Introduction
Vitamin B12, scientifically known as cobalamin, is an essential water-soluble vitamin vital for numerous bodily functions. Primarily sourced from animal products like meat, dairy, and eggs, B12 plays a critical role in DNA synthesis, fatty acid metabolism, and the formation of myelin, the protective sheath around nerve fibers. The absorption of vitamin B12 is a complex process, requiring intrinsic factor, a glycoprotein produced by parietal cells in the stomach. This factor binds to B12 and facilitates its uptake in the terminal ileum, the final section of the small intestine. A deficiency in vitamin B12 can disrupt these essential processes, leading to a spectrum of hematologic and neurological complications. While the liver stores substantial reserves of B12, prolonged insufficient absorption, whether due to dietary inadequacy, malabsorption issues, or a lack of intrinsic factor, can deplete these stores and result in deficiency. Therefore, accurate B12 Diagnosis is crucial for timely intervention and management to prevent severe health consequences. This article aims to provide a comprehensive guide to vitamin B12 deficiency, emphasizing its diagnosis, management, and the collaborative role of healthcare professionals in optimizing patient care.
Etiology of Vitamin B12 Deficiency
Vitamin B12 deficiency arises from a variety of causes, broadly categorized into four primary etiologies:
-
Autoimmune Conditions: Pernicious anemia, a prominent autoimmune disorder, is characterized by the body’s immune system mistakenly attacking parietal cells in the stomach or intrinsic factor itself. This autoimmune reaction leads to the production of antibodies against intrinsic factor, which are known as anti-intrinsic factor antibodies. These antibodies interfere with the binding of intrinsic factor to vitamin B12, thereby hindering B12 absorption in the terminal ileum. Consequently, pernicious anemia is a significant cause of B12 deficiency due to impaired intrinsic factor function.
-
Malabsorption Syndromes: Malabsorption is a critical factor in B12 deficiency. Since intrinsic factor is produced by parietal cells in the stomach, any surgical procedures that bypass or remove parts of the stomach, such as gastric bypass surgery, can significantly reduce intrinsic factor production. This reduction impairs B12 absorption. Similarly, conditions affecting the terminal ileum, the primary site of B12 absorption, can also lead to deficiency. Surgical resection of the terminal ileum, often performed in cases of Crohn’s disease, directly reduces the absorptive surface for B12. Other intestinal conditions, such as celiac disease-induced inflammation or infections like Diphyllobothrium latum (fish tapeworm) infestation, can damage the small intestinal lining and disrupt B12 absorption.
-
Dietary Insufficiency: While the liver maintains substantial B12 reserves, dietary inadequacy over an extended period can deplete these stores. Strict vegan diets, which exclude all animal products, are a primary dietary cause of B12 deficiency. Vitamin B12 is naturally found in animal-derived foods; therefore, individuals adhering to vegan diets for approximately three years or more without B12 supplementation are at high risk of developing a deficiency.
-
Exposure to Toxins and Medications: Certain substances and medications can interfere with vitamin B12 absorption or metabolism. Nitrous oxide, commonly used in anesthesia and recreational settings, can inactivate vitamin B12, leading to deficiency and neurological symptoms. Metformin, a widely prescribed medication for type 2 diabetes, has also been associated with B12 deficiency. The exact mechanism is not fully understood but may involve altered intestinal motility or bacterial overgrowth affecting B12 absorption. Prolonged use of proton pump inhibitors (PPIs), which reduce stomach acid, can also impair B12 absorption by affecting the release of B12 from food proteins and the binding of B12 to intrinsic factor.
Understanding these diverse etiologies is crucial for accurate b12 diagnosis and targeted management strategies.
Epidemiology of Vitamin B12 Deficiency
The prevalence of vitamin B12 deficiency is variable and significantly influenced by the underlying cause, age group, and geographic location. In the general population, studies examining anemia have indicated that B12 deficiency accounts for approximately 1% to 2% of anemia cases. However, among individuals exhibiting macrocytosis, an abnormal enlargement of red blood cells (defined by a mean corpuscular volume, MCV, >100 fL), B12 deficiency is a more prominent factor, contributing to 18% to 20% of cases.
Age is a significant demographic factor in B12 deficiency. Older adults are disproportionately affected, regardless of the underlying etiology. This increased susceptibility in the elderly may be attributed to factors such as age-related atrophic gastritis (reducing intrinsic factor production), decreased dietary intake, and malabsorption issues.
