Introduction
Autosomal dominant polycystic kidney disease (ADPKD) stands as the most prevalent inherited cause of end-stage kidney disease (ESKD) globally. In the United States alone, it affects approximately 500,000 individuals. This genetic disorder is characterized by the development of fluid-filled cysts in both kidneys, leading to a gradual decline in renal function. Polycystic kidney disease is broadly classified into autosomal dominant polycystic kidney disease and autosomal recessive polycystic kidney disease (ARPKD), based on their inheritance patterns. ADPKD is significantly more common, affecting 1 in 400 to 1,000 individuals, while ARPKD is rarer, with an estimated prevalence of 1 in 20,000 to 40,000 live births.
ADPKD is a progressive and multisystemic condition. Beyond bilateral renal cyst formation and kidney enlargement, it involves other organs such as the heart, liver, pancreas, spleen, and arachnoid membranes. Effective Autosomal Dominant Polycystic Kidney Disease Diagnosis is critical for early intervention and management. This article provides an overview of the epidemiology, genetics, clinical presentation, and management of ADPKD, equipping healthcare professionals with the essential knowledge for improved patient care for this complex and widespread condition. Early and accurate autosomal dominant polycystic kidney disease diagnosis is the first step towards slowing disease progression and managing its complications.
Objectives:
- To establish a systematic screening protocol for autosomal dominant polycystic kidney disease diagnosis, incorporating regular imaging and genetic testing, particularly for patients with a family history of ADPKD.
- To formulate appropriate management strategies, including lifestyle adjustments and pharmacological treatments, for patients with a confirmed autosomal dominant polycystic kidney disease diagnosis, aiming to slow disease progression and manage associated complications.
- To implement evidence-based guidelines in the management of ADPKD, including the judicious use of tolvaptan, to optimize patient outcomes following an autosomal dominant polycystic kidney disease diagnosis.
- To promote coordinated care among various healthcare providers, ensuring seamless transitions between primary care, nephrology, and other relevant specialties, thereby optimizing the management of the complex healthcare needs of patients with an autosomal dominant polycystic kidney disease diagnosis.
Etiology
The etiology of ADPKD is rooted in genetic mutations. Several genes are implicated, with two primary genes identified. Mutations in the PKD1 gene, located on chromosome 16p13.3, are responsible for approximately 85% of ADPKD cases. The PKD2 gene, found on 4q21, accounts for around 15% of cases. Accurate autosomal dominant polycystic kidney disease diagnosis often considers these genetic factors, especially in familial cases.
Mutations in the GANAB gene are believed to contribute to approximately 1% of ADPKD patients, often associated with more variable polycystic liver disease. Genetic testing plays an increasingly important role in autosomal dominant polycystic kidney disease diagnosis and risk assessment.
Mutations in both PKD1 and PKD2 genes result in similar disease phenotypes. In the PKD1 form, about 50% of patients progress to require renal replacement therapy by the age of 60. PKD2 mutations typically manifest later in life and are associated with a milder disease course, characterized by fewer renal cysts, delayed onset of hypertension, and a lower incidence of end-stage kidney disease (ESKD) compared to PKD1. These genetic distinctions are increasingly relevant in refining autosomal dominant polycystic kidney disease diagnosis and prognosis.
Epidemiology
ADPKD is a global health concern, affecting individuals across all races. The prevalence rate of diagnosed cases ranges from 1 in 400 to 1 in 1,000 worldwide. While some individuals with ADPKD may remain asymptomatic throughout their lives, it is not considered a benign condition. Approximately half to possibly three-quarters of affected individuals will develop end-stage kidney disease by the age of 70, constituting up to 10% of all ESKD patients. Epidemiological data is crucial for understanding the scope of autosomal dominant polycystic kidney disease diagnosis and its impact.
End-stage kidney disease due to ADPKD is observed less frequently in African Americans compared to White Americans. Data from 1998 to 2001 in the United States indicated that ESKD caused by ADPKD occurred in 8.7 per 1 million men and 6.9 per 1 million women. Comparable data for the same period showed rates of 7.8 and 6.0 per million individuals in Europe and 5.6 and 4.0 per million in Japan. The estimated worldwide incidence is approximately 12.5 million individuals. These global variations highlight the importance of consistent diagnostic approaches for autosomal dominant polycystic kidney disease diagnosis across different populations.
