Audiograms are fundamental tools in healthcare, specifically designed for the diagnosis and monitoring of hearing loss across all age groups. These graphical representations are created by meticulously plotting the softest sounds a patient can hear at various frequencies, offering a detailed snapshot of their auditory capabilities. The interpretation of an audiogram, known as Audiogram Diagnosis, is crucial for differentiating between types of hearing loss, such as conductive and sensorineural, and for guiding subsequent medical or surgical interventions aimed at improving or preserving hearing function. This article delves into the essentials of audiogram diagnosis, providing a comprehensive overview for understanding these vital hearing tests.
Decoding the Audiogram: Intensity and Frequency
To effectively understand an audiogram diagnosis, it’s essential to grasp the concepts of sound intensity and frequency, which are the axes upon which audiograms are built.
Intensity, often perceived as loudness, is measured in decibels (dB). The decibel scale is logarithmic, meaning that a small increase in dB represents a significant jump in sound intensity. For instance, an increase of 10 dB signifies a tenfold increase in sound intensity, while a 20 dB increase makes the sound 100 times more intense. Standard audiograms typically assess hearing across an intensity range of 0 to 110 dB. To put this into perspective, normal conversational speech registers around 60 dB.
| Common Sounds and Their Intensity (dB) |
|—|—|—|
| Near-total silence | 0 dB | Lawnmower | 90 dB |
| Whispering | 15 dB | Car Horn | 110 dB |
| Refrigerator Hum | 40 dB | Jackhammer | 120 dB |
| Normal Conversation | 60 dB | Gun Shot or Firework | 140 dB |
| Vacuum Cleaner | 70 dB | Jet Takeoff | 150 dB |
Frequency, often associated with the pitch of a sound, is measured in Hertz (Hz). The typical range of human hearing spans from 20 to 20,000 Hz. Audiometric testing focuses on the frequencies most relevant to human speech, generally testing between 250 Hz and 8000 Hz, as human speech typically falls within the 250 Hz to 6000 Hz range.
The Process of Audiometric Testing
Audiometric testing is the procedure used to create an audiogram, and it is adapted based on the patient’s age to ensure accurate and reliable results. During the test, an audiometer, a specialized instrument, delivers “pure tone” sounds at specific frequencies and intensities. The test begins with sounds at levels expected to be easily heard and progressively decreases the intensity until the patient can no longer perceive the sound. This threshold is then recorded for each frequency tested.
For different age groups, audiometric testing techniques vary:
- Evoked Otoacoustic Emissions (EOAE): This test measures the function of the outer hair cells in the cochlea and is frequently used as a newborn hearing screening tool.
- Auditory Brainstem Response (ABR): ABR testing uses electrodes to monitor brainwave activity in response to sound stimuli. It’s applicable across all ages but often requires sedation for children older than 6 months to ensure stillness during the test.
- Behavioral Observation Audiometry (BOA) (0 to 5 months): BOA involves observing a child’s behavioral responses to sound stimuli. While useful for very young infants, it does not provide ear-specific information (laterality).
- Visual Reinforcement Audiometry (VRA) (6 months to 2 years): In VRA, a child is trained to turn towards a visual reward, such as a lighted toy, when they hear a sound. This method can assess hearing in each ear separately.
- Conditioned Play Audiometry (CPA) (2 to 5 years): CPA engages children by teaching them to perform a play-based activity, like placing a toy in a bucket, whenever they hear a sound. This method can also assess hearing in each ear independently.
- Conventional Pure-Tone Audiometry (5 years and older): This is the standard method for older children and adults, where the individual raises their hand or presses a button in response to hearing a sound.
| DEGREES OF HEARING LOSS |
|—|—|—|
| Degree of Hearing Loss | Thresholds (dB) | Description |
| Normal | 0-25 Adult (0-15 infant) | Normal Hearing |
| Mild | 20-40 | Difficulty hearing soft sounds and whispers; may struggle in noisy environments. |
| Moderate | 41-55 | Difficulty hearing quieter conversations. |
| Moderate Severe | 56-70 | Difficulty hearing normal conversation; may rely on lip-reading or hearing aids. |
| Severe | 71-90 | Can only understand speech when spoken loudly and in close proximity. |
| Profound | >90 | Generally unable to understand speech and may not hear loud sounds like lawnmowers or heavy traffic. |
Types of Hearing Loss Identified Through Audiogram Diagnosis
Audiogram diagnosis is instrumental in differentiating between the main types of hearing loss: conductive, sensorineural, and mixed.
Conductive Hearing Loss (CHL) occurs when sound waves are unable to effectively reach the inner ear. This type of hearing loss often arises from obstructions or issues in the outer or middle ear. Common causes of conductive hearing loss include:
- Cerumen Impaction: Earwax buildup blocking the ear canal.
- Perforated Tympanic Membrane: A hole or rupture in the eardrum.
- Middle Ear Effusion: Fluid accumulation in the middle ear space, often due to infection.
- Otosclerosis: Abnormal bone growth in the middle ear that hinders the movement of the ossicles.
Conductive hearing losses are often more amenable to medical or surgical correction compared to sensorineural losses. Clinical tests like the Rinne and Weber tests can provide preliminary insights into conductive hearing loss. The Weber test involves placing a vibrating tuning fork on the midline of the head; in unilateral conductive hearing loss, the sound lateralizes to the affected ear. The Rinne test compares air conduction and bone conduction; conductive hearing loss is indicated when bone conduction is perceived louder than air conduction in the affected ear (negative Rinne).
