Introduction
Experiencing numbness in both arms can be a disconcerting symptom, often triggering concern and prompting a search for answers. For automotive technicians, who rely heavily on hand dexterity and tactile feedback for diagnostics and repairs, bilateral arm numbness can be particularly alarming and potentially career-impacting. Understanding the possible causes of bilateral arm numbness is crucial for seeking timely and appropriate medical evaluation. This article provides a comprehensive overview of the differential diagnoses for bilateral arm numbness, drawing upon neurological principles and relevant medical conditions, and expanding on the complexities presented in cases like “person-in-the-barrel” syndrome. We aim to equip you with a foundational understanding to better navigate this symptom and advocate for your health.
Common Causes of Bilateral Arm Numbness
Bilateral arm numbness, meaning a loss of sensation or abnormal sensation affecting both arms, can arise from a variety of conditions affecting different parts of the nervous system. It’s essential to consider the symptom’s characteristics – is it constant or intermittent? Is it accompanied by weakness, pain, or tingling? These details help narrow down the potential diagnoses. The causes can be broadly categorized into peripheral nervous system issues, central nervous system conditions, and systemic illnesses.
Peripheral Nervous System Disorders
The peripheral nervous system (PNS) comprises the nerves outside the brain and spinal cord. When these nerves are compromised bilaterally, it can lead to symmetrical symptoms like numbness in both arms.
1. Peripheral Neuropathies
Peripheral neuropathy refers to damage to the peripheral nerves. When it affects nerves in both arms symmetrically, it can cause bilateral numbness.
-
Vasculitic Neuropathy (Mononeuritis Multiplex): As highlighted in the original article concerning “person-in-the-barrel” syndrome, vasculitis, or inflammation of blood vessels, can cause mononeuritis multiplex. This condition affects multiple peripheral nerves in a seemingly random pattern. While the original case presented with bilateral arm weakness, sensory symptoms like numbness are also common. The patchy nerve damage from vasculitis can indeed manifest as bilateral arm numbness.
 Mononeuritis multiplex can cause patchy nerve damage leading to sensory and motor deficits.
Mononeuritis multiplex can cause patchy nerve damage leading to sensory and motor deficits.Alt text: Illustration depicting patchy nerve damage in mononeuritis multiplex, highlighting its potential to cause sensory and motor deficits.
-
Diabetic Neuropathy: Diabetes mellitus is a common cause of peripheral neuropathy. High blood sugar levels can damage nerves over time. Diabetic neuropathy often presents in a “stocking-glove” distribution, affecting hands and feet symmetrically, and can include numbness, tingling, and pain in both arms.
-
Vitamin Deficiencies: Deficiencies in certain B vitamins, particularly B12, as well as vitamin E, can lead to peripheral neuropathy and bilateral arm numbness. These vitamins are crucial for nerve health, and their lack can impair nerve function.
-
Toxic Neuropathies: Exposure to certain toxins, including heavy metals and some industrial chemicals, can cause peripheral nerve damage and bilateral arm numbness. Automotive technicians working with various chemicals should be aware of potential neurotoxic exposures.
2. Brachial Plexopathy (Bilateral, Rare)
The brachial plexus is a network of nerves that originates in the neck and shoulder and supplies the arm and hand. While brachial plexopathy is more commonly unilateral (affecting one arm), bilateral brachial plexopathy, though rare, can occur and cause numbness in both arms. This can be due to:
- Inflammatory or Autoimmune Conditions: Conditions like Parsonage-Turner syndrome (neuralgic amyotrophy), though typically unilateral, can rarely affect both brachial plexuses.
- Thoracic Outlet Syndrome (TOS): While TOS often presents with unilateral symptoms, bilateral TOS is possible, especially if anatomical factors or postural habits contribute to compression on both sides. TOS involves compression of nerves or blood vessels in the space between the collarbone and the first rib.
3. Nerve Entrapment Syndromes (Less Likely Bilateral Arm Numbness)
Conditions like carpal tunnel syndrome and cubital tunnel syndrome are nerve entrapment syndromes. While these are common causes of numbness in the hand and arm, they are typically unilateral. Bilateral carpal tunnel syndrome is possible, particularly in conditions causing fluid retention or hormonal changes, but it’s less likely to be the sole explanation for widespread bilateral arm numbness extending beyond the hands.
Central Nervous System Disorders
The central nervous system (CNS) includes the brain and spinal cord. Conditions affecting the CNS can also manifest as bilateral arm numbness.