Increased awareness, earlier detection methods, and advancements in hypertension treatment have led to an increase in the age of ESKD onset and a decrease in all-cause mortality associated with ADPKD. Renal disease tends to be more severe in males; however, polycystic liver disease is more prevalent in females, suggesting a potential hormonal influence. Early and accurate autosomal dominant polycystic kidney disease diagnosis coupled with proactive management is key to improving patient outcomes.
Pathophysiology
The pathophysiology of ADPKD is primarily driven by genetic mutations. Eighty-five percent of patients with ADPKD have PKD1 mutations, 15% have PKD2 gene mutations, and around 1% have GANAB gene mutations. A proportion of patients (10% to 15%) with ADPKD have no known family history, suggesting a high rate of de novo mutations. Understanding these genetic underpinnings is fundamental to autosomal dominant polycystic kidney disease diagnosis and potential therapeutic targets.
PKD1 and PKD2 mutations lead to similar disease presentations, but patients with PKD2 mutations generally experience a milder disease course with fewer renal cysts, later onset of hypertension, and less ESKD than those with PKD1. Patients with GANAB mutations also exhibit a milder phenotype compared to PKD1 but are more prone to hepatic disease. These phenotypic variations underscore the complexity of autosomal dominant polycystic kidney disease diagnosis and prognosis.
-
PKD1 encodes polycystin-1 (PC1), a large integral membrane protein with a substantial extracellular N-terminal, 11 transmembrane regions, and a short intracellular C-terminal. PC1 is located in focal adhesions, primary cilia, tight junctions, desmosomes, and adherens junctions, playing a crucial role in cell-to-cell and cell-to-matrix interactions.
-
PKD2 encodes polycystin-2 (PC2), which features a short cytoplasmic N-terminal, 6 transmembrane regions, and a short cytoplasmic C-terminal. PC2 is found in the endoplasmic reticulum, plasma membrane, primary cilia, centrosomes, and mitotic spindles in dividing cells. PC2 is also involved in the regulation of intracellular calcium.
Cystogenesis in ADPKD is characterized by chloride-rich fluid secretion, which is essential for cyst expansion, even after cysts detach from their parent nephron. The accumulation of cyst fluid, rich in chloride and sodium, is dependent on the active luminal excretion of chloride, primarily through the cystic fibrosis transmembrane conductance regulator (CFTR). These cellular mechanisms are important for understanding disease progression following autosomal dominant polycystic kidney disease diagnosis.
Elevated levels of cAMP are observed in animal models of ADPKD in the kidneys, liver, and vascular smooth muscle cells, playing a significant role in the proliferation of various cell types. Cyclic AMP enhances proliferative pathways in cells derived from ADPKD kidneys while inhibiting proliferation in cells from normal human kidneys. This differential cellular response is a key aspect of ADPKD pathophysiology, relevant to potential therapeutic interventions after autosomal dominant polycystic kidney disease diagnosis.
Each renal cyst is believed to originate from a single, genetically altered clonal hyperproliferative epithelial cell. A somatic mutation, often referred to as the “second hit,” in either the PKD1 or PKD2 gene leads to cyst growth and development. The continuous proliferation of epithelial cells, fluid secretion, and alterations in the extracellular matrix result in focal outpouching from the parent nephron. This “second hit” hypothesis is central to understanding cyst formation in autosomal dominant polycystic kidney disease diagnosis.
Cyst formation can occur in both proximal and distal tubules but is most common in the distal nephron and collecting duct. When cysts exceed 2 cm in size, they typically separate from the parent nephron and continue to autonomously secrete fluid, leading to cyst expansion and kidney enlargement. This expansion, in turn, reduces the number of functional nephrons. The ongoing expansion of cysts compresses renal vessels, causing intrarenal ischemia, which activates the renin-angiotensin-aldosterone system and other factors. These structural and functional changes are critical considerations in autosomal dominant polycystic kidney disease diagnosis and management.
Hypertension in ADPKD is thought to be related to localized areas of kidney ischemia resulting from cyst expansion. This ischemia leads to increased renin release and a subsequent rise in blood pressure. The walls of cysts and cells in the connective tissue surrounding cysts contain renin, suggesting that increasing cyst size contributes to worsening hypertension. Hypertension is a common and often early clinical manifestation detected during autosomal dominant polycystic kidney disease diagnosis.
