Introduction
Aspergillosis, primarily caused by Aspergillus fumigatus, is the most prevalent mold infection affecting the lungs. This infection presents a wide array of clinical manifestations, influenced significantly by the host’s immune status. These manifestations range from allergic bronchopulmonary aspergillosis (ABPA) in individuals with asthma or cystic fibrosis [1], to chronic pulmonary aspergillosis (CPA) in those with pre-existing lung conditions and mild immunocompromise [2]. CPA itself encompasses several forms, from simple aspergilloma to chronic cavitary, fibrosing, and microinvasive aspergillosis [2]. Subacute invasive aspergillosis, or chronic necrotizing aspergillosis, represents a progressive form in mildly immunocompromised patients [2], while acute invasive pulmonary aspergillosis (IPA) is a severe infection seen in significantly immunocompromised individuals, including those with hematologic malignancies, neutropenia post-chemotherapy, or recipients of organ or stem cell transplants [3]. Notably, IPA has also emerged as a complication in critically ill, apparently immunocompetent patients in the intensive care unit (ICU), particularly those with severe influenza or coronavirus disease 2019 (COVID-19) [4–6].
While Aspergillus fumigatus is the most common culprit, Aspergillus flavus, Aspergillus terreus, and Aspergillus niger also contribute to pulmonary aspergillosis, with regional variations in prevalence [7, 8]. Less frequent causative species include Aspergillus nidulans, Aspergillus calidoustus, and certain cryptic species like Aspergillus lentulus.
Diagnosing pulmonary aspergillosis is a significant challenge due to the limited sensitivity and specificity of available diagnostic tools. This complexity often leads to delays in diagnosis and treatment. Furthermore, the management of this condition is complicated by limited treatment options, potential drug interactions, adverse effects of antifungal medications, and the growing concern of antifungal resistance. This review aims to provide a comprehensive overview of the current diagnostic criteria and therapeutic strategies for IPA and CPA, highlighting recent advancements and future directions in patient management. Allergic aspergillosis, specifically ABPA, will not be covered in this discussion.
Diagnosis of Pulmonary Aspergillosis: Establishing the Criteria
Invasive Pulmonary Aspergillosis (IPA) Diagnosis Criteria
Diagnosing IPA presents a considerable clinical challenge due to the often subtle and nonspecific initial symptoms, coupled with the limitations of radiological and mycological tests. Therefore, the diagnosis of IPA relies on a graded approach, categorizing the likelihood of infection as possible, probable, or proven. The European Organization for Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium (EORTC-MSGERC) criteria are the gold standard for defining IPA in immunocompromised patients [9]. These criteria integrate host factors, clinical manifestations, and mycological evidence to establish a diagnostic probability (figure 1) [9].
Diagnostic Categories Based on EORTC-MSGERC Criteria
- Possible IPA: Requires the presence of at least one host criterion and one clinical criterion. This category indicates a suspicion of IPA but lacks definitive mycological confirmation.
- Probable IPA: Necessitates meeting at least one host criterion, one clinical criterion, and one mycological criterion. This category suggests a higher likelihood of IPA due to supporting mycological evidence.
- Proven IPA: Defined independently of host, clinical, and mycological criteria, and typically requires histopathological evidence of Aspergillus invasion in tissue samples.
Host Criteria for IPA Diagnosis
Host criteria identify conditions that predispose individuals to IPA. These include:
- Hematopoietic stem cell transplant (HSCT) recipients: Particularly allogeneic HSCT recipients with graft-versus-host disease (GVHD).
- Hematologic malignancy: Especially acute leukemia and lymphoma.
- Neutropenia: Prolonged chemotherapy-induced neutropenia (absolute neutrophil count < 500 cells/µL for >10 days).
- Solid organ transplant (SOT) recipients: Especially lung transplant recipients.
- Corticosteroid use: High-dose or prolonged corticosteroid therapy (e.g., prednisone ≥ 0.3 mg/kg/day for >3 weeks).
- Other immunosuppressive medications: Including TNF-alpha inhibitors, Bruton tyrosine kinase inhibitors, and other agents causing significant immunosuppression.
- Inherited immunodeficiency: Severe combined immunodeficiency, chronic granulomatous disease, etc.
Clinical Criteria for IPA Diagnosis
Clinical criteria encompass signs and symptoms suggestive of IPA, combined with radiological findings.
- Lower respiratory tract symptoms: Cough, dyspnea, pleuritic chest pain, hemoptysis. These symptoms are often nonspecific but should raise suspicion in at-risk patients.
- Fever: Persistent or recurrent fever despite broad-spectrum antibiotic therapy, particularly in neutropenic patients.
- Radiological findings on Chest CT:
- Nodules or masses: Well-circumscribed dense lesions, often with a halo sign.
- Halo sign: Ground-glass opacity surrounding a nodule, representing hemorrhage in early IPA.
- Air crescent sign: Partial cavitation within a nodule, indicating a later stage of IPA and necrosis.
- Cavity: Established cavitation within a lesion, a late manifestation associated with poorer prognosis.
- Pleural effusion or empyema: Less common but can occur in IPA.
Chest computed tomography (CT) is crucial in the diagnostic process for suspected IPA, especially in immunocompromised individuals [10]. Standard chest radiography is less sensitive and not recommended for initial screening [10].
Mycological Criteria for IPA Diagnosis
Mycological criteria provide laboratory evidence of Aspergillus infection. These tests can be broadly categorized into direct and indirect methods.
-
Direct Mycological Evidence:
- Histopathology: Microscopic examination of tissue biopsies (lung, pleural fluid) showing hyphae characteristic of Aspergillus with evidence of tissue invasion. This is the gold standard for proven IPA.
- Culture: Isolation of Aspergillus species from respiratory samples (sputum, bronchoalveolar lavage (BAL) fluid, pleural fluid, tissue). While culture is specific, it has limited sensitivity, particularly in early IPA.
-
Indirect Mycological Evidence (Biomarkers and Molecular Tests):
- Galactomannan (GM) Assay: Detects galactomannan, a polysaccharide component of the Aspergillus cell wall, in serum and BAL fluid.
