Introduction
Idiopathic intracranial hypertension (IIH), previously known as benign intracranial hypertension, is a condition characterized by elevated intracranial pressure (ICP) without a detectable underlying cause such as a tumor or hydrocephalus. As content creators at xentrydiagnosis.store, we understand the importance of precision and expertise in diagnostics, whether it’s for vehicles or the human body. While our primary focus is automotive repair, understanding complex diagnostic processes in other fields, like medicine, sharpens our analytical skills. This article delves into the diagnosis of benign intracranial hypertension, a condition with a rising incidence, especially amongst certain populations. Recognizing the subtle signs and understanding the diagnostic pathway is crucial for timely intervention and preventing severe complications.
The incidence of IIH is significantly higher in young, obese women, estimated at 20 per 100,000 in this demographic, compared to normal-weight individuals. This represents a 20-fold increase, highlighting the strong correlation with obesity. Given the alarming global rise in obesity rates, the prevalence of IIH is expected to escalate. While initially considered primarily a condition affecting young women, it’s now recognized that obesity, rather than gender or age, is likely the predominant risk factor. This broader understanding is essential for effective diagnosis across diverse patient groups.
Visual impairment is a major concern in IIH, present in up to 90% of patients at diagnosis. Historically, a significant proportion progressed to permanent visual loss. However, recent studies suggest a better visual prognosis, possibly due to earlier diagnosis and increased awareness. Despite this improvement, delayed diagnosis remains a challenge as the symptoms can be insidious, and patients often consult various specialists before receiving the correct diagnosis of benign intracranial hypertension. This article aims to provide a comprehensive overview of the diagnostic process, crucial symptoms, and investigative strategies for benign intracranial hypertension.
Clinical Presentation and Diagnostic Indicators
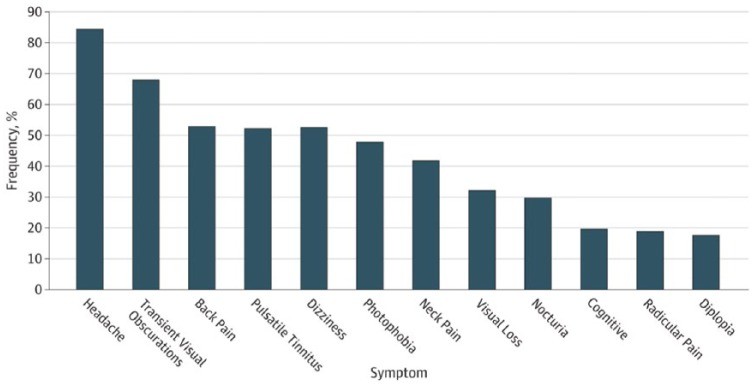
Benign intracranial hypertension typically manifests with a combination of symptoms, with headache, visual disturbances, and papilledema (swelling of the optic disc) being the most common triad. These symptoms are well-documented and serve as key indicators for clinicians.
Headache is reported by the vast majority of IIH patients, around 93%, often described as a constant or near-daily occurrence. The headache associated with benign intracranial hypertension lacks specific characteristics, frequently mimicking chronic migraine or tension-type headaches. However, it’s more likely to be localized rather than across the entire head and often has a pulsating quality. Factors like coughing, straining, and physical exertion can exacerbate the headache, providing important clues for diagnosis.
Pulsatile tinnitus, a rhythmic whooshing sound in the ears, is another hallmark symptom, resulting from increased vascular pulsations due to high ICP. While highly prevalent, patients may not spontaneously report it unless specifically asked. This highlights the importance of detailed questioning during the diagnostic process.
Visual disturbances are critical. Transitory visual obscurations, brief episodes of vision loss or dimming, can occur due to increased pressure on the optic nerve. Papilledema, a direct sign of increased ICP, is a key clinical finding. It’s important to note that in rare cases, increased ICP can occur without papilledema, especially in patients with chronic migraines. Diagnosing IIH without papilledema requires careful consideration and additional investigations.
Other symptoms can include dizziness, nausea, memory and concentration difficulties, and double vision (diplopia), particularly horizontal diplopia due to sixth nerve palsy. Furthermore, cognitive dysfunction, affecting executive function, memory, and processing speed, has been increasingly recognized as a significant aspect of IIH, even persisting after ICP normalization.
Diagnostic Examination and Procedures
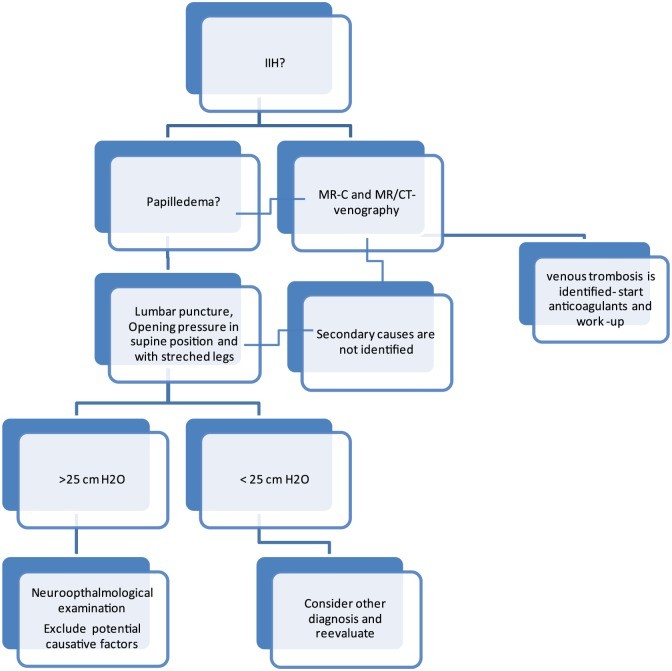
Diagnosing benign intracranial hypertension requires a systematic approach, combining clinical examination, neuroimaging, and lumbar puncture. Fundoscopy, the examination of the optic disc with an ophthalmoscope, is the initial crucial step. Detecting papilledema through fundoscopy is a primary indicator of IIH. While the interpretation of papilledema can vary, especially among less experienced clinicians, it remains a readily accessible and essential bedside test, especially in emergency settings.