The cysts also initiate an inflammatory response in the surrounding renal parenchyma and promote renal fibrosis. Progressive cyst expansion, increased systemic vascular resistance, sodium retention, and increasing renal fibrosis ultimately lead to ESKD. These progressive pathological changes are crucial in understanding the long-term prognosis following autosomal dominant polycystic kidney disease diagnosis.
Liver cysts are a frequent extrarenal manifestation of ADPKD and are more prevalent in women. They are known to increase in size and number in response to high estrogen states, such as pregnancy and oral contraceptive use. The presence of liver cysts can support autosomal dominant polycystic kidney disease diagnosis, especially in women.
In the hepatic system, the absence of polycystin results in cyst formation, increased cell proliferation and apoptosis, enhanced fluid secretion, abnormal cell–matrix interactions, and alterations in cell polarity. The proliferative and secretive activities of cystic epithelium are regulated by estrogens, either directly or by amplifying growth signals such as nerve growth factor, IGF1, FSH, and VEGF. Understanding these hormonal influences is relevant in managing extrarenal manifestations after autosomal dominant polycystic kidney disease diagnosis.
A higher cyst burden, reflected by increased total kidney volume, is considered a risk factor for the development of hypertension, even in individuals with normal serum creatinine levels. Total kidney volume is an important biomarker in assessing disease severity following autosomal dominant polycystic kidney disease diagnosis.
Histopathology
Histopathological examination of kidney tissue in ADPKD reveals key features. Epithelial cell proliferation, abnormal fluid secretion, and abnormal extracellular matrix deposition by cystic epithelial cells are prominent. These changes are accompanied by alterations in the pericystic blood and lymphatic microvasculature. Histopathology provides crucial insights confirming autosomal dominant polycystic kidney disease diagnosis and understanding disease mechanisms.
Tubular dilation, microcysts, and tubular atrophy are common findings. Tubular dilation is also associated with an enlarged Bowman’s space. Extensive interstitial fibrosis is observed in the peritubular area, particularly near cysts. These histological features are important for differentiating ADPKD from other renal cystic diseases during autosomal dominant polycystic kidney disease diagnosis.
Cyst enlargement causes compression of the surrounding nephrons, interstitium, and renal vasculature. Vascular changes include fibrosclerosis and lumen narrowing. Inflammatory cells, especially fibroblasts and monocytes, are prominent. These structural changes contribute to renal dysfunction in ADPKD and are considered in the comprehensive assessment following autosomal dominant polycystic kidney disease diagnosis.
History and Physical
Patients with ADPKD can present with a wide range of clinical conditions, reflecting the multisystem nature of the disorder. Renal function may remain normal for decades. However, once the glomerular filtration rate (GFR) begins to decline, renal impairment typically progresses rapidly, with an average GFR loss of 4.0 to 5.0 mL/minute/year. A thorough history and physical examination are crucial first steps in autosomal dominant polycystic kidney disease diagnosis.
Male sex, early onset of hypertension, PKD1 genotype, increased total kidney volume, and the presence of proteinuria are associated with worse prognostic outcomes. Total kidney volume is a primary predictive biomarker for future GFR loss. Risk stratification is essential after autosomal dominant polycystic kidney disease diagnosis to guide management.
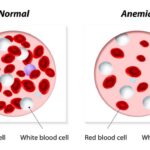
The most common clinical presentations of ADPKD include hypertension, anemia, liver cysts, hematuria, flank pain, palpable abdominal masses, urinary tract infections, renal failure, nephrolithiasis, and renal cancers. Recognizing these diverse clinical manifestations is vital for accurate autosomal dominant polycystic kidney disease diagnosis.
Hypertension is the most universal and often the earliest clinical presentation in ADPKD patients. Microalbuminuria, proteinuria, and hematuria are also more prevalent in patients with hypertension and ADPKD. Episodes of acute flank pain are frequently observed due to cyst bleeding, infection, stones, and, less commonly, tumors. These common symptoms often prompt the initial investigation leading to autosomal dominant polycystic kidney disease diagnosis.
Gross (visible) hematuria may be the initial presenting symptom. Cyst hemorrhage is a frequent complication, causing gross hematuria when the cyst communicates with the collecting system. It can also manifest with fever, raising suspicion of cyst infection. Occasionally, a hemorrhagic cyst may rupture, leading to a retroperitoneal bleed. These acute presentations can necessitate urgent autosomal dominant polycystic kidney disease diagnosis and management.