- Serum GM: Widely used screening test, but sensitivity varies depending on patient population and antifungal prophylaxis. Specificity can be affected by certain medications and conditions.
- BAL Fluid GM: Higher sensitivity and specificity compared to serum GM, especially in patients with localized pulmonary disease.
- (1→3)-β-d-Glucan (BDG) Assay: Detects BDG, a component of the cell wall of many fungi, including Aspergillus. Less specific for Aspergillus than GM, as it can be positive in other fungal infections. Primarily used in serum.
- Aspergillus PCR: Detects Aspergillus DNA in respiratory samples, serum, and other body fluids.
- BAL Fluid PCR: High sensitivity and specificity for IPA diagnosis.
- Serum PCR: Becoming increasingly used, but standardization and interpretation of results are still evolving.
- Commercial Kits: Several commercially available kits offer rapid and standardized Aspergillus PCR detection, some including detection of azole resistance mutations (table 1).
- Galactomannan (GM) Assay: Detects galactomannan, a polysaccharide component of the Aspergillus cell wall, in serum and BAL fluid.
figure 1 visually summarizes the EORTC-MSGERC diagnostic classification for IPA.
FIGURE 1. Diagnostic Classification of Invasive Pulmonary Aspergillosis (IPA) According to EORTC-MSGERC Criteria
Schematic representation of the diagnostic classification of invasive pulmonary aspergillosis (IPA) based on the European Organization for Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium criteria. Diagnosis categories are based on host, clinical, and mycological factors. Possible IPA: one host + one clinical criterion. Probable IPA: one host + one clinical + one mycological criterion. Proven IPA: Histopathological evidence of invasion. BAL: bronchoalveolar lavage; CT: computed tomography; PCR: specific polymerase chain reaction for Aspergillus species.
table 1 provides a detailed overview of nonculture commercial diagnostic tests for IPA.
TABLE 1. Characteristics of Nonculture Commercial Diagnostic Tests for Invasive Pulmonary Aspergillosis
Summary of key nonculture diagnostic tests for IPA, including target antigen or DNA, test type, manufacturer, detection spectrum, sample type, and cut-off values. Includes Galactomannan assays (Platelia, Soña, VirClia), (1→3)-β-d-Glucan assays (Fungitell, Fungitell STAT, Wako, Dynamiker), and Aspergillus DNA PCR assays (MycAssay Aspergillus, AsperGenius, MycoGenie, Fungiplex Aspergillus azole-R). BAL: bronchoalveolar lavage; EIA: enzyme immunoassay; LFA: lateral flow assay; NA: not applicable; ODI: optical density index.
Diagnostic Approaches in Specific Patient Populations
The clinical presentation, diagnostic approach, and performance of diagnostic tests for IPA can vary significantly across different patient populations. Therefore, it is essential to tailor diagnostic strategies based on the underlying risk factors and clinical context.
IPA Diagnosis in Hematologic Cancer Patients
Patients with hematologic malignancies, particularly those undergoing intensive chemotherapy or allogeneic HSCT, are at the highest risk for IPA [14–18]. The incidence ranges from 2–8% in these high-risk groups. However, IPA is increasingly diagnosed in other hematologic cancer populations previously considered at lower risk, such as those with lymphoma, multiple myeloma, or chronic leukemia [8, 19–21]. Novel anticancer therapies like Bruton tyrosine kinase inhibitors have also been linked to increased IPA risk [22].
Radiological Findings: Neutropenic hematologic cancer patients often present with characteristic chest CT findings:
- Halo Sign: Frequently observed in early IPA, representing nodules surrounded by ground-glass opacity.
- Nodules and Masses: Well-defined, dense pulmonary lesions.
- Air Crescent Sign and Cavitation: Later stage findings indicating necrosis and poorer prognosis [10, 23].
Mycological Tests: Direct examination and cultures from respiratory samples have low yield in hematologic cancer patients (around 20% and 50% sensitivity, respectively) [24–26]. Nonculture methods, particularly serum or BAL GM and PCR, are crucial for IPA diagnosis, often being the sole mycological markers in over 50% of cases [8, 12, 25, 27]. table 2 summarizes the performance of GM and PCR in serum and BAL. Combined use of serum or BAL GM and PCR yields the highest sensitivity and specificity [28–30]. BDG testing in serum is less specific in this population due to false-positive results, especially in patients receiving intravenous immunoglobulins [11, 31, 32].
TABLE 2. Performance of Galactomannan (GM) and Aspergillus PCR in Serum and Bronchoalveolar Lavage Fluid (BAL) for IPA Diagnosis in Hematologic Cancer Patients
Meta-analysis data showing sensitivity and specificity of serum and BAL GM and Aspergillus PCR for diagnosing proven and probable IPA in hematologic cancer patients. Includes data from Pfeiffer et al., Leeflang et al., Arvanitis et al., Mengoli et al., Guo et al., Avni et al., Zou et al., Heng et al., and De Heer et al. Highlights the improved performance of combined GM and PCR testing. CI: Confidence Interval.
Diagnostic Algorithm: Due to the increasing use of posaconazole prophylaxis in high-risk patients [33, 34], routine serial serum GM screening is not universally recommended due to low positive predictive value in this context [34, 35]. However, a pre-emptive approach using serial serum GM screening (e.g., twice weekly) can be an alternative to systemic antifungal prophylaxis [34]. Chest CT is essential for persistent or recurrent febrile neutropenia or positive serum GM. Bronchoscopy with BAL should be considered if a lung lesion consistent with IPA is seen on CT, as BAL samples provide the highest sensitivity and specificity for IPA detection (table 2) [12]. figure 2 outlines a diagnostic algorithm for IPA in high-risk hematologic cancer patients. Early chest CT is crucial in patients with positive serum GM due to the association with more advanced disease and poorer prognosis [24].
