Europace. 2019 Jan 01;21(1):9-21. [PMC free article: PMC6321962] [PubMed: 29688316]
12.Tedford RJ, James C, Judge DP, Tichnell C, Murray B, Bhonsale A, Philips B, Abraham T, Dalal D, Halushka MK, Tandri H, Calkins H, Russell SD. Cardiac transplantation in arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Am Coll Cardiol. 2012 Jan 17;59(3):289-90. [PMC free article: PMC3258430] [PubMed: 22240135]
13.Corrado D, Basso C, Thiene G. Arrhythmogenic right ventricular cardiomyopathy: diagnosis, prognosis, and treatment. Heart. 2000 May;83(5):588-95. [PMC free article: PMC1760807] [PubMed: 10768917]
14.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MG, Daubert JP, Fontaine G, Gear K, Hauer R, Nava A, Picard MH, Protonotarios N, Saffitz JE, Sanborn DM, Steinberg JS, Tandri H, Thiene G, Towbin JA, Tsatsopoulou A, Wichter T, Zareba W. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010 Apr;31(7):806-14. [PMC free article: PMC2848326] [PubMed: 20172912]
15.Jain R, Dalal D, Daly A, Tichnell C, James C, Evenson A, Jain R, Abraham T, Tan BY, Tandri H, Russell SD, Judge D, Calkins H. Electrocardiographic features of arrhythmogenic right ventricular dysplasia. Circulation. 2009 Aug 11;120(6):477-87. [PMC free article: PMC2814546] [PubMed: 19635971]
16.Gemayel C, Pelliccia A, Thompson PD. Arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2001 Dec;38(7):1773-81. [PubMed: 11738273]
17.Haugaa KH, Basso C, Badano LP, Bucciarelli-Ducci C, Cardim N, Gaemperli O, Galderisi M, Habib G, Knuuti J, Lancellotti P, McKenna W, Neglia D, Popescu BA, Edvardsen T., EACVI Scientific Documents Committee, EACVI Board members and external reviewers. EACVI Scientific Documents Committee, EACVI Board members and external reviewers. Comprehensive multi-modality imaging approach in arrhythmogenic cardiomyopathy-an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2017 Mar 01;18(3):237-253. [PMC free article: PMC5837226] [PubMed: 28069601]
18.Corrado D, van Tintelen PJ, McKenna WJ, Hauer RNW, Anastastakis A, Asimaki A, Basso C, Bauce B, Brunckhorst C, Bucciarelli-Ducci C, Duru F, Elliott P, Hamilton RM, Haugaa KH, James CA, Judge D, Link MS, Marchlinski FE, Mazzanti A, Mestroni L, Pantazis A, Pelliccia A, Marra MP, Pilichou K, Platonov PGA, Protonotarios A, Rampazzo A, Saffitz JE, Saguner AM, Schmied C, Sharma S, Tandri H, Te Riele ASJM, Thiene G, Tsatsopoulou A, Zareba W, Zorzi A, Wichter T, Marcus FI, Calkins H., International Experts. Arrhythmogenic right ventricular cardiomyopathy: evaluation of the current diagnostic criteria and differential diagnosis. Eur Heart J. 2020 Apr 07;41(14):1414-1429. [PMC free article: PMC7138528] [PubMed: 31637441]
19.Cannavale G, Francone M, Galea N, Vullo F, Molisso A, Carbone I, Catalano C. Fatty Images of the Heart: Spectrum of Normal and Pathological Findings by Computed Tomography and Cardiac Magnetic Resonance Imaging. Biomed Res Int. 2018;2018:5610347. [PMC free article: PMC5818975] [PubMed: 29503824]
20.Zorzi A, Cipriani A, Bariani R, Pilichou K, Corrado D, Bauce B. Role of Exercise as a Modulating Factor in Arrhythmogenic Cardiomyopathy. Curr Cardiol Rep. 2021 May 07;23(6):57. [PMC free article: PMC8105216] [PubMed: 33961139]
21.Thiene G, Corrado D, Basso C. Arrhythmogenic right ventricular cardiomyopathy/dysplasia. Orphanet J Rare Dis. 2007 Nov 14;2:45. [PMC free article: PMC2222049] [PubMed: 18001465]
22.Fontaine G, Tonet J, Gallais Y, Lascault G, Hidden-Lucet F, Aouate P, Halimi F, Poulain F, Johnson N, Charfeddine H, Frank R. Ventricular tachycardia catheter ablation in arrhythmogenic right ventricular dysplasia: a 16-year experience. Curr Cardiol Rep. 2000 Nov;2(6):498-506. [PubMed: 11203287]
23.Gaine SP, Calkins H. Antiarrhythmic Drug Therapy in Arrhythmogenic Right Ventricular Cardiomyopathy. Biomedicines. 2023 Apr 19;11(4) [PMC free article: PMC10136163] [PubMed: 37189831]
24.Corrado D, Leoni L, Link MS, Della Bella P, Gaita F, Curnis A, Salerno JU, Igidbashian D, Raviele A, Disertori M, Zanotto G, Verlato R, Vergara G, Delise P, Turrini P, Basso C, Naccarella F, Maddalena F, Estes NA, Buja G, Thiene G. Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2003 Dec 23;108(25):3084-91. [PubMed: 14638546]
25.Corrado D, Basso C. Arrhythmogenic left ventricular cardiomyopathy. Heart. 2022 May;108(9):733-743. [PMC free article: PMC8995901] [PubMed: 34257076]
26.Brugada R, Campuzano O, Sarquella-Brugada G, Brugada J, Brugada P. Brugada syndrome. Methodist Debakey Cardiovasc J. 2014 Jan-Mar;10(1):25-8. [PMC free article: PMC4051330] [PubMed: 24932359]
27.Wallace R, Calkins H. Risk Stratification in Arrhythmogenic Right Ventricular Cardiomyopathy. Arrhythm Electrophysiol Rev. 2021 Apr;10(1):26-32. [PMC free article: PMC8076971] [PubMed: 33936740]
28.Zhu X, Wang Z, Ferrari MW, Ferrari-Kuehne K, Bulter J, Xu X, Zhou Q, Zhang Y, Zhang J. Anticoagulation in cardiomyopathy: unravelling the hidden threat and challenging the threat individually. ESC Heart Fail. 2021 Dec;8(6):4737-4750. [PMC free article: PMC8712898] [PubMed: 34498416]
29.Hodes AR, Tichnell C, Te Riele AS, Murray B, Groeneweg JA, Sawant AC, Russell SD, van Spaendonck-Zwarts KY, van den Berg MP, Wilde AA, Tandri H, Judge DP, Hauer RN, Calkins H, van Tintelen JP, James CA. Pregnancy course and outcomes in women with arrhythmogenic right ventricular cardiomyopathy. Heart. 2016 Feb 15;102(4):303-12. [PMC free article: PMC4752646] [PubMed: 26719359]
Disclosures:
Sandy Shah, Krishna Kishore Umapathi, Preeti Rout, Maria Horenstein, and Tony Oliver declare no relevant financial relationships with ineligible companies.