Urinary tract infections (UTIs) are common in ADPKD, including cystitis, acute pyelonephritis, cyst infection, and perinephric abscesses. Escherichia coli, Klebsiella, Proteus species, and other Enterobacteriaceae are the most frequently identified infectious agents. Recurrent UTIs in the context of cystic kidney disease should raise suspicion for ADPKD and prompt further investigation towards autosomal dominant polycystic kidney disease diagnosis.
Renal stone disease occurs in approximately 20% to 25% of patients with ADPKD. Most stones are composed of uric acid, calcium oxalate, or both. This is attributed to lower urinary volumes, intrarenal stasis due to anatomical obstruction, hypocitraturia, and low urinary magnesium levels. Renal calculi can be challenging to diagnose on imaging in ADPKD patients due to calcifications in the renal parenchyma and cyst walls. Unenhanced CT scans of the abdomen and pelvis are most helpful for diagnosing nephrolithiasis in ADPKD patients. Renal stones are a significant comorbidity that may be identified during autosomal dominant polycystic kidney disease diagnosis and management.
The prevalence of hepatic cysts increases with age. Polycystic liver disease should be suspected when four or more cysts are present in the hepatic parenchyma. Patients may remain asymptomatic or present with liver impairment or pain due to infection or cyst rupture. About 7% to 36% of patients also have pancreatic cysts, which are more common with PKD2 mutations than with PKD1. Extrarenal cysts, particularly liver cysts, often support autosomal dominant polycystic kidney disease diagnosis.
Mitral valve prolapse and aortic regurgitation are the most common cardiovascular abnormalities associated with ADPKD. It is also linked to increased coronary aneurysms, asymptomatic pericardial effusions, congenital heart malformations, aortic valve stenosis, and atrial fibrillation. Gastrointestinal abnormalities are also common; up to 50% of patients with ADPKD will also have diverticulosis. These systemic associations are important to consider in the comprehensive autosomal dominant polycystic kidney disease diagnosis and management.
Although children with ADPKD generally do not have renal impairment (unlike ARPKD), they exhibit higher rates of hypertension and proteinuria compared to children without ADPKD, requiring close monitoring and treatment. Early-onset hypertension in children with a family history of cystic kidney disease is a significant indicator for autosomal dominant polycystic kidney disease diagnosis.
It’s also suggested that in children, the incidence of early-onset ADPKD is similar to ARPKD, making differentiation between these two disorders challenging. Differential autosomal dominant polycystic kidney disease diagnosis from ARPKD is particularly important in pediatric cases.
Evaluation
The autosomal dominant polycystic kidney disease diagnosis is typically made through a combination of factors: a positive family history, imaging studies such as ultrasonography and/or CT scans, and clinical findings like hypertension and/or renal failure. The disorder should also be considered in patients presenting with renal impairment associated with multiple bilateral cysts on renal imaging (CT or renal ultrasound), regardless of family history of ADPKD.
Ultrasound is often sufficient for asymptomatic patients with normal renal function in autosomal dominant polycystic kidney disease diagnosis. In children, if initial ultrasound findings are negative for kidney cysts, follow-up ultrasounds should be deferred until adolescence (between ages 15 and 18). Ultrasound is a common initial imaging modality in autosomal dominant polycystic kidney disease diagnosis.
CT or MRI can be used to estimate height-adjusted total kidney volume for risk stratification of disease progression and can be beneficial for management planning after autosomal dominant polycystic kidney disease diagnosis.
In patients with a strong family history and palpable kidneys, a baseline CT or MRI can be helpful in managing potential future complications, tracking disease progression, and early detection of nephrolithiasis. Advanced imaging modalities like CT and MRI play a crucial role in comprehensive autosomal dominant polycystic kidney disease diagnosis and monitoring.
The Renal Association Clinical Practice Guidelines recommend educating parents or caregivers of individuals with ADPKD about the risk of inheritance. Blood pressure screening every two years is advised for at-risk children older than two years and young adults. Genetic counseling and family screening are important components of autosomal dominant polycystic kidney disease diagnosis and management in families with known ADPKD.
Genetic testing for autosomal dominant polycystic kidney disease diagnosis can be performed using direct DNA sequencing or DNA gene linkage analysis (requiring samples from at least three family members, including those with and without ADPKD). Genetic testing boasts a 99% accuracy rate for both PKD1 and PKD2 genes and is commercially available. Genetic testing provides a definitive autosomal dominant polycystic kidney disease diagnosis and can be particularly useful in specific scenarios.