FIGURE 2. Diagnostic Approach for IPA in High-Risk Hematologic Cancer Patients
Algorithm outlining the diagnostic steps for invasive pulmonary aspergillosis (IPA) in high-risk hematologic cancer patients. Includes initial assessment, role of serum galactomannan (GM) screening, chest CT, and bronchoalveolar lavage (BAL). AF: antifungal; BAL: bronchoalveolar lavage; CT: computed tomography; EORTC/MSGERC: European Organization for Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium; GM: galactomannan; GVHD: graft versus host disease; HSCT: haematopoietic stem cell transplantation; IA: invasive aspergillosis; MRI: magnetic resonance imaging; ODI: optical density index; PCR: specific polymerase chain reaction for Aspergillus species.
For lower-risk hematologic cancer patients (e.g., chronic leukemia, lymphoma, autologous HSCT), routine antifungal prophylaxis or GM screening is not recommended. However, clinicians should maintain a low threshold for suspicion and promptly investigate with chest CT and further diagnostic tests if IPA is suspected, as diagnosis is often delayed or missed in this group [19].
IPA Diagnosis in Solid Organ Transplant (SOT) Recipients
The incidence of IPA in SOT recipients is estimated at 1–3%, with higher rates in heart and lung transplant recipients [36, 37]. Diagnosing IPA in SOT recipients is challenging due to less specific radiological findings and lower sensitivity of mycological tests compared to hematologic cancer patients.
Radiological Findings: Chest CT findings in SOT recipients are diverse and nonspecific, mimicking bacterial or viral pneumonias. These include:
- Tree-in-bud pattern
- Lobar infiltrates
- Ground-glass opacities
- Nodules and masses (less specific than in hematologic cancer patients)
Mycological Tests: Serum GM sensitivity is lower in SOT recipients (around 40%) compared to hematologic cancer patients [38]. BDG has poor sensitivity and specificity in this population [31, 39]. However, BAL GM and PCR performance is comparable to hematologic cancer patients, with high performance for combined use [40, 41].
Diagnostic Approach: Routine serial monitoring of serum fungal biomarkers is not recommended in SOT patients due to limited sensitivity and specificity [34]. In cases of clinical suspicion (e.g., suggestive chest CT lesion), bronchoscopy with combined mycological testing (culture, GM, PCR) in BAL is the cornerstone for IPA diagnosis.
IPA Diagnosis in Other Immunocompromised Hosts
Limited data exists on diagnostic test performance in other immunocompromised populations (e.g., autoimmune diseases, corticosteroid therapy, Bruton tyrosine kinase inhibitors). However, performance is expected to be similar to nonneutropenic populations like SOT recipients.
IPA Diagnosis in ICU Patients
IPA incidence in the ICU varies greatly. Patients with severe influenza or COVID-19 are at highest risk, with reported incidences from 5 to 30% [42]. IPA is more strongly associated with influenza than COVID-19, with angioinvasion (positive serum GM or histopathology) more frequent in influenza-associated IPA [42–44]. Distinguishing between Aspergillus colonization and true IPA is challenging in COVID-19 [45, 46]. However, Aspergillus detection in respiratory samples is a marker of poor prognosis in both influenza and COVID-19 [4, 6]. Other predisposing conditions in ICU patients include liver cirrhosis, extracorporeal membrane oxygenation, and short-course corticosteroids [5, 47, 48].
Clinical Presentation and Radiology: IPA should be suspected in intubated patients with worsening respiratory status despite antibiotics. Chest CT findings are usually nonspecific and resemble viral or bacterial pneumonias [5, 42, 49, 50].
Diagnostic Criteria in ICU: The EORTC-MSGERC criteria are often not directly applicable to ICU patients without traditional immunosuppressive conditions. Modified diagnostic criteria have been proposed for ICU-acquired IPA, particularly in influenza and COVID-19 [49–51]. Diagnosis typically relies on positive Aspergillus tests (direct exam, culture, GM, or PCR) in BAL fluid. The significance of positive tests in non-BAL respiratory samples (e.g., bronchial aspirates) is less clear. Serum GM sensitivity is around 50–60% in influenza-associated IPA [6, 44], but <15% in COVID-19 [42].
Chronic Pulmonary Aspergillosis (CPA) Diagnosis Criteria
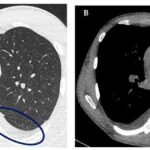
CPA primarily affects individuals with underlying lung diseases (tuberculosis sequelae, nontuberculous mycobacterial infections, lung cancer, bronchiectasis) and minimal or no immunosuppression [2]. Suggestive chest CT imaging is paramount for CPA diagnosis [2].
Radiological Hallmarks of CPA:
- Aspergilloma (Fungus Ball): The most characteristic finding – a mass within a pre-existing lung cavity.
- Cavity Changes: Expansion or wall thickening of existing cavities.
- Parenchymal Destruction and Fibrosis: Developing around pre-existing cavities.
- Pleural Thickening or Effusion
- Bronchial Artery Enlargement or Pseudo-aneurysm
- Aspergillus Nodules: Can mimic lung cancer due to irregular or spiculated borders [2].
Microbiological Documentation: Obtained through cultures of respiratory samples (sputum, BAL). Aspergillus PCR is highly sensitive but may be less specific than culture for distinguishing colonization from infection in CPA [2, 52]. PCR can be useful for detecting azole resistance in patients on antifungal therapy for CPA [53].
Biomarkers and Serology:
- BAL GM: Acceptable sensitivity (75–85%) and specificity (75–80%) in CPA [2, 54, 55].
- Serum GM: Poor sensitivity and not recommended for CPA diagnosis [2, 56].
- Anti-Aspergillus IgG or Precipitins: Good positive predictive value for CPA diagnosis, with acceptable sensitivity (75–80%) for aspergilloma, but less so for chronic cavitary pulmonary aspergillosis [2, 57]. Recommended for diagnosis and monitoring treatment response [2].
Treatment Strategies for Pulmonary Aspergillosis
Antifungal (AF) Drug Classes
Three main classes of antifungal drugs are currently used to treat aspergillosis (table 3): polyenes, triazoles, and echinocandins [33, 34]. Novel antifungals like olorofim and fosmanogepix are under clinical investigation and available for compassionate use, offering promise for azole-resistant IPA [58].