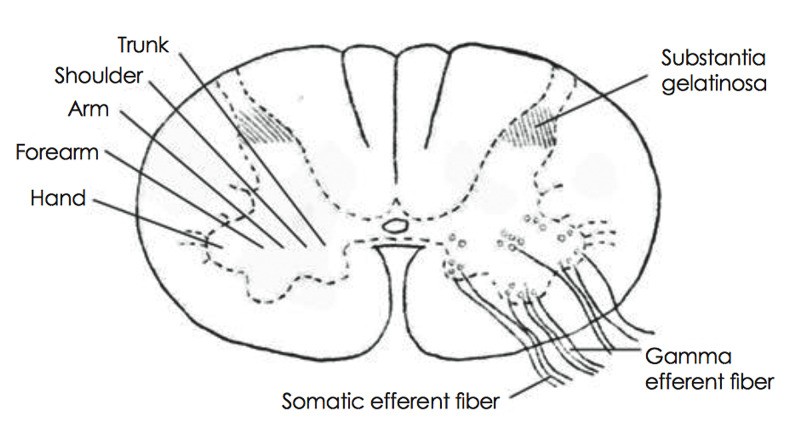
1. Cervical Myelopathy (Spinal Cord Compression in the Neck)
Cervical myelopathy, or compression of the spinal cord in the neck, is a significant cause of bilateral arm symptoms. The spinal cord carries sensory and motor pathways, and compression in the cervical region can disrupt signals to both arms, leading to numbness, weakness, and other neurological deficits. Causes include:
- Cervical Spondylosis: Degenerative changes in the cervical spine, such as bone spurs and disc herniation, can narrow the spinal canal and compress the spinal cord.
- Cervical Spinal Stenosis: Narrowing of the spinal canal in the neck.
- Cervical Disc Herniation: A herniated disc in the neck can press on the spinal cord.
2. Multiple Sclerosis (MS)
Multiple sclerosis is an autoimmune disease that affects the brain and spinal cord. MS can cause a wide range of neurological symptoms, including bilateral arm numbness, weakness, and sensory disturbances. MS lesions in the spinal cord or brainstem can disrupt sensory pathways to both arms.
3. Stroke (Brainstem or Bilateral Cerebral Infarcts)
While stroke typically causes unilateral weakness or numbness, certain types of strokes can cause bilateral arm numbness.
-
Brainstem Stroke: The brainstem contains pathways for sensation and movement for both sides of the body. A stroke in the brainstem can affect both arms (and potentially legs).
-
Bilateral Cerebral Infarcts (Watershed Infarcts): As discussed in the context of “person-in-the-barrel” syndrome, watershed infarcts, occurring in the border zones between major cerebral arteries, can selectively affect the motor cortex areas controlling the arms. While the original article focused on weakness, sensory involvement and numbness can also occur in these infarcts. These are often caused by systemic hypoperfusion (reduced blood flow to the brain).
Alt text: Diagram illustrating watershed infarcts in the brain, showing how they can affect motor areas related to arm function and potentially cause sensory deficits like numbness.
4. Anterior Spinal Cord Syndrome
Anterior spinal cord syndrome, often caused by infarction (loss of blood supply) of the anterior spinal artery, can damage the anterior portion of the spinal cord. This can lead to bilateral weakness and sensory loss, including numbness, below the level of the lesion. The anterior horn cells, as mentioned in the original article’s discussion of ischemia, are particularly vulnerable.
Systemic Conditions
Certain systemic conditions can indirectly or directly cause bilateral arm numbness.
1. Autoimmune Diseases
Besides vasculitis, other autoimmune diseases like lupus and rheumatoid arthritis can sometimes cause peripheral neuropathy or CNS involvement that leads to bilateral arm numbness.
2. Infections
Certain infections, such as Lyme disease or HIV, can affect the nervous system and cause peripheral neuropathy or CNS complications, potentially leading to bilateral arm numbness.
3. Critical Illness Myopathy and Polyneuropathy
As mentioned in the original article, critical illness myopathy and polyneuropathy, which can develop in severely ill patients, can cause generalized weakness and sensory disturbances, potentially including bilateral arm numbness.
4. Paraneoplastic Syndromes
In rare cases, cancers can trigger paraneoplastic syndromes, where the body’s immune system attacks the nervous system, leading to neurological symptoms like bilateral arm numbness.