Pernicious anemia, a specific cause of B12 deficiency, exhibits notable ethnic and geographic variations. It is more frequently observed in individuals of Northern European descent. Conversely, the incidence of pernicious anemia is lower in populations of African descent and those originating from other regions of Europe. These epidemiological patterns highlight the complex interplay of genetic, environmental, and dietary factors in the global distribution of vitamin B12 deficiency. Effective b12 diagnosis strategies need to consider these epidemiological factors to target at-risk populations for screening and intervention.
Pathophysiology of Vitamin B12 Deficiency
The intricate pathophysiology of vitamin B12 deficiency involves disruptions in several key metabolic pathways, impacting both hematologic and neurologic functions. In healthy individuals, dietary vitamin B12 initially binds to R-factor, a protein secreted by salivary glands. This complex traverses to the small intestine, where pancreatic enzymes cleave B12 from R-factor. Subsequently, B12 binds to intrinsic factor, a glycoprotein produced by gastric parietal cells. The B12-intrinsic factor complex then attaches to specific receptors in the terminal ileum, facilitating B12 absorption into the bloodstream.
Once absorbed, vitamin B12 functions as a crucial cofactor for two primary enzymes:
-
Methionine Synthase: B12 is essential for methionine synthase, which catalyzes the conversion of homocysteine to methionine. This reaction is critical for the synthesis of S-adenosylmethionine (SAMe), a universal methyl donor involved in numerous biochemical reactions, including DNA methylation and neurotransmitter synthesis. A byproduct of this reaction is the conversion of methyltetrahydrofolate (methyl-THF) to tetrahydrofolate (THF). THF is a vital coenzyme in the synthesis of pyrimidine and purine bases, the building blocks of DNA. In B12 deficiency, the impaired conversion of homocysteine to methionine leads to an accumulation of homocysteine and a deficiency of THF. Consequently, DNA synthesis is compromised, particularly in rapidly dividing cells like those in the bone marrow, leading to megaloblastic anemia. This anemia is characterized by fatigue and pallor, common symptoms of B12 deficiency. The impaired DNA synthesis also affects other rapidly proliferating cell lines, such as polymorphonuclear leukocytes (PMNs), resulting in the formation of hypersegmented neutrophils, a hallmark of B12 deficiency identifiable on peripheral blood smears.
-
Methylmalonyl-CoA Mutase: Vitamin B12 also serves as a cofactor for methylmalonyl-CoA mutase, an enzyme that converts methylmalonyl-CoA to succinyl-CoA, an important intermediate in the citric acid cycle (Krebs cycle) for energy production. In B12 deficiency, the impaired activity of methylmalonyl-CoA mutase results in the accumulation of methylmalonic acid (MMA). Elevated MMA levels, along with elevated homocysteine levels, are hypothesized to contribute to myelin damage, which underlies the neurological manifestations of B12 deficiency, such as neuropathy and ataxia. The myelin damage, particularly in the spinal cord, leads to a condition known as subacute combined degeneration of the spinal cord (SCDSC). SCDSC affects the dorsal columns (responsible for proprioception and vibration sense), lateral corticospinal tracts (motor pathways), and spinocerebellar tracts (coordination), resulting in symptoms like loss of proprioception, ataxia, peripheral neuropathy, and cognitive impairment, including dementia.
Understanding this detailed pathophysiology is fundamental for effective b12 diagnosis and for appreciating the diverse clinical manifestations of vitamin B12 deficiency.
History and Physical Examination in B12 Diagnosis
A comprehensive evaluation for suspected vitamin B12 deficiency necessitates a thorough history and physical examination, with particular attention to gastrointestinal (GI) and neurological systems. Given that B12 deficiency can manifest as macrocytic anemia, initial presenting symptoms often include signs of anemia, such as persistent fatigue and pallor. In severe cases, increased hemolysis due to ineffective red blood cell production may lead to jaundice, making a dermatological examination relevant. Patients may also report symptoms like peripheral neuropathy, glossitis (inflammation of the tongue), diarrhea, headaches, and neuropsychiatric disturbances, including mood changes or cognitive difficulties.
In taking a detailed GI history, it is crucial to inquire about pre-existing conditions such as celiac disease or Crohn’s disease, which can impair B12 absorption. A surgical history, especially gastrectomy or bowel resection, particularly of the ileum, significantly raises suspicion for B12 deficiency. Dietary history is also vital; a recent transition to a strict vegan diet increases the likelihood of dietary B12 deficiency.