TABLE 3. Antifungal Agents for the Treatment of Pulmonary Aspergillosis
Summary table outlining antifungal drug classes (Polyenes, Triazoles, Echinocandins), specific drugs within each class, typical dosages, therapeutic uses (IPA, CPA, prophylaxis), and key comments regarding administration, monitoring, and resistance. Includes drugs like Amphotericin B formulations, Itraconazole, Voriconazole, Posaconazole, Isavuconazole, Caspofungin, Anidulafungin, and Micafungin. D1: day 1; DDI: drug–drug interaction; GGT: gamma glutamyltranspeptidase; GM: galactomannan; IPA: invasive pulmonary aspergillosis; TDM: therapeutic drug monitoring.
Triazoles
Triazoles (itraconazole, voriconazole, posaconazole, isavuconazole) are ergosterol biosynthesis inhibitors, fungicidal against most Aspergillus species, except for rare species like Aspergillus lentulus and Aspergillus calidoustus [59, 60]. Available in IV and oral formulations, their main side effect is hepatotoxicity, more frequent with voriconazole and posaconazole (10–15%) than isavuconazole [25, 61]. Drug-drug interactions are significant due to cytochrome P450 enzyme inhibition, especially with voriconazole [62]. QT interval prolongation is a concern with most triazoles (except isavuconazole), requiring ECG monitoring [63]. Therapeutic drug monitoring (TDM) is recommended for itraconazole, voriconazole, and posaconazole due to pharmacokinetic variability [34]. Voriconazole is first-line for IPA [33, 34], but posaconazole and isavuconazole have shown similar efficacy [25, 61]. Isavuconazole offers advantages of less hepatotoxicity, fewer drug interactions, and more stable pharmacokinetics (less need for TDM) [25, 70]. Azole resistance in A. fumigatus, linked to environmental fungicide use, is a growing concern [71]. Cyp51A gene mutations (TR34/L98H, TR46/Y121F/T289A) confer pan-azole resistance [72]. Azole-resistant IPA is associated with higher mortality [73].
Amphotericin B
Amphotericin B, a polyene, disrupts fungal cell membrane integrity by binding to ergosterol [74], and may also induce oxidative damage [75]. It has broad antifungal activity, fungicidal against most Aspergillus species except A. terreus [74, 76]. Acquired resistance is rare [77]. Lipid formulations of amphotericin B (liposomal amphotericin B, amphotericin B lipid complex, amphotericin B colloidal dispersion) are safer than conventional amphotericin B deoxycholate, with reduced nephrotoxicity (10–15% vs. 33%) and infusion reactions [78, 79]. Voriconazole showed better therapeutic success and fewer adverse events than amphotericin B deoxycholate in a randomized trial [80]. Liposomal amphotericin B has comparable efficacy to voriconazole for IPA [81]. Liposomal amphotericin B is second-line for IPA and first-line for azole-resistant IPA [34], and also used empirically for suspected invasive mold infections due to broader spectrum, including Mucorales and azole-resistant Aspergillus [34]. Local epidemiology of resistant pathogens should guide empirical therapy choice.
Echinocandins
Echinocandins (caspofungin, anidulafungin, micafungin) inhibit beta-glucan synthase, disrupting fungal cell wall integrity [82]. Available only in IV formulations. Rezafungin, a novel echinocandin, allows weekly dosing [83]. Echinocandins have limited in vitro activity against Aspergillus, with fungistatic effects [82]. Caspofungin exhibits a paradoxical effect in vitro (reduced efficacy at higher concentrations), clinical relevance uncertain [82]. Acquired echinocandin resistance is rare [82, 84]. Clinical experience with echinocandin monotherapy is variable, no randomized trials compare echinocandins to amphotericin B or triazoles [82, 85]. Echinocandins are not routinely recommended for IPA monotherapy, except when triazoles or amphotericin B are contraindicated [33, 34]. Combination therapy with voriconazole may be used in severe IPA [34]. While in vitro and animal studies suggest synergy [82, 86, 87], a randomized trial showed only a trend towards improved survival with combination therapy, with significant effect limited to GM-positive patients [26]. Echinocandin-triazole combination is also an option for azole-resistant IPA (alternative to liposomal amphotericin B), but clinical efficacy is unproven [88]. Synergy between echinocandins and amphotericin B is also suggested by preclinical and limited clinical data [82, 89].
Novel AF Agents
Novel antifungals are needed to combat azole-resistant IPA. Olorofim, a dihydroorotate dehydrogenase inhibitor, is fungicidal against all Aspergillus species, including azole-resistant strains [58]. Fosmanogepix (prodrug of manogepix), a glycosylphosphatidylinositol anchor pathway inhibitor, is fungistatic against all Aspergillus species, including resistant strains [58]. Both are in phase II trials for IPA [58], with IV and oral formulations. Ibrexafungerp, an oral beta-glucan synthase inhibitor, has similar Aspergillus activity to echinocandins [58]. A phase II trial is evaluating ibrexafungerp plus voriconazole vs. voriconazole monotherapy for IPA [58]. Other novel agents in development include tetrazoles and encochleated amphotericin B [58].
Therapeutic Approaches for IPA and CPA
Invasive Pulmonary Aspergillosis (IPA) Treatment
Prompt initiation of antifungal therapy is critical when IPA is suspected. If bronchoscopy is planned, antifungal therapy should ideally start after the procedure, but within 24 hours. IPA treatment approach is generally similar across immunocompromised patient subsets. Triazoles (voriconazole, isavuconazole, or posaconazole) are preferred for probable or proven IPA. Liposomal amphotericin B is recommended for possible IPA to cover Mucorales and azole-resistant Aspergillus. Choice of initial therapy is also influenced by liver and kidney function, and potential drug interactions. Combination therapy (triazole plus echinocandin) is reserved for severe or refractory IPA. Surgery is rarely needed, except for source control in cases of pleural/mediastinal involvement, extrapulmonary foci, life-threatening hemoptysis, or nonresponsive disease. Recovery of bone marrow function and reduction of immunosuppression are crucial for treatment success. Tapering immunosuppressants requires careful multidisciplinary consideration to prevent graft rejection, GVHD, or worsening of underlying conditions.