The primary indication for genetic testing is in young adults with negative ultrasonographic findings but a family history suggestive of ADPKD, particularly when considering kidney donation, family planning, or pregnancy. Genetic testing is valuable in confirming autosomal dominant polycystic kidney disease diagnosis in ambiguous cases.
Genetic testing for ADPKD is not routinely performed or required for autosomal dominant polycystic kidney disease diagnosis or management in most cases. However, it can be useful for prognosis, diagnostic confirmation, estimating disease progression, and family planning. While not always necessary, genetic testing enhances the precision of autosomal dominant polycystic kidney disease diagnosis and risk assessment.
Genetic testing may also be employed to confirm an ADPKD diagnosis when clinical factors and imaging are inconclusive. In complex presentations, genetic testing can provide definitive confirmation of autosomal dominant polycystic kidney disease diagnosis.
The decision to pursue genetic testing or renal ultrasonography for asymptomatic children should be a collaborative one, involving caretakers, parents, and healthcare professionals. Ethical considerations and shared decision-making are important in autosomal dominant polycystic kidney disease diagnosis in children.
Ultrasound Criteria for ADPKD: Original Ravine PKD1 Diagnostic Criteria
- Ages 15 to 29 years: 2 or more cysts, unilateral or bilateral.
- Ages 30 to 59 years: 2 or more cysts in each kidney.
- Ages 60 years or older: 4 or more cysts in each kidney.
These criteria are also used for diagnosing PKD2 but are less accurate. Two notable characteristics of these criteria are:
- Three or more total cysts in individuals aged 15 to 39 years have a positive predictive value of 100%.
- Two or fewer cysts in individuals older than 40 years have a negative predictive value of 100%.
These ultrasound criteria are fundamental in establishing autosomal dominant polycystic kidney disease diagnosis using imaging.
Autosomal Dominant vs Autosomal Recessive Polycystic Kidney Disease
Distinguishing between ADPKD and ARPKD is crucial in autosomal dominant polycystic kidney disease diagnosis. Key differences include:
Autosomal Dominant Polycystic Kidney Disease:
- Symptoms typically onset at age 30 or later.
- Incidence of 1:400 – 1:1,000 (relatively common).
- Hepatic cysts may develop but generally do not lead to significant liver disease or failure.
- Strong family history is common due to dominant inheritance.
- Average life expectancy ranges from roughly 53 to 70 years.
- ESKD typically develops in the 60s.
Autosomal Recessive Polycystic Kidney Disease:
- Symptoms usually begin at birth or shortly thereafter.
- Incidence of 1:20,000 – 1:40,000 (relatively rare).
- Hepatic cysts develop early and can be seen prenatally. Liver disease is significant and may progress to cirrhosis.
- Usually no family history of this disease as it is inherited recessively.
- High mortality in newborns (20% within the first month), but those surviving the newborn period have a 90% chance of living to at least 20 years.
- ESKD develops in 50% of patients reaching 20 years of age.
These comparative features aid in the differential autosomal dominant polycystic kidney disease diagnosis from ARPKD.
Abdominal CT scan revealing polycystic kidneys and liver cysts in ADPKD patient, coronal view.
Treatment / Management
The Mayo classification system (classes 1A, 1B, 1C, 1D, and 1E) categorizes ADPKD risk from lowest to highest for adverse disease outcomes. Total kidney volume is considered the most useful and diagnostic criterion. Risk stratification using tools like the Mayo classification is important for guiding management after autosomal dominant polycystic kidney disease diagnosis.
The latter three stages of the Mayo classification are associated with a higher risk of ESKD. These criteria help identify high-risk patients who would benefit from more aggressive management strategies following autosomal dominant polycystic kidney disease diagnosis.
Lifestyle and Dietary Modifications are recommended, although their definitive impact on preventing ADPKD progression is not fully established. Patients are often advised to drink three liters of fluids daily to suppress vasopressin, thereby reducing cAMP production and inhibiting cyst production. Lifestyle modifications are a key component of long-term management after autosomal dominant polycystic kidney disease diagnosis.
All ADPKD patients are generally advised to limit sodium intake to less than 2 grams per day. The CRISP study demonstrated a positive correlation between the increase in total kidney volume and 24-hour urine sodium excretion. Restricted sodium intake can also improve blood pressure control, which is crucial in managing ADPKD after autosomal dominant polycystic kidney disease diagnosis.