Neurological manifestations can be subtle initially but progress in more severe cases. As previously mentioned, SCDSC is a serious neurological complication of B12 deficiency. A comprehensive neurological examination should assess for signs of dementia, peripheral neuropathy (sensory and motor deficits), ataxia (impaired coordination and balance), and loss of proprioception (awareness of body position). A mental status examination is also important to evaluate for neuropsychiatric changes.
Key components of the history and physical examination relevant to b12 diagnosis include:
- Symptoms of Anemia: Fatigue, weakness, pallor, shortness of breath, dizziness.
- Gastrointestinal Symptoms: Glossitis, diarrhea, constipation, nausea, loss of appetite, weight loss.
- Neurological Symptoms: Peripheral neuropathy (numbness, tingling, burning sensations in hands and feet), ataxia, muscle weakness, cognitive impairment, memory loss, mood changes, depression, psychosis.
- Dietary History: Vegan diet, vegetarian diet with limited dairy/egg intake, alcohol abuse (which can impair B12 absorption and nutritional status).
- Medical History: Pernicious anemia, atrophic gastritis, Crohn’s disease, celiac disease, gastric surgery (gastrectomy, gastric bypass, ileal resection), metformin use, proton pump inhibitor (PPI) use, nitrous oxide exposure.
- Physical Examination Findings: Pallor, jaundice, glossitis, tachycardia, signs of peripheral neuropathy (decreased vibration sense, proprioception, reflexes), gait abnormalities, cognitive impairment.
A meticulous history and physical exam, focusing on these key areas, is essential for prompting appropriate laboratory investigations and achieving accurate b12 diagnosis.
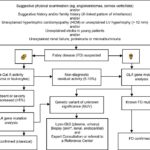
Evaluation and B12 Diagnosis
In patients suspected of vitamin B12 deficiency based on clinical presentation, initial laboratory investigations are essential for confirmation and differential diagnosis. These tests typically include:
-
Complete Blood Count (CBC) with Peripheral Smear: A CBC is a fundamental initial test. In B12 deficiency, it often reveals anemia, characterized by decreased hemoglobin and hematocrit levels. Macrocytic anemia, indicated by an elevated mean corpuscular volume (MCV) greater than 100 fL, is a hallmark finding, although not specific to B12 deficiency. The peripheral blood smear is crucial for identifying hypersegmented neutrophils, where a significant proportion of neutrophils exhibit five or more lobes in their nuclei. This finding is highly suggestive of B12 or folate deficiency.
-
Serum B12 and Folate Levels: Measuring serum B12 and folate levels is critical for differentiating between these two common causes of macrocytic anemia. A serum B12 level above 300 pg/mL is generally considered within the normal range. Levels between 200 and 300 pg/mL are in a borderline range, necessitating further enzymatic testing for definitive b12 diagnosis. Serum B12 levels below 200 pg/mL are indicative of deficiency. It is important to note that serum B12 levels alone may not always reflect tissue B12 status, and borderline levels can be misleading. Folate deficiency also presents with macrocytic anemia and can mimic B12 deficiency symptoms. Therefore, concurrent measurement of serum folate levels is essential for differential diagnosis.
-
Enzymatic Testing (Methylmalonic Acid and Homocysteine Levels): In cases where serum B12 levels are borderline (200-300 pg/mL) or when clinical suspicion for B12 deficiency remains high despite seemingly normal B12 levels, enzymatic testing is invaluable. B12 deficiency impairs the activity of methionine synthase and methylmalonyl-CoA mutase, leading to elevated serum levels of homocysteine and methylmalonic acid (MMA), respectively. Elevated levels of both MMA and homocysteine are highly sensitive and specific indicators of B12 deficiency, providing a more accurate b12 diagnosis compared to serum B12 alone, especially in early or mild deficiency. Importantly, in folate deficiency, only homocysteine levels are elevated, while MMA levels remain normal. This distinction is crucial for differentiating between B12 and folate deficiencies.
-
Further Investigations to Determine Etiology: Once B12 deficiency is confirmed, determining the underlying cause is essential for appropriate management. The clinical history, including surgical history (gastrectomy, ileal resection, gastric bypass), dietary history (veganism), and medication use (metformin, PPIs), can often point to the etiology. If the cause remains unclear after initial assessment, further investigations are warranted:
- Anti-Intrinsic Factor Antibody Test: If pernicious anemia is suspected (especially in cases of atrophic gastritis or in older patients), testing for anti-intrinsic factor antibodies is recommended. Positive antibodies strongly support the diagnosis of pernicious anemia, an autoimmune cause of B12 deficiency.