Treatment duration is generally 6–12 weeks, guided by immune recovery and CT scan resolution [33, 34]. PET/CT may have a role in monitoring treatment response, but needs further validation [10, 90]. Secondary prophylaxis may be considered in patients with prolonged immunosuppression [34]. Shorter treatment durations (4–6 weeks) may be considered for immunocompetent ICU patients (e.g., influenza, COVID-19) after ICU discharge [46].
Chronic Pulmonary Aspergillosis (CPA) Treatment
CPA management is complex, requiring a multidisciplinary team. Surgical indications are individualized, considering lesion number/size, underlying lung disease, and lung function. Pre-operative antifungal therapy may be needed for complex surgeries to prevent fungal spillage. Post-operative therapy is considered for partial resections, complex procedures with spillage risk, or histopathology/cultures showing invasion.
In non-surgical cases, antifungal therapy aims to prevent lesion progression, hemoptysis, and improve respiratory symptoms, quality of life, and outcomes [2, 91]. Long-term suppressive therapy is usually necessary, as response is slow and often partial. Regular chest CT (every 3–6 months) monitors treatment response [2]. Oral triazoles are the mainstay of CPA treatment. Itraconazole is often first-line due to low cost and safety [2, 91]. Voriconazole or posaconazole are used for more severe disease [2, 92, 93]. Isavuconazole is an alternative for toxicity or drug interactions. Long-term triazole therapy requires regular dermatologic monitoring for skin cancer [94]. Echinocandin therapy can be considered for triazole intolerance or resistance [2, 95]. Rezafungin or oral ibrexafungerp are potential alternatives, but efficacy data in CPA are lacking.
For non-surgical patients with recurrent hemoptysis despite antifungals, direct instillation of amphotericin B or triazoles into the aspergilloma cavity may be effective [2, 96]. Hemoptysis management may require tranexamic acid or arterial embolization. Surgery is considered for severe or recurrent hemoptysis [2]. CPA management relies heavily on expert opinion due to limited clinical trials [2]. The CPAnet international registry aims to standardize care and improve understanding of CPA [97].
Conclusions
Pulmonary aspergillosis incidence and clinical spectrum are expanding due to increased at-risk populations, including recipients of novel anticancer and immunomodulatory therapies, and the recent influenza and COVID-19 pandemics. Diagnostic challenges arise from heterogeneous presentations and limitations of microbiological tests. Clinicians must be vigilant in suspecting and diagnosing pulmonary aspergillosis in new and atypical patient categories where it is often overlooked. Emerging azole resistance in A. fumigatus is a major concern, but new antifungal drug classes offer promising therapeutic advances.
Points for Clinical Practice
- Pulmonary aspergillosis is increasingly prevalent due to expanding at-risk populations.
- It is increasingly recognized in mildly immunocompromised or apparently immunocompetent patients (e.g., severe influenza or COVID-19).
- Diagnosis is challenging due to limited test sensitivity and specificity, requiring combined diagnostic approaches.
- Treatment is complex due to limited antifungal drug classes and emerging resistance.
Footnotes
Number 7 in the Series “Respiratory infections” Edited by Antoni Torres and Michael S. Niederman
Provenance: Commissioned article, peer reviewed.
Previous articles in this series: No. 1: Kumar K, Daley CL, Griffith DE, et al. Management of Mycobacterium avium complex and Mycobacterium abscessus pulmonary disease: therapeutic advances and emerging treatments. Eur Respir Rev 2022; 31: 210212. No. 2: Cilloniz C, Luna CM, Hurtado JC, et al. Respiratory viruses: their importance and lessons learned from COVID-19. Eur Respir Rev 2022; 31: 220051. No. 3: Cavallazzi R, Ramirez JA. How and when to manage respiratory infections out of hospital. Eur Respir Rev 2022; 31: 220092. No. 4: Reynolds D, Burnham JP, Vazquez Guillamet C, et al. The threat of multidrug-resistant/extensively drug-resistant Gram-negative respiratory infections: another pandemic. Eur Respir Rev 2022; 31: 220068. No. 5: Puerta-Alcalde P, Garcia-Vidal C. Non-Aspergillus mould lung infections. Eur Respir Rev 2022; 31: 220104. No. 6: Al-Tawfiq JA, Kim H, Memish ZA. Parasitic lung diseases. Eur Respir Rev 2022; 31: 220093.
Conflict of interest: F. Lamoth has research funding from Gilead, MSD, Pfizer and Novartis, and has participated in Advisory boards for Gilead, MSD and Pfizer. All contracts were made with and fees paid to his institution (CHUV).
Conflict of interest: T. Calandra has participated in advisory boards or consulted for Menarini, Shinogi, Cytosorbent, ThermoFisher and GE Healthcare for projects unrelated to the submitted work and on data safety monitoring boards for Cidara and Novartis. All contracts were made with and fees paid to his institution (CHUV).
This article has an editorial commentary: https://doi.org/10.1183/16000617.0150-2022
References
[1] Patterson TF, Thompson GR 3rd, Denning DW, et al. Executive Summary: Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis 2016; 63: 433–42.
[2] Denning DW, Cadranel J, Beigelman-Aubry C, et al. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management. Eur Respir J 2016; 47: 45–68.
[3] Ullmann AJ, Lipton JH, Vesole DH, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med 2007; 356: 335–47.
[4] Koehler P, Cornely OA, Bottiger BW, et al. European Confederation of Medical Mycology Focused Workshop Group on ‘Aspergillus’ in critically ill patients. European expert consensus definition of invasive pulmonary aspergillosis in critically ill, non-immunocompromised patients. Intensive Care Med 2020; 46: 1879–88.
[5] Blot SI, Taccone FS, Van den Abeele AM, et al. European Society of Clinical Microbiology and Infectious Diseases Study Group of Invasive Fungal Infections. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Clin Infect Dis 2012; 54: 53–60.
[6] Schauwvlieghe AF, Rijnders BJ, Philips N, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med 2018; 6: 782–92.