Sensorineural Hearing Loss (SNHL) results from damage to the inner ear structures, specifically the cochlea, or the auditory nerve pathways leading to the brain. SNHL is the most prevalent type of permanent hearing loss. Common causes include:
- Noise Exposure: Prolonged exposure to loud noises is a leading cause of SNHL.
- Aging (Presbycusis): Age-related degeneration of the inner ear.
- Ototoxic Medications: Certain medications can damage the inner ear.
- Genetic Factors: Hereditary conditions can predispose individuals to SNHL.
- Infections: Diseases like meningitis, mumps, and measles can cause SNHL.
- Head Trauma: Injuries, particularly temporal bone fractures, can damage the inner ear.
- Congenital Malformations: Structural abnormalities of the inner ear present from birth.
- Acoustic Neuroma or Meningioma: Tumors affecting the auditory nerve.
Sensorineural hearing loss is often less easily corrected through surgical means compared to conductive hearing loss, and management typically involves hearing aids, cochlear implants, or other rehabilitative strategies.
Mixed Hearing Loss is diagnosed when both conductive and sensorineural components are present. This indicates issues in both the outer or middle ear and the inner ear or auditory nerve.
Interpreting the Audiogram: A Visual Representation of Hearing
The audiogram itself is a graph where hearing thresholds are plotted. The y-axis represents intensity in decibels (dB HL), starting from 0 dB at the top (better hearing) and increasing downwards (poorer hearing). The x-axis represents frequency in Hertz (Hz), progressing from low to high frequencies from left to right.
Symbols on the audiogram denote different aspects of hearing:
- O: Thresholds for air conduction in the right ear.
- X: Thresholds for air conduction in the left ear.
- <: Thresholds for bone conduction in the right ear, mastoid placement.
- >: Thresholds for bone conduction in the left ear, mastoid placement.
Key audiometric measures include:
- Threshold: The softest sound level heard at least 50% of the time.
- Speech Reception Threshold (SRT): The lowest intensity at which a person can repeat bisyllabic words (spondees) 50% of the time. SRT should correlate with pure-tone average thresholds.
- Word Recognition Score: The percentage of words correctly identified at a comfortable listening level, indicating speech clarity.
- Speech Discrimination: Similar to word recognition, but often tested at a louder intensity (e.g., 30 dB above SRT) to assess maximum speech understanding.
- Acoustic Reflex: Measures muscle contractions in the middle ear in response to loud sounds, testing both ipsilateral and contralateral reflexes.
- Tympanometry: Assesses middle ear function by measuring ear canal volume and tympanic membrane mobility using air pressure changes. Tympanometry results are classified into types (A, B, C) that indicate normal function, fluid presence, or negative pressure.
It is important to note that while patients often seek a “percentage of hearing loss,” audiogram results in decibels do not directly translate into a meaningful percentage due to the logarithmic nature of the decibel scale. Formulas to calculate “percent disability” exist primarily for disability pension eligibility and should not be misinterpreted as a direct measure of hearing loss percentage in a clinically meaningful way.
Noise-Induced Hearing Loss and the Audiogram “Notch”
Chronic noise exposure is a significant risk factor for hearing loss, and audiogram diagnosis plays a crucial role in identifying Noise-Induced Hearing Loss (NIHL). A characteristic feature of NIHL on an audiogram is a “notch” at 4000 Hz. This dip in hearing thresholds at 4000 Hz, with recovery at higher frequencies, is highly indicative of damage from noise exposure. Sounds at or above 85 dB, when experienced for prolonged durations, can cause hearing damage. If you need to raise your voice to be heard in an environment, it’s likely that the noise level exceeds 80 dB and poses a risk to your hearing over time.
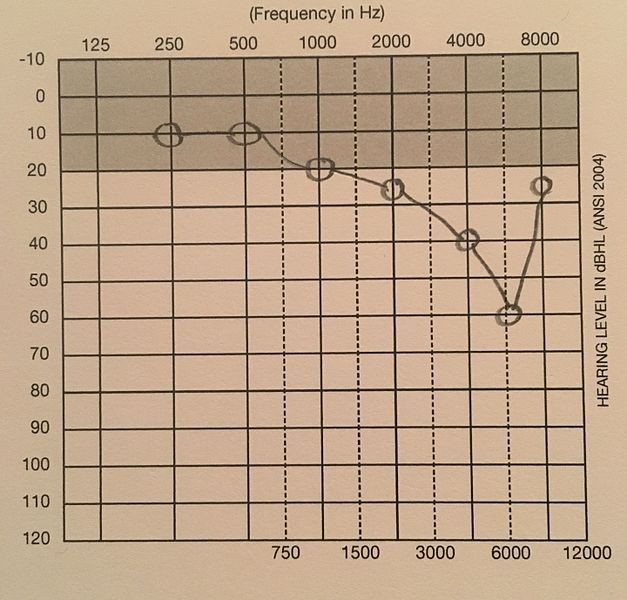 Example of Notched Audiogram indicative of Noise-Induced Hearing Loss
Example of Notched Audiogram indicative of Noise-Induced Hearing Loss
Image depicting a notched audiogram, a common indicator of Noise-Induced Hearing Loss (NIHL), showing a characteristic dip in hearing thresholds at the 4000Hz frequency.
Conclusion
Audiogram diagnosis is an indispensable component of audiology and otolaryngology, providing essential information for the evaluation, diagnosis, and management of hearing loss. By carefully interpreting audiograms, healthcare professionals can accurately classify the type and degree of hearing loss, guide appropriate interventions, and monitor hearing health over time. Understanding the principles of audiometry and the nuances of audiogram interpretation is vital for anyone involved in hearing healthcare and for individuals seeking to understand their own or their family’s hearing abilities.