- Gastrointestinal Workup: In the absence of a clear dietary or surgical cause, gastrointestinal malabsorption should be investigated. This may include testing for celiac disease (celiac serology), Crohn’s disease (inflammatory markers, imaging, endoscopy), or bacterial overgrowth.
- Schilling Test (Historically): The Schilling test was historically used to diagnose pernicious anemia and assess B12 absorption. However, it is rarely performed now due to complexity and availability issues. It involved administering radiolabeled B12 orally and measuring its excretion in urine. Abnormal absorption patterns could differentiate between malabsorption and pernicious anemia. Modern diagnostic approaches largely rely on serum B12, MMA, homocysteine, and anti-intrinsic factor antibody testing.
A systematic approach to evaluation, combining clinical assessment with appropriate laboratory investigations, is crucial for accurate b12 diagnosis and effective management of vitamin B12 deficiency.
Treatment and Management of B12 Deficiency
Treatment strategies for vitamin B12 deficiency are primarily aimed at repleting B12 stores and addressing the underlying cause of the deficiency. The route and duration of treatment are tailored to the etiology and severity of the deficiency.
-
Oral B12 Supplementation: For patients with B12 deficiency due to dietary insufficiency, such as in strict vegans, oral B12 supplements are typically effective. High-dose oral B12 (1000-2000 mcg daily) can overcome absorption limitations even in individuals with impaired intrinsic factor production, as a small percentage of B12 can be absorbed through passive diffusion in the intestine when given in high doses. Oral supplementation is convenient and well-tolerated for maintenance therapy in dietary deficiency.
-
Parenteral B12 Administration (Intramuscular or Subcutaneous Injection): In cases of B12 deficiency resulting from malabsorption, pernicious anemia, or significant neurological symptoms, parenteral B12 administration is often preferred, especially initially. Intramuscular injections of cyanocobalamin or hydroxocobalamin are commonly used. A typical regimen involves 1000 mcg of B12 intramuscularly weekly for 4-8 weeks to rapidly replenish B12 stores, followed by monthly maintenance injections of 1000 mcg for life in conditions like pernicious anemia or post-gastrectomy. Subcutaneous injections are also an option and can be self-administered by patients after proper training.
-
Intranasal B12 Gel: For maintenance therapy in patients with pernicious anemia or malabsorption, intranasal B12 gel is available as an alternative to injections. It delivers B12 through nasal absorption and can be a convenient option for some patients who prefer to avoid injections.
-
Addressing Underlying Etiology: While B12 repletion is the immediate goal, addressing the underlying cause of the deficiency is crucial for long-term management. For dietary deficiency, dietary counseling and B12 supplementation are sufficient. For malabsorption syndromes, managing the underlying condition (e.g., Crohn’s disease, celiac disease) is essential. In pernicious anemia, lifelong B12 replacement is necessary due to irreversible intrinsic factor deficiency. For medication-induced deficiency (e.g., metformin, PPIs), considering alternative medications or B12 supplementation may be needed.
-
Monitoring and Follow-up: After initiating B12 treatment, monitoring the patient’s clinical response and laboratory parameters is important. Improvement in symptoms, resolution of anemia, normalization of MCV, and increases in serum B12 levels, along with decreases in MMA and homocysteine levels, indicate effective treatment. Regular follow-up and periodic B12 level checks are recommended, especially in patients with ongoing risk factors for deficiency.
-
Prophylactic B12 Supplementation: In individuals at high risk of developing B12 deficiency, such as strict vegans, patients with malabsorption syndromes, or post-gastrectomy patients, prophylactic B12 supplementation may be considered to prevent deficiency before it develops. However, routine prophylactic treatment is not universally recommended, and monitoring B12 status and intervening when deficiency is detected is a common approach.
The choice of treatment modality for b12 diagnosis and deficiency is individualized based on the etiology, severity, patient preference, and comorbidities. Effective management requires a comprehensive approach encompassing B12 repletion, addressing underlying causes, and ongoing monitoring.
Differential Diagnosis of B12 Deficiency
When considering a b12 diagnosis, it is crucial to differentiate vitamin B12 deficiency from other conditions that can present with similar hematologic and neurologic manifestations. The differential diagnosis includes:
-
Folate Deficiency: Folate deficiency is another common cause of macrocytic anemia and can present with fatigue, weakness, and glossitis, similar to B12 deficiency. However, neurological symptoms are less common in isolated folate deficiency. Differentiating between the two is crucial as treatment strategies differ. Measuring both serum B12 and folate levels is essential for distinguishing these conditions. Elevated MMA levels are specific to B12 deficiency, whereas homocysteine is elevated in both B12 and folate deficiency.