[7] Guinea J, Recio R, Escribano P, et al. Epidemiology of invasive aspergillosis in a tertiary care hospital: a 7-year study. Eur J Clin Microbiol Infect Dis 2010; 29: 1537–41.
[8] Patterson TF, Seibel NL, Sampson J, et al. Aspergillosis in pediatric oncology patients: the changing epidemiology. Clin Infect Dis 2001; 32: 1553–8.
[9] Donnelly JP, Chen SC, Kauffman CA, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis 2020; 71: 1367–76.
[10] Huppert LA, Perfect JR. Invasive Aspergillosis. Open Forum Infect Dis 2021; 8: ofab622.
[11] Lewis RE. Current and emerging approaches to the diagnosis of invasive fungal diseases. Expert Rev Anti Infect Ther 2011; 9: 913–24.
[12] De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 2008; 46: 1813–21.
[13] White PL, Barnes RA, Barton R, et al. UK National Mycology Reference Laboratory; European Aspergillus PCR Initiative. Development of a standardized method for detection of invasive aspergillosis by polymerase chain reaction. J Clin Microbiol 2010; 48: 1232–9.
[14] Lin SJ, Marty FM, Baden LR, et al. Aspergillosis in patients with hematologic malignancy in the era of new antifungal agents. Cancer 2003; 97: 2657–66.
[15] Neofytos D, Horn D, Anaissie E, et al. Epidemiology and outcome of invasive fungal infections in adult hematopoietic stem cell transplant recipients: analysis of Multicenter Prospective Antifungal Therapy (PATH) Alliance registry. Clin Infect Dis 2009; 48: 265–73.
[16] Kontoyiannis DP, Marr KA, Park BJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) Database. Clin Infect Dis 2010; 50: 1091–100.
[17] Fisher CE, Prasad V, Sahasranaman S, et al. Invasive fungal infections following allogeneic hematopoietic stem cell transplantation: recent trends and impact of newer antifungal agents. Bone Marrow Transplant 2012; 47: 721–7.
[18] Park SY, Cho SY, Lee DG, et al. Changing epidemiology and risk factors for invasive fungal infections in patients with acute leukemia. Leukemia Lymphoma 2012; 53: 718–24.
[19] Pagano L, Caira M, Candoni A, et al. Invasive aspergillosis in haematologic patients: changes in epidemiology, diagnosis, and therapy. Haematologica 2007; 92: 1545–55.
[20] perfect JR, Cox GM. Aspergillosis. Infect Dis Clin North Am 2000; 14: 541–70.
[21] Ruhnke M, Grosse-Koning K, Schmidt-Hieber M, et al. Posaconazole for secondary prophylaxis of invasive fungal infections in patients with hematologic malignancies and hematopoietic stem cell transplant recipients: a retrospective analysis. Eur J Haematol 2010; 85: 42–8.
[22] Lamoth F. Aspergillosis complicating chronic granulomatous disease and primary antibody deficiencies. Semin Respir Crit Care Med 2021; 42: 799–814.
[23] Caillot D, Couaillier JF, Bernard A, et al. Increasing volume and changing characteristics of invasive pulmonary aspergillosis lesions during amphotericin B therapy assessed by computed tomography. Clin Infect Dis 1996; 22: 28–32.
[24] Herbrecht R, Letscher-Bru V, Oprea C, et al. Invasive aspergillosis in haematopoietic stem cell transplant recipients: diagnostic yield of transbronchial biopsy and bronchoalveolar lavage. Bone Marrow Transplant 2001; 28: 777–80.
[25] Maertens JA, Rahav G, Lee MY, et al. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. Lancet 2016; 387: 760–9.
[26] Marr KA, Boeckh M, Carter RA, et al. Combination antifungal therapy for invasive aspergillosis. Clin Infect Dis 2004; 39: 797–807.
[27] Ruiz-Camps I, Limper AH, Segal LN, et al. Aspergillosis: pathogenesis, diagnosis, and treatment. Semin Respir Crit Care Med 2021; 42: 715–17.
[28] Arvanitis M, Arikan-Akdagli S, Bruggemann RJ, et al. European Aspergillus PCR Initiative. Molecular detection of aspergillosis: systematic review and meta-analysis. Clin Microbiol Infect 2014; 20: 113–22.
[29] Avni T, Grossman Z, Leibovici L, et al. Bronchoalveolar lavage galactomannan for diagnosis of invasive pulmonary aspergillosis in non-neutropenic patients—systematic review and meta-analysis. Clin Microbiol Infect 2012; 18: 959–66.
[30] Heng J, Chen SC, Marriott D, et al. Meta-analysis of diagnostic performance of bronchoalveolar lavage galactomannan and PCR for invasive pulmonary aspergillosis. J Clin Microbiol 2017; 55: 2204–14.
[31] Ostrosky-Zeichner L, Alexander BD, Kett DH, et al. Multicenter prospective evaluation of the β-d-glucan assay as aid to diagnosis of invasive fungal infections. Am J Respir Crit Care Med 2005; 171: 1265–70.
[32] Ellis M, Al Abdely H, Sandison T, et al. Prospective evaluation of performance characteristics of the β-d-glucan assay for diagnosis of invasive fungal infections in high-risk neutropenic patients. Clin Infect Dis 2008; 46: 34–41.
[33] Ullmann AJ, Aguado JM, Arikan-Akdagli S, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect 2018; 24 Suppl 1: e1–e38.
[34] Tissot F, Agrawal S, Pagano L, et al. ECIL-6 guidelines for the treatment of invasive aspergillosis, candidiasis and mucormycosis in haematological malignancy and transplant recipients. Haematologica 2017; 102: 433–44.
[35] Cordonnier C, Pautas C, Maury S, et al. Galactomannan antigenemia for the diagnosis of invasive pulmonary aspergillosis in neutropenic patients. Clin Infect Dis 1999; 29: 1–6.
[36] Singh N, Husain S. Invasive aspergillosis in solid organ transplant recipients. Am J Transplant 2003; 3: 1094–104.
[37] Husain S, Kwak EJ, Zuckerman R, et al. Invasive aspergillosis after lung transplantation. Am J Respir Crit Care Med 2004; 169: 596–601.
