Introduction
As auto repair experts at xentrydiagnosis.store, we understand the complexities of diagnostics and the importance of a systematic approach. Just as we meticulously analyze vehicle systems, the human brain, particularly the deep gray matter structures like the basal ganglia, requires a similarly detailed diagnostic process when abnormalities arise. Bilateral basal ganglia hyperintensity, as observed on Magnetic Resonance Imaging (MRI), is a significant finding that can indicate a wide range of underlying conditions. Understanding the differential diagnosis is crucial for accurate assessment and appropriate management, even if our expertise is primarily in automotive systems, recognizing patterns and diagnostic approaches in other complex systems can be beneficial. This article provides a comprehensive overview of the differential diagnosis of bilateral basal ganglia hyperintensity, drawing from established medical knowledge to enhance your diagnostic acumen, applicable in principle across different complex systems.
The basal ganglia and thalami, central hubs within the brain, are responsible for a multitude of functions, from motor control and autonomic processes to cognition and emotion. Their high metabolic demand makes them vulnerable to various insults, often manifesting as bilateral lesions. While our focus at xentrydiagnosis.store is vehicle diagnostics, appreciating the systematic approach to diagnosing complex issues in other domains, like the human brain, can sharpen our problem-solving skills. This review will explore the diverse etiologies of bilateral basal ganglia hyperintensity, categorized by lesion location and pathology type, to provide a structured framework for differential diagnosis. We will delve into inherited metabolic disorders, acquired toxic and metabolic conditions, inflammatory and infectious processes, vascular events, and neoplastic causes, emphasizing characteristic imaging findings and clinical contexts relevant to understanding diagnostic processes in complex systems.
Pathology Predominantly Affecting the Basal Ganglia
Inherited Metabolic/Genetic Disorders
Leigh Syndrome (Subacute Necrotizing Encephalopathy)
Leigh syndrome, a severe mitochondrial disorder, typically presents in infancy or early childhood with progressive neurodegeneration. While we diagnose engine malfunctions, Leigh syndrome represents a critical system failure in the human body. Key MRI findings include bilateral symmetric T2 hyperintensity in the putamen and brainstem, often with restricted diffusion in acute phases. Other basal ganglia structures, the thalamus, and cerebellar dentate nuclei can also be involved. Elevated lactate levels in blood or CSF are suggestive.
Alt Text: Axial T2 MRI of a 6-year-old with Leigh Syndrome showing bilateral basal ganglia hyperintensity and thalamic lesions, indicative of mitochondrial dysfunction.
Alt Text: Axial FLAIR MRI of a 4-year-old with Leigh Syndrome highlighting bilateral putamen hyperintensity, a key imaging feature for differential diagnosis.
Glutaric Aciduria Type 1
Glutaric aciduria type 1, another inherited metabolic disorder, often manifests in infants with seizures and psychomotor regression. Just as we recognize patterns in vehicle diagnostic codes, the characteristic MRI features of glutaric aciduria type 1 are crucial. These include frontotemporal atrophy with widened Sylvian fissures (“bat wing” appearance), subdural hygromas, and bilateral T2 hyperintensity in the caudate and putamen, which may show restricted diffusion acutely and atrophy later.
Alt Text: Axial and coronal T2 MRI of a 14-year-old with Glutaric Aciduria Type 1 showing bilateral lentiform nuclei hyperintensity and frontotemporal white matter changes.
Alt Text: Axial T2 MRI and ADC map of a 20-month-old with Glutaric Aciduria Type 1 demonstrating basal ganglia hyperintensity, restricted diffusion, and widened Sylvian fissures.
Wilson Disease
Wilson disease, or hepatolenticular degeneration, results from impaired copper metabolism, leading to copper accumulation in the liver and brain. Like diagnosing electrical system faults, recognizing the subtle MRI signs of Wilson disease is key. Bilateral symmetric T2 hyperintensity in the putamen (often peripherally) is common, along with involvement of other basal ganglia structures, thalamus, and brainstem. T1 hyperintensity of the globus pallidus is frequently seen. The “face of the giant panda” sign in the midbrain is highly specific but not always present.