-
Other Causes of Macrocytic Anemia: Besides B12 and folate deficiency, other conditions can cause macrocytic anemia, including:
- Alcohol abuse: Alcohol can directly suppress bone marrow function and lead to macrocytosis.
- Myelodysplastic syndromes (MDS): These are bone marrow disorders characterized by ineffective blood cell production, often with macrocytosis.
- Hypothyroidism: Severe hypothyroidism can sometimes cause macrocytic anemia.
- Liver disease: Chronic liver disease can be associated with macrocytosis.
- Drug-induced macrocytosis: Certain medications, such as hydroxyurea and zidovudine, can cause macrocytosis.
-
Neurological Conditions Mimicking B12 Deficiency: The neurological manifestations of B12 deficiency, such as peripheral neuropathy, ataxia, and cognitive impairment, can overlap with other neurological disorders, including:
- Multiple Sclerosis (MS): MS can cause a wide range of neurological symptoms, including sensory disturbances, weakness, and ataxia.
- HIV Myelopathy: HIV infection can affect the spinal cord, leading to myelopathy with symptoms resembling SCDSC.
- Syphilis (Neurosyphilis): Neurosyphilis can present with neurological deficits, including sensory ataxia and cognitive impairment.
- Lead Toxicity: Lead poisoning can cause neuropathy and cognitive dysfunction.
- Peripheral Neuropathies of Other Etiologies: Diabetic neuropathy, alcoholic neuropathy, and other toxic or metabolic neuropathies can mimic B12 deficiency neuropathy.
- Dementia and Cognitive Impairment of Other Causes: Alzheimer’s disease, vascular dementia, and other neurodegenerative conditions can present with cognitive decline, requiring differentiation from B12 deficiency-related cognitive impairment.
A thorough clinical evaluation, targeted laboratory testing (including B12, folate, MMA, homocysteine levels), and consideration of other diagnostic possibilities are essential for accurate b12 diagnosis and appropriate management.
Prognosis of B12 Deficiency
The prognosis for patients with vitamin B12 deficiency is generally favorable, especially when diagnosed and treated promptly. Early b12 diagnosis and treatment are critical to prevent irreversible neurological damage.
-
Hematologic Recovery: Anemia and macrocytosis typically respond rapidly to B12 repletion. Improvement in fatigue and pallor is usually noticeable within days to weeks of starting treatment, and normalization of CBC parameters occurs within a few weeks to months.
-
Neurological Recovery: Neurological symptoms may take longer to improve and the extent of recovery depends on the severity and duration of symptoms before treatment. Patients with mild or recent-onset neurological deficits often experience significant or complete recovery. However, in cases with severe or long-standing neurological damage, particularly SCDSC, residual deficits may persist despite treatment. Early intervention is crucial to maximize neurological recovery. Younger patients generally tend to have better neurological outcomes compared to older individuals with more chronic conditions.
-
Factors Influencing Prognosis:
- Age: Younger patients tend to have better outcomes than older patients.
- Severity and Duration of Symptoms: Mild, recent-onset symptoms have a better prognosis than severe, chronic symptoms.
- Presence of Neurological Deficits: Patients without severe neurological deficits at diagnosis have a better prognosis.
- Adherence to Treatment: Consistent B12 replacement therapy, especially in chronic conditions like pernicious anemia, is essential for maintaining remission and preventing recurrence of deficiency and its complications.
-
Long-term Outlook: With ongoing B12 replacement therapy and management of underlying conditions, patients with B12 deficiency can lead normal, healthy lives. Lifelong B12 therapy may be required in conditions like pernicious anemia or post-gastrectomy. Regular monitoring and follow-up are important to ensure treatment effectiveness and detect any recurrence or complications.
While the prognosis is generally good with timely b12 diagnosis and treatment, delayed diagnosis or inadequate treatment can lead to irreversible neurological damage and poorer outcomes.
Complications of Untreated B12 Deficiency
Untreated vitamin B12 deficiency can lead to a range of serious complications, affecting both hematologic and neurologic systems, as well as increasing the risk of other health issues. Potential complications include:
-
Severe Anemia and Heart Failure: Severe macrocytic anemia from B12 deficiency can lead to reduced oxygen-carrying capacity of the blood, causing tissue hypoxia and strain on the cardiovascular system. In susceptible individuals, this can precipitate heart failure or exacerbate pre-existing cardiac conditions.