Diagnostic Approach to Bilateral Arm Numbness
Evaluating bilateral arm numbness requires a thorough medical history, neurological examination, and often, diagnostic testing.
- Medical History: Detailed questioning about the onset, duration, character, location, and associated symptoms (weakness, pain, tingling) of the numbness, as well as past medical history, medications, and potential toxic exposures.
- Neurological Examination: Assessment of strength, reflexes, sensation, coordination, and cranial nerve function to localize the problem to the peripheral or central nervous system.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): These tests evaluate the function of peripheral nerves and muscles, helping to diagnose peripheral neuropathies, brachial plexopathies, and nerve entrapments. As seen in the case study, NCS/EMG is crucial for identifying mononeuritis multiplex.
- Blood Tests: To screen for underlying conditions like diabetes, vitamin deficiencies, autoimmune diseases, and inflammatory markers (like CRP and ESR, elevated in the case study).
- Cerebrospinal Fluid (CSF) Analysis: May be performed to evaluate for inflammatory or infectious conditions affecting the CNS, although in the presented case of vasculitis, CSF was non-inflammatory.
- Imaging Studies:
- MRI of the Cervical Spine: To evaluate for cervical myelopathy, spinal cord compression, disc herniation, and spinal stenosis.
- MRI of the Brain: To rule out MS, stroke, and other CNS lesions, especially if central causes are suspected.
- CT Angiography or MR Angiography: To evaluate blood vessels if vasculitis or stroke is suspected.
- Nerve Biopsy: In cases of suspected vasculitic neuropathy or other inflammatory neuropathies, a nerve biopsy (like the superficial radial sensory nerve biopsy considered in the original case) may be performed for definitive diagnosis.
Differential Diagnosis Summary
| Category | Condition | Key Features |
|---|---|---|
| Peripheral Neuropathies | Vasculitic Neuropathy (Mononeuritis Multiplex) | Patchy, asymmetric nerve involvement, sensory and motor deficits, inflammatory markers. |
| Diabetic Neuropathy | Symmetrical “stocking-glove” distribution, associated diabetes, other diabetic complications. | |
| Vitamin Deficiencies | History of poor diet, malabsorption, or specific vitamin deficiencies. | |
| Toxic Neuropathies | Exposure to neurotoxins, heavy metals, industrial chemicals. | |
| Brachial Plexopathy | Bilateral Brachial Plexopathy | Rare, potential inflammatory or compressive causes affecting both brachial plexuses. |
| Central Nervous System | Cervical Myelopathy | Neck pain, stiffness, weakness, sensory changes in arms and legs, bowel/bladder dysfunction. |
| Multiple Sclerosis (MS) | Relapsing-remitting or progressive neurological symptoms, optic neuritis, fatigue, other CNS signs. | |
| Stroke (Brainstem/Bilateral) | Sudden onset, other neurological deficits, risk factors for stroke. | |
| Anterior Spinal Cord Syndrome | Bilateral weakness, loss of pain and temperature sensation, preserved light touch and proprioception below lesion. | |
| Systemic Conditions | Autoimmune Diseases | Systemic symptoms of autoimmune disease (fatigue, joint pain, rash), specific serological markers. |
| Infections | History of infection, systemic symptoms, specific infectious agents identified. | |
| Critical Illness Neuropathy/Myopathy | Severe illness, prolonged ICU stay, generalized weakness and sensory changes. | |
| Paraneoplastic Syndromes | History of cancer, systemic symptoms, neurological deficits not explained by direct tumor involvement. |
Conclusion
Bilateral arm numbness is a complex symptom with a broad differential diagnosis, ranging from peripheral nerve disorders to central nervous system conditions and systemic illnesses. For automotive technicians, prompt and accurate diagnosis is crucial to maintain their livelihood and overall health. Understanding the potential causes, as outlined above, empowers individuals to seek timely medical attention and engage in informed discussions with healthcare providers. A comprehensive evaluation, including neurological examination and appropriate diagnostic testing, is essential to determine the underlying cause and guide effective management strategies. While “person-in-the-barrel” syndrome, as described in the original article, focuses on bilateral arm weakness, the underlying neurological principles and the case of vasculitic neuropathy highlight the intricate pathways and potential for varied presentations of neurological symptoms, including numbness in both arms. If you experience persistent or concerning bilateral arm numbness, seeking professional medical advice is paramount.