[38] Pfeiffer J, Reischauer B, Lass-Florl C, et al. Galactomannan in bronchoalveolar lavage fluid improves diagnosis of invasive pulmonary aspergillosis and may allow for early treatment. Bone Marrow Transplant 2006; 37: 737–42.
[39] Hayden RT, Mihu MR, Roberts JS, et al. Evaluation of the Platelia Aspergillus enzyme immunoassay and the Fungitell β-d-glucan assay for diagnosis of invasive fungal infections in solid organ transplant recipients. Clin Infect Dis 2008; 46: e88–98.
[40] Marty FM, Koo S, Bryar JM, et al. Bronchoalveolar lavage galactomannan, chitin, and polymerase chain reaction assays for diagnosing invasive aspergillosis after lung transplantation. Transplantation 2007; 84: 749–57.
[41] Singh N, Aris R, Blair JE, et al. Invasive aspergillosis in recipients of lung transplants: association with airway colonization and implications for prevention. Am J Respir Crit Care Med 2005; 171: 771–6.
[42] Alanazi M, Alhabo M, Alenzi FQ, et al. Invasive pulmonary aspergillosis in critically ill COVID-19 patients: a systematic review and meta-analysis. J Fungi (Basel) 2021; 7: 1087.
[43] Wiederhold NP. Invasive pulmonary aspergillosis in influenza patients: more common and more deadly? Lancet Respir Med 2018; 6: 737–8.
[44] van de Veerdonk FL, Kullberg BJ, Lestrade PP, et al. Influenza-associated invasive aspergillosis in critically ill patients. Intensive Care Med 2017; 43: 1118–20.
[45] Verweij PE, Gangneux JP, Bassetti M, et al. ECCMID and ESCMID joint guidelines for the diagnosis and management of mucormycosis 2023. Clin Microbiol Infect 2023; 29 Suppl 1: 1–92.
[46] Gangneux JP, Bouree P, Lanternier F, et al. Fungal complications of COVID-19: current knowledge and future perspectives. Lancet Respir Med 2020; 8: 1071–3.
[47] Taccone FS, Van den Abeele AM, Bulpa P, et al. European Society of Clinical Microbiology and Infectious Diseases Study Group of Invasive Fungal Infections. Epidemiology of invasive aspergillosis in critically ill patients: clinical presentation, underlying risk factors, and outcome. Crit Care Med 2015; 43: 441–9.
[48] Morrissey CO, Chen SC, Sorrell TC, et al. Galactomannan and PCR versus culture and microscopy for diagnosing invasive aspergillosis in critically ill patients: a systematic review and meta-analysis. Crit Care Med 2013; 41: 2441–50.
[49] Khanna N, Kraft CA, Cornely OA, et al. IPA COVID-19 Study Group. Invasive pulmonary aspergillosis and coronavirus disease 2019: interim guidance from the IPA COVID-19 Study Group. Mycoses 2020; 63: 649–66.
[50] Hoenigl M, Seidel D, Carvalho A, et al. ECCMID Study Group for Infections in Critically Ill Patients (ESGCIP); European Confederation of Medical Mycology (ECMM). ECCMID/ESCMID guideline for the diagnosis and management of mucormycosis 2019. Clin Microbiol Infect 2020; 26 Suppl 1: 1–26.
[51] Meersseman W, Lagrou K, Maertens J, et al. Invasive aspergillosis in critically ill patients without classic risk factors. Am J Respir Crit Care Med 2004; 170: 621–5.
[52] Duyk CA, Woods G, McCarthy DI, et al. Utility of PCR for diagnosis of chronic pulmonary aspergillosis. J Clin Microbiol 2014; 52: 4157–61.
[53] Astvad KM, Hare RK, Jensen JS, et al. Clinical value of Aspergillus PCR for diagnosis of chronic pulmonary aspergillosis and for prediction of azole resistance. J Clin Microbiol 2017; 55: 2859–67.
[54] Page ID, Richardson M, Denning DW. Bronchoalveolar lavage fluid galactomannan for the diagnosis of chronic pulmonary aspergillosis. Thorax 2004; 59: 497–500.
[55] Lortholary O, Gangneux JP, Sitbon K, et al. European Confederation of Medical Mycology (ECMM). European Confederation of Medical Mycology (ECMM) consensus criteria for defining chronic pulmonary aspergillosis and its subtypes: a proposal. Clin Microbiol Infect 2011; 17 Suppl 5: 19–25.
[56] Kauffman CA, Dewsnup DH, Pappas PG, et al. Serum galactomannan antigen detection for diagnosis of invasive aspergillosis in patients with AIDS. Clin Infect Dis 1994; 19: 313–15.
[57] Binder RE, Faling LJ, Pugatch RD, et al. Chronic necrotizing pulmonary aspergillosis: a discrete clinical entity. Medicine (Baltimore) 1982; 61: 109–24.
[58] McCarthy MW, Warris A, Petraitiene R, et al. New antifungal agents in development for invasive aspergillosis. Curr Opin Infect Dis 2023; 36: 523–32.
[59] Howard SJ, Cerar D, Anderson MJ, et al. Azole antifungal resistance in Aspergillus fumigatus associated with cystic fibrosis. Antimicrob Agents Chemother 2006; 50: 2581–2.
[60] Lortholary J, Alanio A, Lanternier F, et al. Invasive infections due to Aspergillus species other than A. fumigatus. Clin Microbiol Infect 2011; 17: 1723–34.
[61] Ullmann AJ, Schuster MG, Schlamm HT, et al. IDSA Aspergillosis Guideline Panel. Antifungal stewardship: optimizing antifungal therapy in patients with invasive aspergillosis. Clin Infect Dis 2018; 67: 1581–92.
[62] Lempers VJ, Burger DM, Aarnoutse RE, et al. Drug–drug interactions of antifungal agents in patients with invasive fungal infections. Expert Opin Drug Metab Toxicol 2018; 14: 457–69.