-
Irreversible Neurological Damage: Prolonged B12 deficiency can result in progressive and potentially irreversible neurological damage, particularly SCDSC. This can manifest as chronic peripheral neuropathy, persistent ataxia, cognitive impairment, dementia, and even paralysis in severe cases. Early b12 diagnosis and treatment are crucial to prevent irreversible neurological sequelae.
-
Increased Risk of Gastric Cancer: Pernicious anemia, a common cause of B12 deficiency, is associated with an increased risk of gastric cancer, particularly gastric carcinoid tumors and adenocarcinoma. This increased risk is attributed to chronic atrophic gastritis, which is a feature of pernicious anemia. Regular endoscopic surveillance may be recommended in patients with pernicious anemia.
-
Increased Risk of Autoimmune Disorders: Pernicious anemia is itself an autoimmune condition, and individuals with pernicious anemia have an increased risk of developing other autoimmune disorders, such as type 1 diabetes mellitus, autoimmune thyroid disease (Hashimoto’s thyroiditis, Graves’ disease), vitiligo, and myasthenia gravis.
-
Pregnancy Complications: B12 deficiency in pregnant women has been linked to an increased risk of neural tube defects in the fetus, as well as other adverse pregnancy outcomes. Adequate B12 status is essential during pregnancy.
-
Other Potential Complications: Some studies suggest potential associations between B12 deficiency and increased risk of cardiovascular disease, cognitive decline, and osteoporosis, although more research is needed to confirm these links.
Preventing these complications underscores the importance of timely b12 diagnosis and effective treatment of vitamin B12 deficiency.
Deterrence and Patient Education for B12 Deficiency
Preventive measures and patient education are crucial in mitigating the risk of vitamin B12 deficiency and ensuring early detection and management. Key aspects of deterrence and patient education include:
-
Dietary Education: Individuals following vegan or strict vegetarian diets should be educated about the importance of B12 supplementation. Plant-based foods do not naturally contain B12, so supplementation or consumption of B12-fortified foods is necessary to prevent deficiency. Vegetarians who consume dairy and eggs should also be aware of the potential for deficiency, especially if intake is limited.
-
Awareness of Risk Factors: Patients with risk factors for B12 deficiency, such as older adults, individuals with malabsorption syndromes (Crohn’s disease, celiac disease), post-gastrectomy patients, and those taking metformin or PPIs long-term, should be educated about their increased risk and the importance of regular B12 status monitoring.
-
Importance of Supplement Adherence: Patients prescribed B12 supplements, particularly those with pernicious anemia or malabsorption requiring lifelong therapy, need to understand the importance of consistent adherence to their treatment regimen to prevent recurrence of deficiency and its complications.
-
Recognizing Symptoms: Patients should be educated about the common symptoms of B12 deficiency, such as fatigue, weakness, pallor, peripheral neuropathy (numbness, tingling), and cognitive changes. Promptly reporting these symptoms to a healthcare provider can facilitate early b12 diagnosis and intervention.
-
Routine Screening: In at-risk populations, such as older adults and individuals with malabsorption risk factors, routine screening for B12 deficiency may be considered as part of preventive care.
-
Family Screening: In families with a history of pernicious anemia, other family members may be at increased risk and should be aware of the condition and consider screening.
-
Healthcare Provider Education: Healthcare professionals, including primary care physicians, nurses, pharmacists, and dietitians, play a vital role in educating patients about B12 deficiency, risk factors, prevention, and the importance of early b12 diagnosis and treatment.
Effective patient education and preventive strategies are essential in reducing the burden of vitamin B12 deficiency and its associated health consequences.
Enhancing Healthcare Team Outcomes in B12 Deficiency Management
Optimal management of vitamin B12 deficiency requires a collaborative, interprofessional healthcare team approach. Effective teamwork improves patient outcomes and ensures comprehensive care. Key roles and strategies for enhancing healthcare team outcomes include:
-
Primary Care Physician: The primary care physician is often the first point of contact for patients with suspected B12 deficiency. Their role includes:
- Recognizing risk factors and symptoms of B12 deficiency.
- Ordering initial screening tests (CBC, serum B12 level).
- Initiating initial treatment and referral to specialists when needed.
- Providing ongoing monitoring and management of B12 deficiency.