Alt Text: Axial T2 and T1 MRI of a 6-year-old with Wilson Disease showing bilateral putamen and caudate hyperintensity on T2 and globus pallidus hyperintensity on T1.
Huntington Disease
Huntington disease, a progressive neurodegenerative disorder, is characterized by striatal atrophy. Just as we understand wear and tear in mechanical components, Huntington disease represents a progressive degradation of brain structures. MRI shows bilateral caudate and putamen atrophy, particularly of the caudate heads, leading to a “boxed-out” appearance of the frontal horns. Juvenile-onset Huntington disease may present with T2 hyperintensity in the striatum.
Alt Text: Coronal T1 MRI of a 36-year-old with Huntington Disease showing caudate atrophy and “boxed-out” frontal horns, classic for this neurodegenerative disorder.
Alt Text: Axial T2 MRI of a 17-year-old with Juvenile Huntington Disease demonstrating caudate and putamen atrophy with associated hyperintensity.
Neurodegeneration with Brain Iron Accumulation (NBIA)
NBIA encompasses disorders with abnormal iron accumulation in the basal ganglia. Similar to identifying metallic debris in engine oil, MRI can detect abnormal iron deposits in the brain. The “eye of the tiger” sign, characterized by T2 hypointense globus pallidus with central hyperintensity, is nearly pathognomonic for pantothenate kinase-associated neurodegeneration (PKAN). Other NBIA subtypes may show different iron deposition patterns and additional features like cystic changes.
Alt Text: Axial FLAIR and T1 MRI of an 8-year-old with PKAN, showing the “eye of the tiger” sign in the globus pallidus, indicative of brain iron accumulation.
Acquired Metabolic/Toxic Disorders
Carbon Monoxide Poisoning
Carbon monoxide (CO) poisoning, a common cause of toxic injury, leads to tissue hypoxia. Just as exhaust fumes can damage a vehicle’s catalytic converter, CO poisoning damages brain tissue. Bilateral focal globus pallidus lesions, hypodense on CT and hyperintense on T2, FLAIR, and DWI, with restricted diffusion acutely, are highly characteristic. White matter hyperintensities are also common.
Alt Text: Axial CT scan of a 37-year-old CO poisoning victim showing bilateral globus pallidus hypodensity, characteristic of this toxic exposure.
Alt Text: Axial FLAIR MRI of a CO poisoning patient demonstrating bilateral globus pallidus hyperintensity and white matter changes due to hypoxia.
Bilirubin Encephalopathy (Kernicterus)
Kernicterus, a chronic form of bilirubin encephalopathy, results from severe neonatal jaundice. Just as improper fluid levels can damage a car engine, high bilirubin levels can damage the developing brain. Chronic kernicterus shows bilateral symmetric T2 hyperintensity in the globus pallidus and subthalamic nucleus. Acute to subacute phases demonstrate T1 hyperintensity in these regions.
Alt Text: Axial T2 MRI of a 4-year-old with Kernicterus showing bilateral globus pallidus hyperintensity, a hallmark of chronic bilirubin encephalopathy.
Chronic Hepatic Encephalopathy/Manganese Toxicity
Chronic hepatic encephalopathy, often associated with liver cirrhosis, can lead to manganese accumulation in the brain. Similar to contaminant buildup in vehicle fluids, manganese deposits can disrupt brain function. Bilateral symmetric globus pallidus T1 hyperintensity is characteristic. Other deep gray matter structures and white matter may also be affected.
Alt Text: Axial T1 MRI of a 49-year-old with chronic liver failure and manganese toxicity showing bilateral globus pallidus hyperintensity.
Gadolinium Deposition
Gadolinium deposition, following multiple contrast-enhanced MRIs, can also cause symmetric globus pallidus T1 hyperintensity. While we use contrast dyes in leak detection, repeated exposure in medical imaging can have unintended consequences. This finding needs to be differentiated from manganese deposition and hepatic encephalopathy.