[63] Lewis JS 2nd, Mueller SW, Rogers PD, et al. Voriconazole-induced QT prolongation: case series and review of the literature. Ann Pharmacother 2011; 45: 177–85.
[64] Park S, Kim KH, Kim ES, et al. Therapeutic drug monitoring of voriconazole and clinical implications in patients with invasive fungal infections. Ther Drug Monit 2011; 33: 75–83.
[65] Troke PF, Hockey H, Hope WW. Observational study of the clinical efficacy of voriconazole and its relationship to plasma concentrations in patients with invasive fungal infections. J Antimicrob Chemother 2011; 66: 1782–9.
[66] Hyland R, Jones BC, Smith DA. Identification of the cytochrome P450 enzymes responsible for the metabolism of voriconazole and prediction of drug interactions. Drug Metab Dispos 2003; 31: 540–7.
[67] Courtney R, Pai S, Laughlin M, et al. Posaconazole oral suspension: effect of food and gastric acid-reducing agents on absorption. Antimicrob Agents Chemother 2003; 47: 2188–92.
[68] Krishna G, Motwani T, Ma L, et al. Pharmacokinetics and absolute bioavailability of posaconazole tablet. Antimicrob Agents Chemother 2012; 56: 6274–80.
[69] Schreuder I, van Ramshorst J, Burger DM, et al. Isavuconazole: pharmacology, clinical efficacy and safety. Expert Rev Anti Infect Ther 2018; 16: 31–42.
[70] Cornely OA, Maertens J, Bresnik M, et al. Isavuconazole for primary treatment of invasive mold disease caused by Aspergillus and rare molds: final results of the SECURE trial. Mycoses 2019; 62: 707–15.
[71] Fisher MC, Hawkins NJ, Sanglard D, et al. Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science 2018; 360: 739–42.
[72] Snelders E, van de Veerdonk FL, van den Brink MR, et al. Azole resistance in Aspergillus fumigatus: mechanisms and clinical consequences. Fungal Genet Biol 2011; 48: 196–204.
[73] Buehler L, Clancy CJ, Nguyen MH. Azole-resistant aspergillosis: epidemiology, diagnosis, and management. Drugs 2017; 77: 1229–47.
[74] Brajtburg J, Bolard J. Amphotericin B: mechanism of action and clinical implications. Clin Infect Dis 1992; 15: 486–99.
[75] Sokol-Anderson M, Brajtburg J, Medoff G. Amphotericin B-induced oxidative damage to fungal cells. J Antimicrob Chemother 1986; 17: 29–36.
[76] Hope WW, Castagnola E, Groll AH, et al. International Pediatric Fungal Network. Isavuconazole for primary treatment of invasive aspergillosis in children. J Pediatr Infect Dis Soc 2016; 5: 433–8.
[77] Steinbach WJ, Schell WA, Miller GG, et al. Amphotericin B resistance in Aspergillus terreus. Antimicrob Agents Chemother 2002; 46: 3407–9.
[78] Laniado-Laborín R, Cabrales-Vargas MN. Amphotericin B: side effects and toxicity. J Antimicrob Chemother 2009; 63 Suppl 1: i47–58.
[79] Dupont B, Dromer F, Sanglard D, et al. French Mycosis Study Group. Comparative safety and efficacy of liposomal amphotericin B (AmBisome) and amphotericin B deoxycholate in the treatment of invasive mycoses in neutropenic patients. Clin Infect Dis 1999; 29: 1469–75.
[80] Herbrecht R, Denning DW, Patterson TF, et al. Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 2002; 347: 408–15.
[81] Cornely OA, Böhme A, Ruhnke M, et al. Liposomal amphotericin B as initial therapy for invasive aspergillosis in patients with hematologic malignancies. Haematologica 2007; 92: 1669–72.
[82] Denning DW. Echinocandins and aspergillosis. Clin Infect Dis 2006; 42 Suppl 3: S243–51.
[83] Lepak AJ, VanScoy B, Schmidt S, et al. Pharmacokinetics and pharmacodynamics of rezafungin, a novel echinocandin antifungal. Antimicrob Agents Chemother 2020; 64: e02427-19.
[84] Shields RK, Nguyen MH, Clancy CJ. Echinocandin resistance in Aspergillus fumigatus: risk factors and outcomes. Clin Infect Dis 2013; 57: 643–51.
[85] Marr KA, Laverdiere M, Guglielmo BJ, et al. Caspofungin versus amphotericin B for primary therapy of invasive aspergillosis. Clin Infect Dis 2004; 39: 797–807.
[86] Lewis RE, Albert ND, Kontoyiannis DP. Combination antifungal therapy for invasive aspergillosis: current status and future directions. Med Mycol 2009; 47 Suppl 1: S355–63.
[87] Kontoyiannis DP, Lewis RE, Osherov N, et al. Caspofungin-voriconazole combination therapy for experimental invasive aspergillosis: evidence of synergy and enhanced tissue concentrations of voriconazole. Antimicrob Agents Chemother 2005; 49: 3305–11.
[88] Park SJ, Choi SM, Lee DG, et al. Combination therapy with voriconazole and caspofungin for invasive aspergillosis caused by azole-resistant Aspergillus fumigatus. Antimicrob Agents Chemother 2015; 59: 5401–5.
[89] Andes DR, van Ogtrop ML, Peng J, et al. In vivo comparison of amphotericin B and caspofungin alone and in combination for Aspergillus fumigatus infection. Antimicrob Agents Chemother 2004; 48: 1147–51.
[90] von Lilienfeld-Toal M, Wagener N, Einsele H, et al. 18F-FDG PET/CT for response assessment of invasive fungal infections in neutropenic patients-a systematic review and meta-analysis. J Nucl Med 2018; 59: 709–16.
[91] Schweitzer-Krantz S, Patterson TF. Chronic pulmonary aspergillosis: a review of clinical manifestations, diagnosis, and therapy. Semin Respir Crit Care Med 2021; 42: 785–98.
[92] Hope WW, Walsh TJ, Denning DW. Posaconazole for chronic pulmonary aspergillosis. Antimicrob Agents Chemother 2006; 50: 1579–82.
[93] Kauffman CA, Isa