Acute Zonal Occult Outer Retinopathy (AZOOR) presents a unique diagnostic challenge in ophthalmology. This rare condition, believed to be autoimmune in nature, affects the outer retina and can lead to sudden visual disturbances. While the exact cause remains unknown, prompt and accurate diagnosis is crucial for patient management and understanding the progression of this enigmatic disease. This article delves into the intricacies of Azoor Diagnosis, offering a detailed overview for both patients experiencing symptoms and eye care professionals seeking to refine their diagnostic approach.
Recognizing the Symptoms: The First Step Towards AZOOR Diagnosis
Patients often describe the onset of AZOOR symptoms as sudden and unsettling. A key indicator is the appearance of scotoma, described as blind spots or areas of blurred vision in the visual field. This visual loss is frequently accompanied by photopsia, the perception of flashing or shimmering lights, even when no external light source is present. It’s important to note that while visual disturbances like floaters are common and often benign, the combination of sudden scotoma and photopsia should raise suspicion for conditions like AZOOR, prompting further investigation. Interestingly, some individuals report experiencing a viral-like illness in the weeks preceding the onset of these visual symptoms, suggesting a possible trigger, although this link is still under investigation. Typically, AZOOR initially affects one eye, but it’s not uncommon for the other eye to become involved subsequently.
Who is at Risk for AZOOR and When Does it Occur?
AZOOR exhibits a predilection for certain demographics. It is significantly more prevalent in women, affecting them almost three times as often as men. Myopia, or nearsightedness, is also frequently observed in patients diagnosed with AZOOR. The average age of diagnosis falls in the 30s, but AZOOR can affect individuals across a broader age range, from younger patients to older adults. Furthermore, Caucasians appear to be more commonly affected compared to other ethnic groups. Understanding these demographic trends can aid clinicians in risk assessment and considering AZOOR in the differential diagnosis for patients presenting with relevant symptoms.
The Diagnostic Process: Unraveling the Occult Nature of AZOOR
One of the defining characteristics of AZOOR, and what makes its diagnosis challenging, is its “occult” nature. During a standard eye examination, the retina may often appear remarkably normal, especially in the early stages. This is because the photoreceptor damage, while functionally significant, may not immediately manifest with obvious structural changes visible through traditional ophthalmoscopy. Therefore, diagnosing AZOOR requires a multi-faceted approach, combining careful clinical observation with specialized diagnostic testing.
Clinical Examination: Identifying Subtle Clues
While a routine eye exam might not reveal dramatic abnormalities in AZOOR, a meticulous ophthalmologist will look for subtle signs. These can include initial, delicate changes in the retinal pigment epithelium (RPE), the supportive layer behind the photoreceptors. In some cases, more pronounced RPE abnormalities or alterations in the retinal blood vessels in the affected zone may become apparent over time. Pigmentary changes around the optic nerve head and, less frequently, inflammatory cells in the vitreous humor (the gel-like substance filling the eye) can also be observed. These subtle clinical findings, although not definitive on their own, contribute to the overall diagnostic picture when considered alongside patient symptoms and other test results.
Visual Field Testing: Mapping the Functional Deficit
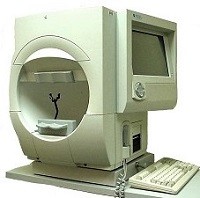
Visual field testing is a cornerstone in the diagnostic workup for AZOOR. This test objectively measures the extent of peripheral vision and identifies any areas of visual loss. The Humphrey Field Analyzer is the most commonly used instrument for this purpose. During the test, the patient fixates on a central point while small flashes of light are presented in their peripheral vision. By recording which flashes the patient perceives, a detailed map of their visual field is created. In AZOOR, visual field testing typically reveals characteristic defects, predominantly in the peripheral visual field, reflecting the “zonal” nature of photoreceptor damage. These visual field defects are crucial evidence supporting the diagnosis, especially in cases where the retinal appearance is largely normal.
 the Humphrey Field Analyzer
the Humphrey Field Analyzer
Image: Humphrey Field Analyzer used for visual field testing in diagnosing AZOOR, illustrating the bowl-shaped perimeter and patient positioning.