Visual field testing, ideally using standardized perimetry, is also vital to assess the extent of visual impairment. Optical coherence tomography (OCT) is a recommended advanced technique for quantifying papilledema and monitoring its changes over time, providing objective measurements for diagnosis and follow-up.
Neuroimaging, primarily magnetic resonance imaging (MRI) of the brain, is the next essential step. MRI helps rule out other conditions that can cause increased ICP, such as brain tumors, hydrocephalus, or venous sinus thrombosis. Specifically, MR venography or CT venography is crucial to exclude sinus venous occlusions, which can present similarly to IIH. While bilateral transverse sinus stenosis is frequently observed in IIH patients, its role in the disease’s cause versus being a marker of elevated ICP is still debated. Other neuroimaging findings suggestive of IIH include an empty sella turcica, flattening of the posterior sclera of the globe, and distention of the perioptic subarachnoid space.
Lumbar puncture with manometry is the definitive procedure to confirm elevated ICP. This involves measuring the cerebrospinal fluid (CSF) pressure by inserting a needle into the lower back. Accurate measurement requires a standardized procedure: the patient should be in the lateral decubitus position, relaxed, and with legs extended. Opening pressure above 25 cm H2O is considered elevated in adults. However, ICP can fluctuate, and repeated measurements might be necessary in atypical cases or when the initial pressure is borderline high. CSF analysis is also performed to ensure normal composition, ruling out infections or inflammatory conditions.
Based on clinical evidence and expertise, a structured diagnostic pathway is recommended for suspected benign intracranial hypertension cases.
Diagnostic Criteria for Benign Intracranial Hypertension
The diagnostic criteria for pseudotumor cerebri syndrome, which encompasses benign intracranial hypertension, are well-defined to ensure accurate diagnosis. These criteria, established by Friedman et al., provide a framework for clinicians.
| 1. Required for diagnosis of pseudotumor cerebri syndromea |
|---|
| 1. Papilloedema |
| 2. Normal neurologic examination except for cranial nerve abnormalities |
| 3. Neuroimaging: Normal brain parenchyma without evidence of hydrocephalus, mass, or structural lesion and no abnormal meningeal enhancement on MRI, with and without gadolinium, for typical patients (female and obese), and MRI, with and without gadolinium, and magnetic resonance venography for others; if MRI is unavailable or contraindicated, contrast-enhanced CT may be used |
| 4. Normal CSF composition |
| 5. Elevated lumbar puncture opening pressure (⩾250 mm CSF in adults and ⩾280 mm CSF in children [250 mm CSF if the child is not sedated and not obese]) in a properly performed lumbar puncture |
| 2. Diagnosis of pseudotumor cerebri syndrome without papilloedema |
| – In the absence of papilloedema, a diagnosis of pseudotumor cerebri syndrome can be made if B–E from above are satisfied, and in addition the patient has a unilateral or bilateral abducens nerve palsy. |
| – In the absence of papilloedema or sixth nerve palsy, a diagnosis of pseudotumor cerebri syndrome can be suggested but not made if B–E from above are satisfied, and in addition at least three of the following neuroimaging criteria are satisfied: |
| 1. Empty sella |
| 2. Flattening of the posterior aspect of the globe |
| 3. Distention of the perioptic subarachnoid space with or without a tortuous optic nerve |
| 4. Transverse venous sinus stenosis |
These criteria emphasize the necessity of papilledema, normal neurological examination (excluding cranial nerve abnormalities), normal neuroimaging, normal CSF composition, and elevated CSF pressure for a definitive diagnosis. Importantly, the criteria also address diagnosing pseudotumor cerebri syndrome (benign intracranial hypertension) without papilledema, acknowledging cases where papilledema is absent but other indicators and neuroimaging findings are present.
Conclusion
Accurate and timely diagnosis of benign intracranial hypertension is paramount to prevent vision loss and manage debilitating symptoms like headache. The diagnostic process involves recognizing the characteristic clinical presentation, performing thorough neurological and ophthalmological examinations, utilizing neuroimaging to exclude other conditions, and confirming elevated ICP via lumbar puncture. Adherence to established diagnostic criteria and a systematic approach are crucial for clinicians. Just as in automotive diagnostics where precision and a step-by-step process are key to identifying and resolving complex issues, the diagnosis of benign intracranial hypertension demands a similar level of expertise and methodical investigation. Increased awareness and specialized care teams are essential to improve outcomes for individuals affected by this challenging condition.