-
Gastroenterologist: A gastroenterologist is crucial in evaluating and managing malabsorption causes of B12 deficiency, such as Crohn’s disease, celiac disease, and pernicious anemia. Their roles include:
- Performing diagnostic procedures (endoscopy, biopsies) to identify GI causes of malabsorption.
- Managing underlying GI conditions.
- Collaborating with the primary care physician on B12 management strategies.
-
Neurologist: A neurologist is essential in evaluating and managing neurological complications of B12 deficiency, such as SCDSC and peripheral neuropathy. Their roles include:
- Performing neurological examinations to assess the extent of neurological involvement.
- Guiding treatment strategies for neurological symptoms.
- Differentiating B12 deficiency-related neurological issues from other neurological disorders.
-
Hematologist: A hematologist may be consulted in complex cases of B12 deficiency-related anemia, especially if there are diagnostic challenges or coexisting hematologic conditions.
-
Pharmacist: The pharmacist plays a crucial role in:
- Ensuring appropriate B12 supplementation (oral, injectable, intranasal).
- Educating patients on proper medication administration and adherence.
- Identifying potential drug interactions or medication-related causes of B12 deficiency (e.g., metformin, PPIs).
-
Registered Dietitian: A registered dietitian is vital in:
- Providing dietary counseling for patients with dietary B12 deficiency (vegans, vegetarians).
- Educating patients on B12-rich foods and fortified products.
- Assessing nutritional status and identifying other potential nutrient deficiencies.
-
Nurse: Nurses play a key role in:
- Patient education about B12 deficiency, treatment, and follow-up.
- Administering B12 injections and training patients/caregivers for self-administration.
- Monitoring patient response to treatment and reporting any concerns to the healthcare team.
- Coordinating care and communication among team members.
Effective communication, shared decision-making, and clear delineation of roles among team members are essential for optimizing patient care in b12 diagnosis and management. Regular team meetings and case conferences can facilitate coordinated care and improve patient outcomes.
Outcomes of B12 Deficiency Treatment
The outcomes of vitamin B12 deficiency treatment are generally positive, particularly with early b12 diagnosis and prompt intervention.
-
Hematologic Improvement: Anemia and macrocytosis typically resolve rapidly with B12 therapy. Hemoglobin levels and MCV normalize within weeks to months, and patients experience improved energy levels and reduced symptoms of anemia.
-
Neurological Improvement: Neurological symptoms often show improvement with B12 repletion, although the extent and rate of recovery vary. Peripheral neuropathy, ataxia, and cognitive impairment may gradually improve over months to years. Patients with milder or recent-onset neurological deficits tend to have better neurological recovery. In cases of severe or long-standing SCDSC, some residual neurological deficits may persist despite treatment. Early treatment is crucial for maximizing neurological recovery.
-
Factors Influencing Outcomes:
- Timeliness of Treatment: Early diagnosis and treatment initiation lead to better outcomes, especially for neurological recovery.
- Severity of Deficiency: Patients with milder deficiency generally have better outcomes than those with severe, long-standing deficiency.
- Patient Adherence: Consistent adherence to B12 replacement therapy, especially in chronic conditions, is essential for maintaining long-term remission and preventing recurrence.
- Underlying Etiology: Management of the underlying cause of B12 deficiency, when possible, is important for long-term outcomes.
-
Long-term Monitoring: Even after successful treatment, long-term monitoring of B12 status and clinical follow-up are recommended, especially in patients with chronic conditions like pernicious anemia or malabsorption, to ensure sustained B12 repletion and detect any recurrence or complications.
Overall, with timely b12 diagnosis, appropriate treatment, and ongoing management, most patients with vitamin B12 deficiency can achieve significant clinical improvement and prevent serious long-term sequelae.
Review Questions (Example – Based on Original Article)
- Which glycoprotein, produced by parietal cells in the stomach, is necessary for vitamin B12 absorption?
- List three potential etiologies of vitamin B12 deficiency.
- What hematologic and neurologic symptoms can result from vitamin B12 deficiency?
- What initial lab tests are typically ordered in the evaluation of suspected vitamin B12 deficiency?
- Describe the recommended treatment approach for vitamin B12 deficiency due to pernicious anemia.