Flank pain in ADPKD patients requires exclusion of other potential causes such as infection, stones, herpes zoster, and neoplasms. Tricyclic antidepressants can be beneficial for chronic pain management, similar to their use in other chronic pain syndromes, and are generally well-tolerated. Cyst aspiration, guided by ultrasound or CT, may be considered if pain is likely due to distortion of the kidney by a large cyst. For pain attributed to multiple cysts, laparoscopic or surgical cyst fenestration or unroofing may be beneficial. Pain management strategies are an important aspect of care following autosomal dominant polycystic kidney disease diagnosis.
Cyst hemorrhage episodes are typically self-limiting. Patients often respond well to conservative management including bed rest, analgesics, and increased fluid intake to prevent clot formation and obstruction of the upper urinary tract. In rare cases, bleeding may be severe, leading to hemodynamic instability, necessitating hospitalization, transfusions, and supportive care. Management of complications like cyst hemorrhage is essential after autosomal dominant polycystic kidney disease diagnosis.
Cyst and urinary tract infections require prompt treatment to prevent retrograde seeding of the renal parenchyma. Antibiotics with good cyst penetration are preferred, including trimethoprim-sulfamethoxazole, ertapenem, chloramphenicol, fluoroquinolones, sulfamethoxazole/trimethoprim, and clindamycin. If fever persists after 1 to 2 weeks of appropriate antimicrobial therapy, percutaneous or surgical drainage of infected cysts should be considered. In cases of end-stage polycystic kidneys, nephrectomy may be necessary. Effective management of infections is crucial in ADPKD patients following autosomal dominant polycystic kidney disease diagnosis.
Nephrolithiasis is more prevalent in ADPKD patients than in the general population. ADPKD patients are predisposed to forming uric acid stones (most common), followed by calcium oxalate urinary calculi. Symptomatic stones are managed similarly to other patients, but urinary alkalinization therapy is suggested whenever possible due to the prevalence of uric acid stones. Potassium citrate and increased oral fluid intake are generally preferred treatments for stone-forming conditions associated with ADPKD, particularly in cases of distal acidification disorders, low urinary volumes, and aciduria. 24-hour urine testing is recommended to identify specific risk factors in ADPKD patients with or at risk for urolithiasis. Management of nephrolithiasis is a common aspect of ADPKD care after autosomal dominant polycystic kidney disease diagnosis.
Management of hypertension is vital for reducing cardiovascular mortality and slowing renal failure progression in ADPKD. The HALT-PKD study suggests a target blood pressure range of less than 120 to 125/80 mm Hg, similar to other patients with chronic kidney disease. In patients with preserved or nearly preserved GFR, a lower blood pressure goal of less than 110/75 mm Hg is associated with a decreased incidence of cardiovascular events and a slower rate of cyst growth. Angiotensin inhibitors are the preferred first-line agents if not contraindicated. ACE inhibitors also protect glomeruli by reducing intraglomerular pressure and slowing GFR decline in those with proteinuria. Beta-blockers and calcium-channel blockers are second-line treatments. Thiazide diuretics are preferred as a third-line treatment in patients with normal renal function and hypercalciuria, while loop diuretics are recommended in patients with impaired renal function as an alternative to thiazides. Aggressive blood pressure management is a cornerstone of ADPKD treatment after autosomal dominant polycystic kidney disease diagnosis.
Tolvaptan is an FDA-approved medication that slows the progression of autosomal dominant polycystic kidney disease by blocking vasopressin V2 receptors, reducing intracellular cyclic AMP levels that stimulate cystic proliferation and growth. It is indicated for ADPKD patients at high risk of rapid disease progression. However, due to its high cost and potential adverse effects, including liver toxicity, its use is generally reserved for patients at high risk of disease progression or those with rapidly declining kidney function. Tolvaptan represents a targeted therapeutic option for slowing disease progression after autosomal dominant polycystic kidney disease diagnosis in selected patients.
Current guidelines for tolvaptan use consider total kidney volume, which precedes GFR decline, in addition to historical GFR decline. Tolvaptan is often favored for patients 55 years or younger with rapidly declining GFR and fewer comorbidities, although there is no definitive age cutoff. Patient selection for tolvaptan therapy is a critical aspect of management following autosomal dominant polycystic kidney disease diagnosis.