Methanol Poisoning
Methanol poisoning, often from ingestion of industrial liquids, causes severe metabolic acidosis. Just as contaminated fuel damages engine components, methanol damages brain tissue. Characteristic bilateral hemorrhagic or non-hemorrhagic putaminal lesions are seen, hyperdense on CT and hyperintense on T2 MRI, often with T1 hyperintensity indicating hemorrhage. Frontal white matter involvement is also common.
Alt Text: Axial FLAIR MRI and ADC map of a 31-year-old with methanol poisoning showing bilateral putamen hyperintensity and frontal white matter changes.
Uremic Encephalopathy and Metabolic Acidosis
Uremic encephalopathy, a complication of end-stage renal failure, involves accumulation of uremic toxins. Just as contaminated fluids in a vehicle system cause malfunction, uremic toxins disrupt brain function. The “lentiform fork” sign, characterized by bilateral putaminal and globus pallidus swelling with a hyperintense rim along the medullary laminae, is a distinctive MRI feature.
Alt Text: Axial FLAIR MRI and ADC map of a 2-year-old with uremic encephalopathy showing the “lentiform fork” sign in the basal ganglia.
Hypoglycemia
Hypoglycemia, or low blood sugar, can cause severe brain damage. Just as fuel starvation damages an engine, glucose deprivation harms brain cells. MRI may show selective white matter or gray matter involvement, including the basal ganglia, with restricted diffusion. Thalamic sparing can help differentiate hypoglycemia from hypoxia.
Alt Text: Axial FLAIR MRI and ADC map of a 77-year-old with hypoglycemic encephalopathy showing bilateral cortical and striatal hyperintensity, sparing the thalamus.
Hyperglycemia
Hyperglycemia, specifically non-ketotic hyperglycemia, can cause hemichorea-hemiballismus. Like diagnosing erratic engine behavior, understanding the clinical context is crucial. CT and MRI show unilateral putaminal hyperdensity and T1 hyperintensity, respectively, contralateral to symptoms. This is characteristically unilateral, unlike most other metabolic disorders.
Alt Text: Axial CT and T1 MRI of a 79-year-old with hyperglycemia showing unilateral putamen hyperdensity and hyperintensity, associated with hemichorea-hemiballismus.
Inflammatory/Infectious Disorders
Autoimmune Encephalitis
Autoimmune encephalitis, mediated by antibodies against neuronal antigens, can target the basal ganglia. Just as electrical interference can cause erratic sensor readings, autoimmune processes disrupt brain function. Anti-CV2/CRMP5 encephalitis may show striatal and claustrum hyperintensity on T2 and FLAIR MRI.
Alt Text: Axial T2 MRI of a 46-year-old with autoimmune encephalitis showing bilateral putamen and caudate hyperintensity, associated with anti-CV2/CRMP5 antibodies.
Cryptococcosis
Cryptococcal CNS infection, particularly in immunocompromised individuals, can manifest as gelatinous pseudocysts or cryptococcomas in the basal ganglia. Similar to fungal growth in air conditioning systems, cryptococcal infection represents an opportunistic invasion. Pseudocysts are CSF-like on MRI but FLAIR hyperintense. Cryptococcomas are enhancing nodules.
Alt Text: Axial FLAIR and post-contrast T1 MRI of an HIV-positive patient with cryptococcosis showing bilateral basal ganglia lesions, some enhancing, indicative of fungal infection.
Neoplastic Disorders
Germinoma
Germinomas, intracranial tumors, can occur in the basal ganglia. Like diagnosing unusual noises in a vehicle, subtle imaging findings in germinomas can be challenging. They may be unilateral or bilateral, with mild CT hyperdensity and T1/T2 MRI hyperintensity. SWI/T2* MRI may show more prominent hypointensities. Hemiatrophy can develop in unilateral cases.
Alt Text: Axial T2 MRI of a 14-year-old with germinoma showing asymmetric basal ganglia lesions and hemiatrophy, suggestive of neoplastic origin.
Pathology Predominantly Affecting the Thalami
Inherited Metabolic/Genetic Disorders
Lysosomal Storage Disorders (Gangliosidoses)
Gangliosidoses, lysosomal storage disorders, can present with thalamic abnormalities. Just as sludge buildup in a car’s lubrication system disrupts function, lysosomal storage disorders disrupt cellular processes. Infantile gangliosidoses characteristically show hyperdense thalami on CT and T1 hyperintensity/T2 hypointensity on MRI.