Optical Coherence Tomography (OCT): Visualizing Photoreceptor Degeneration
Optical coherence tomography (OCT) is an advanced imaging technique that provides cross-sectional views of the retina, allowing visualization of individual retinal layers. OCT has become an indispensable tool in AZOOR diagnosis. In patients with AZOOR, OCT scans can reveal zones of outer retinal and photoreceptor layer degeneration, even when these changes are not readily apparent on clinical examination. Specifically, thinning or disruption of the outer retinal layers, including the photoreceptor inner and outer segments, is a hallmark finding in AZOOR. OCT not only aids in confirming the diagnosis but also helps in monitoring disease progression and assessing the extent of retinal damage.
Fundus Autofluorescence (FAF): Detecting RPE Abnormalities
Fundus autofluorescence (FAF) is another valuable imaging modality in AZOOR diagnosis. FAF captures the natural fluorescence emitted by lipofuscin, a metabolic byproduct that accumulates in the RPE cells. Damaged or dysfunctional RPE cells, as seen in AZOOR, often exhibit abnormal autofluorescence patterns. In AZOOR, FAF imaging may reveal areas of altered autofluorescence corresponding to the zones of photoreceptor loss. These abnormalities can manifest as either increased (hyperautofluorescence) or decreased (hypoautofluorescence) signal, depending on the stage and nature of RPE involvement. FAF provides complementary information to OCT and visual field testing, further strengthening the diagnostic confidence in AZOOR.
Angiography: Ruling Out Other Conditions
While less specific for AZOOR itself, angiography, including fluorescein angiography (FA) and indocyanine green angiography (ICGA), may be used in certain cases to rule out other retinal conditions that can mimic AZOOR or to further characterize the retinal changes. These techniques involve injecting dyes into the bloodstream and imaging the retinal blood vessels. In AZOOR, angiography findings are often subtle or non-specific, which can be helpful in differentiating it from conditions with prominent vascular abnormalities. However, angiography is not routinely required for AZOOR diagnosis and is typically reserved for cases with atypical presentations or when considering alternative diagnoses.
Differential Diagnosis: Distinguishing AZOOR from Mimickers
It is essential to consider other conditions that can present with similar symptoms to AZOOR. These include:
- Multiple Evanescent White Dot Syndrome (MEWDS): Another inflammatory condition affecting the outer retina, often presenting with photopsia and scotoma. MEWDS typically has a more benign and self-limiting course than AZOOR.
- Acute Retinal Pigment Epitheliitis (ARPE): Characterized by dark spots in the vision and RPE lesions. ARPE usually has a better visual prognosis compared to AZOOR.
- Idiopathic Blind Spot Enlargement Syndrome (IBSE): Presents with an enlarged blind spot and can have overlapping features with AZOOR.
- Retinal Dystrophies: Certain inherited retinal conditions can mimic AZOOR, particularly in atypical or late-onset presentations.
Careful clinical evaluation, detailed history taking, and comprehensive diagnostic testing are crucial to differentiate AZOOR from these and other potential mimickers.
The Importance of Early and Accurate AZOOR Diagnosis
While there is currently no proven cure for AZOOR, accurate and timely diagnosis is paramount for several reasons. Firstly, it allows for appropriate patient counseling and management of expectations regarding the disease course and visual prognosis. While visual acuity is often preserved, patients need to be aware of the potential for persistent visual field defects and the possibility of disease progression or recurrence in some cases. Secondly, establishing a diagnosis of AZOOR helps to rule out other, potentially treatable conditions. Finally, early diagnosis facilitates enrollment in clinical trials and research studies aimed at better understanding AZOOR and developing effective therapies.
Conclusion: Navigating the Diagnostic Landscape of AZOOR
Diagnosing AZOOR requires a thorough and systematic approach. Recognizing the characteristic symptoms of sudden scotoma and photopsia, particularly in at-risk individuals, is the initial step. Comprehensive ophthalmic examination combined with specialized tests such as visual field testing, OCT, and FAF are essential for confirming the diagnosis and excluding other conditions. While AZOOR remains a complex and somewhat enigmatic disease, advancements in diagnostic technologies continue to improve our ability to identify and manage this condition effectively, ultimately benefiting patients experiencing vision loss from this rare retinopathy. Consultation with a retina specialist experienced in inflammatory and retinal disorders is highly recommended for anyone suspecting they may have AZOOR.