A current guideline for tolvaptan use is a yearly GFR decline of ≥3.0 mL/min primarily attributed to ADPKD, estimated from at least five measurements over four years. Factors suggesting GFR decline might be due to causes other than ADPKD include known vascular disease, uncontrolled hypertension, diabetes mellitus, and severe proteinuria (>1 g/d). Tolvaptan has not been studied in patients younger than 18. Careful assessment of GFR decline and other comorbidities is necessary to determine the appropriateness of tolvaptan therapy after autosomal dominant polycystic kidney disease diagnosis.
The TEMPO and REPRISE trials demonstrated the efficacy of tolvaptan in preventing GFR decline in ADPKD. However, tolvaptan carries a black box warning due to potential liver failure. Baseline and regular monitoring of liver function tests (AST, ALT, and bilirubin) is mandatory. Due to liver injury risks, tolvaptan is available only through a restricted distribution protocol under an FDA-approved REMS program. Tolvaptan is contraindicated in patients taking CYP3A4 inhibitors. Common adverse effects include increased thirst, polyuria, nocturia, polydipsia, and hypernatremia, which can lead to drug discontinuation. Liver function monitoring and management of side effects are crucial considerations when using tolvaptan after autosomal dominant polycystic kidney disease diagnosis.
Statins are frequently used in chronic kidney disease patients due to the equivalent cardiovascular risk of renal failure to coronary heart disease. However, evidence regarding statins slowing ADPKD progression is conflicting. The role of statins in directly modifying ADPKD progression after autosomal dominant polycystic kidney disease diagnosis remains under investigation.
Mammalian targets of rapamycin (mTOR) inhibitors, sirolimus and everolimus, have been studied in ADPKD but have not shown benefit on renal outcomes. Significant adverse effects also limit their use. Currently, mTOR inhibitors are not recommended for routine use in ADPKD management after autosomal dominant polycystic kidney disease diagnosis.
Somatostatin and somatostatin analogs such as octreotide, lanreotide, and pasireotide have not been shown to affect ADPKD disease progression. Somatostatin analogs are not considered effective treatments for ADPKD following autosomal dominant polycystic kidney disease diagnosis.
Nephrectomy is indicated in ADPKD patients for unbearable abdominal discomfort, anorexia, renal cell carcinoma, renal hemorrhage, kidney infection with gas-forming agents, and staghorn calculi in nonfunctioning kidneys with persistent UTIs. Nephrectomy for large, cystic kidneys can be considered in ESKD patients if symptomatic or to increase abdominal capacity for future renal transplant. Nephrectomy remains a potential surgical option for specific complications in advanced ADPKD after autosomal dominant polycystic kidney disease diagnosis.
ADPKD with ESKD necessitates hemodialysis, renal transplantation, or peritoneal dialysis. Survival rates for ADPKD patients on hemodialysis are generally higher (10%-15% mortality at 5 years) than for patients on hemodialysis due to other causes, possibly due to lower rates of coronary artery disease in this population. Renal replacement therapy is the ultimate management for ESKD resulting from ADPKD after autosomal dominant polycystic kidney disease diagnosis.
Treatments on the Horizon
Several potential future treatments for ADPKD are currently under investigation.
-
Transepithelial chloride secretion, mediated by CFTR, is a key mechanism in cystogenesis. CFTR inhibitors are being studied for their potential to inhibit cyst formation in ADPKD, but current studies are preclinical.
-
Curcumin, derived from turmeric, activates antioxidant transcription, reduces inflammation, and suppresses cell proliferation. It is being researched for various diseases, and its potential positive effects on reducing cell growth and improving arterial function in ADPKD are under investigation.
These emerging therapies offer potential future advancements in ADPKD management following autosomal dominant polycystic kidney disease diagnosis.
Differential Diagnosis
Renal cysts can be observed in other systemic diseases, necessitating differential autosomal dominant polycystic kidney disease diagnosis.
Bardet-Biedl syndrome is a complex genetic disorder characterized by various symptoms, including vision problems, obesity, and kidney abnormalities. Renal cysts can be a renal manifestation but are not the defining feature.
HNF1B mutations can cause renal cysts, often associated with other systemic disorders such as early-onset diabetes, early-onset gout, pancreatic hypoplasia, abnormal liver function, and genital tract malformations.
Medullary sponge kidney disease is a rare congenital disorder (1:5,000 individuals) that can lead to small cysts or renal collecting tubule dilatations. While it can cause renal cyst-like structures, it does not progress to renal failure but is highly associated with nephrocalcinosis and nephrolithiasis, often due to hypocitraturia and hypercalciuria. It is also associated with a higher incidence of UTIs.