References
(Same references as the original article would be listed here, maintaining the original numbering)
1.Layden AJ, Täse K, Finkelstein JL. Neglected tropical diseases and vitamin B12: a review of the current evidence. Trans R Soc Trop Med Hyg. 2018 Oct 01;112(10):423-435. [PMC free article: PMC6457089] [PubMed: 30165408]
2.Fritz J, Walia C, Elkadri A, Pipkorn R, Dunn RK, Sieracki R, Goday PS, Cabrera JM. A Systematic Review of Micronutrient Deficiencies in Pediatric Inflammatory Bowel Disease. Inflamm Bowel Dis. 2019 Feb 21;25(3):445-459. [PubMed: 30137322]
3.Miller JW. Proton Pump Inhibitors, H2-Receptor Antagonists, Metformin, and Vitamin B-12 Deficiency: Clinical Implications. Adv Nutr. 2018 Jul 01;9(4):511S-518S. [PMC free article: PMC6054240] [PubMed: 30032223]
4.Röhrig G, Gütgemann I, Kolb G, Leischker A. [Clinical hematological symptoms of vitamin B12 deficiency in old age : Summarized overview of this year’s symposium of the Working Group “Anemia in the Aged” on the occasion of the annual conference of the German Geriatric Society (DGG) in Frankfurt]. Z Gerontol Geriatr. 2018 Jun;51(4):446-452. [PubMed: 29796870]
5.Devi A, Rush E, Harper M, Venn B. Vitamin B12 Status of Various Ethnic Groups Living in New Zealand: An Analysis of the Adult Nutrition Survey 2008/2009. Nutrients. 2018 Feb 07;10(2) [PMC free article: PMC5852757] [PubMed: 29414857]
6.Oo TH, Rojas-Hernandez CM. Challenging clinical presentations of pernicious anemia. Discov Med. 2017 Sep;24(131):107-115. [PubMed: 28972879]
7.Cavalcoli F, Zilli A, Conte D, Massironi S. Micronutrient deficiencies in patients with chronic atrophic autoimmune gastritis: A review. World J Gastroenterol. 2017 Jan 28;23(4):563-572. [PMC free article: PMC5292330] [PubMed: 28216963]
8.Coskun M, Sevencan NO. The Evaluation of Ophthalmic Findings in Women Patients With Iron and Vitamin B12 Deficiency Anemia. Transl Vis Sci Technol. 2018 Aug;7(4):16. [PMC free article: PMC6108531] [PubMed: 30159209]
9.Bhat DS, Gruca LL, Bennett CD, Katre P, Kurpad AV, Yajnik CS, Kalhan SC. Evaluation of tracer labelled methionine load test in vitamin B-12 deficient adolescent women. PLoS One. 2018;13(5):e0196970. [PMC free article: PMC5967743] [PubMed: 29795596]
10.Guan B, Yang J, Chen Y, Yang W, Wang C. Nutritional Deficiencies in Chinese Patients Undergoing Gastric Bypass and Sleeve Gastrectomy: Prevalence and Predictors. Obes Surg. 2018 Sep;28(9):2727-2736. [PubMed: 29754386]
11.Bromage S, Ganmaa D, Rich-Edwards JW, Rosner B, Bater J, Fawzi WW. Projected effectiveness of mandatory industrial fortification of wheat flour, milk, and edible oil with multiple micronutrients among Mongolian adults. PLoS One. 2018;13(8):e0201230. [PMC free article: PMC6071971] [PubMed: 30070992]
12.Homan J, Schijns W, Aarts EO, Janssen IMC, Berends FJ, de Boer H. Treatment of Vitamin and Mineral Deficiencies After Biliopancreatic Diversion With or Without Duodenal Switch: a Major Challenge. Obes Surg. 2018 Jan;28(1):234-241. [PubMed: 28861696]
13.Freedberg DE, Kim LS, Yang YX. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017 Mar;152(4):706-715. [PubMed: 28257716]
14.Ziegler O, Sirveaux MA, Brunaud L, Reibel N, Quilliot D. Medical follow up after bariatric surgery: nutritional and drug issues. General recommendations for the prevention and treatment of nutritional deficiencies. Diabetes Metab. 2009 Dec;35(6 Pt 2):544-57. [PubMed: 20152742]
15.Cham G, Davis N, Strivens E, Traves A, Manypeney G, Gunnarsson R. Factors correlating to the propensity of general practitioners to substitute borderline vitamin B12 deficiency. Scand J Prim Health Care. 2018 Sep;36(3):242-248. [PMC free article: PMC6381524] [PubMed: 29933709]
16.Watson J, Lee M, Garcia-Casal MN. Consequences of Inadequate Intakes of Vitamin A, Vitamin B12, Vitamin D, Calcium, Iron, and Folate in Older Persons. Curr Geriatr Rep. 2018;7(2):103-113. [PMC free article: PMC5918526] [PubMed: 29721404]