Autoimmune diseases occur when the body’s immune system, which is designed to fight off harmful invaders like bacteria and viruses, mistakenly attacks healthy cells. This misdirection can lead to a wide range of conditions affecting various parts of the body, from the skin and joints to internal organs. While there are over 80 known autoimmune diseases, pinpointing the exact condition can be a complex and lengthy process, often requiring expert Autoimmune Disease Diagnosis strategies.
The Complexity of Autoimmune Disease Diagnosis
Diagnosing autoimmune diseases is not straightforward. Unlike infections where specific pathogens can be identified through tests, autoimmune conditions are characterized by the immune system’s malfunction. There isn’t usually a single, definitive test to confirm most autoimmune diseases. Adding to the complexity, many autoimmune conditions share overlapping symptoms with each other and with other illnesses. Symptoms like fatigue, muscle aches, and low-grade fever are common across various health issues, making it challenging to immediately suspect an autoimmune disorder. This diagnostic ambiguity often necessitates a thorough and multifaceted approach.
Navigating the Diagnostic Path
The journey to an autoimmune disease diagnosis typically involves several key steps:
-
Comprehensive Medical History and Physical Examination: The first step involves a detailed discussion about your symptoms, their onset, duration, and any factors that worsen or relieve them. Your doctor will also inquire about your family medical history, as autoimmune diseases often have a genetic component. A thorough physical examination helps assess objective signs of illness, such as inflammation, rashes, or joint swelling.
-
Blood Tests: Unraveling Immune System Clues: Blood tests are crucial in the diagnostic process. While no single blood test can definitively diagnose most autoimmune diseases, a panel of tests can help identify patterns and markers indicative of immune system dysfunction. Commonly used blood tests include:
- Antinuclear Antibody (ANA) test: This test is often the first step in screening for autoimmune diseases. A positive ANA test suggests the possibility of an autoimmune disorder, but it’s not specific to any one disease and can be positive in healthy individuals as well.
- Autoantibody tests: These tests look for specific antibodies that target the body’s own tissues. Examples include rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies (for rheumatoid arthritis), anti-dsDNA antibodies (for lupus), and others. The presence and type of autoantibodies help narrow down diagnostic possibilities.
- Inflammatory markers: Tests like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) measure general inflammation levels in the body. Elevated levels can support the suspicion of an autoimmune or inflammatory condition, although they are not specific to autoimmune diseases.
- Complete Blood Count (CBC) and Metabolic Panel: These routine tests assess overall health and can reveal abnormalities that might be associated with autoimmune diseases or help rule out other conditions.
-
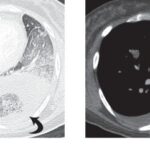
Imaging Studies: Visualizing Internal Impact: Imaging techniques play a vital role in assessing the extent and nature of organ involvement in autoimmune diseases. X-rays, ultrasounds, CT scans, and MRIs can visualize joints, organs, and tissues, helping to identify inflammation, damage, or structural changes caused by the autoimmune process. For example, joint damage in rheumatoid arthritis can be assessed with X-rays, while MRI can provide detailed images of soft tissues affected by conditions like lupus.
-
Specialist Referrals: Expertise for Complex Cases: Given the complexity of autoimmune diseases, referral to a specialist is often necessary. The type of specialist depends on the suspected condition and the body systems involved. Common specialists include:
- Rheumatologists: Experts in autoimmune diseases affecting joints, muscles, and bones, such as rheumatoid arthritis, lupus, and scleroderma.
- Dermatologists: Specialists in skin conditions, including autoimmune skin diseases like psoriasis and pemphigus.
- Gastroenterologists: Specialists in digestive system disorders, including autoimmune conditions like Crohn’s disease and ulcerative colitis.
- Endocrinologists: Experts in hormone disorders, including autoimmune thyroid diseases like Hashimoto’s thyroiditis and Graves’ disease.
- Neurologists: Specialists in nervous system disorders, including autoimmune conditions like multiple sclerosis and myasthenia gravis.
-
The Importance of Time and Observation: Autoimmune disease diagnosis can be a process of elimination and observation over time. Symptoms may fluctuate, and the clinical picture can evolve. Doctors often need to monitor the patient’s condition, repeat tests, and assess response to treatments to refine the diagnosis. Sometimes, it may take months or even years to arrive at a definitive diagnosis.
Patient Advocacy in the Diagnostic Journey
Being an active participant in your healthcare journey is crucial for effective autoimmune disease diagnosis. This includes:
- Detailed Symptom Tracking: Keep a thorough record of your symptoms, including when they occur, how long they last, their severity, and any triggers or relieving factors. This information is invaluable for your doctor.
- Family Health History: Gather information about autoimmune diseases or related conditions in your family. Sharing this with your doctor can raise suspicion and guide diagnostic testing.
- Open Communication: Don’t hesitate to ask questions, express concerns, and advocate for yourself. Clear and open communication with your healthcare team is essential for navigating the diagnostic process.
- Seeking Second Opinions: If you feel uncertain about your diagnosis or treatment plan, seeking a second opinion from another specialist can provide reassurance and alternative perspectives.
Conclusion: Towards Accurate Autoimmune Disease Diagnosis
Diagnosing autoimmune diseases is a challenging but critical process. It requires a combination of careful clinical evaluation, targeted laboratory testing, imaging studies, and specialist expertise. While it can be a lengthy journey, advancements in diagnostic tools and a collaborative approach between patients and healthcare providers are continuously improving the accuracy and timeliness of autoimmune disease diagnosis, paving the way for effective management and improved quality of life.