Alt Text: Axial T1 and T2 MRI of a 17-month-old with Gangliosidosis showing bilateral thalamic hyperintensity on T1 and hypointensity on T2, a key feature of lysosomal storage disorders.
Acquired Metabolic/Toxic Disorders
Toluene Toxicity/Solvent Abuse
Toluene toxicity, from chronic solvent abuse, can cause irreversible brain damage. Similar to prolonged exposure to harsh chemicals damaging car paint, toluene damages brain tissue over time. Characteristic MRI findings include low T2 signal in the thalami and white matter hyperintensity with atrophy.
, rID: 17082)](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/a434/7405775/f57774e3b526/234_2020_2511_Fig21_HTML.jpg)
Alt Text: Axial T2 MRI of a 21-year-old with toluene toxicity showing bilateral thalamic hypointensity and white matter changes due to chronic solvent abuse.
Wernicke Encephalopathy (WE)
Wernicke encephalopathy, caused by thiamine deficiency, is often associated with alcoholism. Just as a malfunctioning fuel injection system starves the engine, thiamine deficiency starves the brain. Typical MRI findings include symmetric T2 hyperintensity in the medial thalami, periaqueductal gray matter, and mammillary bodies.
Alt Text: Axial FLAIR MRI of a 38-year-old with Wernicke Encephalopathy showing bilateral medial thalamic and periaqueductal gray matter hyperintensity due to thiamine deficiency.
Alt Text: Axial DWI and ADC map of a 49-year-old with Wernicke Encephalopathy due to alcoholism showing bilateral dorsomedial thalamic hyperintensity.
Acute Hyperammonemic Encephalopathy
Acute hyperammonemic encephalopathy, often due to liver disease, results in elevated ammonia levels. Similar to exhaust buildup in a poorly ventilated garage, ammonia buildup is toxic to the brain. MRI shows bilateral symmetric cortical hyperintensity in the insula and cingulate gyrus, often with thalamic involvement. Basal ganglia are typically spared.
Alt Text: Coronal FLAIR MRI of a 26-year-old with acute hyperammonemic encephalopathy showing bilateral insular, cingulate, thalamic, and hippocampal hyperintensity.
, rID: 39037)](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/a434/7405775/1b57df1d3d39/234_2020_2511_Fig25_HTML.jpg)
Alt Text: Axial DWI and T1 MRI of a 60-year-old with acute hyperammonemic encephalopathy due to liver cirrhosis, demonstrating cortical and thalamic hyperintensity and globus pallidus T1 hyperintensity.
Inflammatory/Infectious Disorders
Acute Necrotizing Encephalitis (ANE)
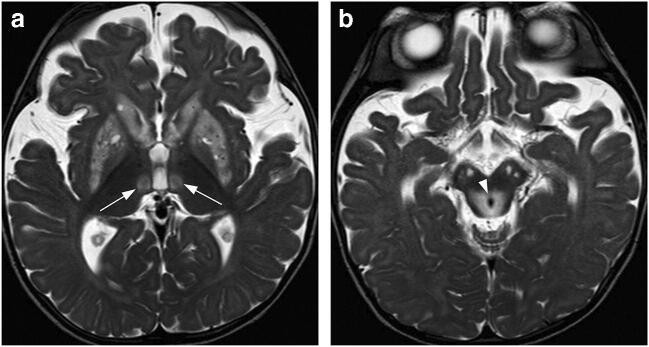
Acute necrotizing encephalitis (ANE), often associated with viral infections, is a rapidly progressive encephalopathy typically involving the thalami. Just as a rapid engine overheat causes critical damage, ANE causes rapid brain tissue necrosis. Characteristic MRI findings are bilateral symmetric hemorrhagic thalamic lesions with surrounding edema and variable diffusion.
Alt Text: Axial ADC map and GRE T2* MRI of a 2-year-old with acute necrotizing encephalitis showing bilateral thalamic hemorrhagic lesions and edema.