Orofaciodigital syndrome type I is a genetic disorder characterized by abnormalities in the face, oral cavity, and digits. Kidney abnormalities, including cysts, can occur but are not typically the primary diagnostic criterion.
Renal cysts can be seen in tuberous sclerosis, but this condition is usually associated with characteristic skin lesions, facial angiofibroma, connective tissue nevi, and cardiac, renal, and pulmonary manifestations.
Conditions in the differential diagnosis of ADPKD include:
- Autosomal dominant tubulointerstitial nephropathy
- Autosomal recessive polycystic kidney disease
- Bardet-Biedl syndrome
- HANAC syndrome
- HNF1B mutations
- Medullary sponge kidney
- Multiple simple renal cysts
- Orofaciodigital syndrome type I
- Parapelvic renal cysts
- Renal spongiosis
- Tuberous sclerosis
- Von Hippel-Lindau syndrome
A thorough clinical evaluation and appropriate investigations are essential for accurate differential autosomal dominant polycystic kidney disease diagnosis.
Prognosis
The prognosis of ADPKD varies, but approximately 50% to possibly 75% of patients will develop ESKD by the age of 70. Understanding the typical disease course is important for patient counseling after autosomal dominant polycystic kidney disease diagnosis.
A Canadian study reported that 25% of ADPKD patients had ESKD by age 47, 50% by age 59, and 75% by age 70. A French study showed that 22% of patients had ESKD by age 50, 42% by age 58, and 72% by age 73. These studies highlight the progressive nature of ADPKD and the likelihood of ESKD development. Prognostic data helps in long-term planning following autosomal dominant polycystic kidney disease diagnosis.
Overall life expectancy for patients with ADPKD is between 53 to 70 years. While ADPKD significantly impacts renal health, life expectancy can be influenced by management and comorbidities after autosomal dominant polycystic kidney disease diagnosis.
Complications
-
End-stage kidney disease requiring dialysis or renal transplantation is the most frequent and severe complication of ADPKD.
-
Modifiable risk factors such as smoking, hypertension, and excessive alcohol intake can worsen disease progression.
-
ADPKD is often associated with diverticular disease, nephrolithiasis, and abdominal wall or inguinal hernias.
Recognizing and managing these potential complications is a crucial aspect of long-term care after autosomal dominant polycystic kidney disease diagnosis.
Deterrence and Patient Education
Following autosomal dominant polycystic kidney disease diagnosis, regular follow-up with nephrologists is essential. Early diagnosis, risk assessment, appropriate pharmacotherapy, and proper management of nephrolithiasis risk factors, urinary citrate levels, hypertension, and proteinuria can help slow disease progression.
Lifestyle modifications such as increased oral water intake, restricted salt intake, and avoidance of NSAIDs are associated with long-term benefits. Patient education plays a vital role in empowering individuals to actively participate in managing their ADPKD after autosomal dominant polycystic kidney disease diagnosis.
Enhancing Healthcare Team Outcomes
Autosomal dominant polycystic kidney disease, being a systemic disorder affecting multiple organs, necessitates a multidisciplinary management approach. A collaborative team including a nephrologist, urologist, interventional radiologist, cardiologist, social worker, and dialysis nurse is essential for providing comprehensive care. Effective teamwork is crucial for optimal patient outcomes following autosomal dominant polycystic kidney disease diagnosis.
Patients must be educated on the importance of optimal blood pressure control and regular blood testing to monitor renal function. They also need to be informed about potential complications, including cerebral aneurysms, hypertension, kidney stones, and end-stage kidney disease. Comprehensive patient education and coordinated care are key to improving quality of life and outcomes after autosomal dominant polycystic kidney disease diagnosis.
Risk prediction scores, such as the PRO-PKD score, can aid in predicting ADPKD prognosis. Optimal management of blood pressure is crucial as uncontrolled hypertension accelerates renal function decline. Effective pain control and early treatment of cyst or urinary tract infections can improve the quality of life for ADPKD patients. Education of patients and families about the condition can also reduce hospitalizations. Prognostic tools and proactive management strategies are important for optimizing patient care after autosomal dominant polycystic kidney disease diagnosis.
Review Questions
Polycystic kidney ultrasound showing multiple cysts characteristic of ADPKD.
Gross pathology of autosomal dominant polycystic kidney disease showing extensive cyst formation.
References
[List of references as in the original article]
Disclosure: (As in original article)