Vascular/Ischemic Disorders
Artery of Percheron Infarction
Artery of Percheron infarction results in bilateral thalamic infarcts due to occlusion of this single artery supplying the paramedian thalami. Like a blocked fuel line causing engine failure, artery occlusion causes brain tissue infarction. CT and MRI show bilateral paramedian thalamic hypodensity and T2/DWI hyperintensity with restricted diffusion. The “midbrain V sign” may also be present.
Alt Text: Axial CT, DWI, and ADC map of a 69-year-old with artery of Percheron infarction showing bilateral thalamic infarcts with restricted diffusion.
Alt Text: Axial CT of chronic artery of Percheron infarction showing bilateral thalamic CSF-like lesions representing resolved infarcts.
Deep Cerebral Venous Thrombosis (DCVT)
Deep cerebral venous thrombosis (DCVT) can lead to bilateral thalamic lesions due to venous congestion. Like a clogged coolant line causing engine overheat, venous thrombosis disrupts brain drainage. CT may show hyperdense veins and thalamic hypodensity or hemorrhage. MRI findings are variable but often show T2 hyperintensity and diffusion abnormality.
Alt Text: Axial and sagittal CT of a 6-month-old with deep cerebral venous thrombosis showing bilateral thalamic lesions and hyperdense thrombosed veins.
Alt Text: Axial T1 MRI and MR venography of a neonate with deep cerebral venous thrombosis showing bilateral thalamic swelling and absent venous flow.
Dural Arteriovenous Fistula (dAVF)
Dural arteriovenous fistula (dAVF) draining into the deep venous system can cause bilateral thalamic edema and dementia due to venous hypertension. Like a short circuit in a vehicle’s electrical system, dAVF disrupts normal brain blood flow. MRI shows bilateral thalamic T2 hyperintensity and increased diffusivity without hemorrhage or DCVT.
Neoplastic Disorders
Diffuse Midline Glioma/Thalamic Glioma
Diffuse midline gliomas, including thalamic gliomas, are aggressive tumors. Like identifying a major engine structural failure, thalamic gliomas represent a serious brain pathology. Bilateral thalamic gliomas show T2 hyperintensity and mass effect.
Alt Text: Axial T2 MRI and ADC map of a 44-year-old with bithalamic glioma showing bilateral thalamic masses with heterogeneous signal and mass effect.
Primary CNS Lymphoma (PCNSL)
Primary CNS lymphoma (PCNSL) can involve the medial thalami bilaterally. Similar to diagnosing a parasitic drain on a car battery, PCNSL represents an abnormal cellular proliferation. CT shows hyperdense lesions, and MRI shows T2 iso- to hypointense lesions with homogeneous enhancement and restricted diffusion.
Alt Text: Axial CT of a 46-year-old with primary CNS lymphoma showing bilateral thalamic hyperdense lesions, indicative of neoplastic infiltration.
Pathology Involving Both the Basal Ganglia and Thalami
Inherited Metabolic/Genetic Disorders
Tubulinopathies or Tubulin-Related Cortical Dysgenesis
Tubulinopathies, genetic brain malformations, affect deep gray matter structures. Like congenital defects in vehicle manufacturing, tubulinopathies represent developmental abnormalities. MRI shows dysmorphic basal ganglia and thalami, often with fused caudate and putamen and enlarged thalami.
Alt Text: Axial T1 MRI of a 10-year-old with tubulinopathy showing dysmorphic basal ganglia and thalami, characteristic of this developmental disorder.
Alt Text: Axial T2 MRI of a 1-month-old with tubulinopathy showing fused caudate and putamen, and dysmorphic thalami.
Neurofibromatosis Type 1 (NF-1)
Neurofibromatosis type 1 (NF-1) is a neurocutaneous syndrome associated with focal abnormal signal intensities (FASIs) in the brain. Like cosmetic blemishes on a car’s paint, FASIs in NF-1 are often benign but diagnostically relevant. MRI shows scattered T2 hyperintensities in the basal ganglia, thalami, brainstem, and cerebellum without mass effect or enhancement.
Alt Text: Axial FLAIR, T1, and T2 MRI of an 8-year-old with NF-1 showing bilateral basal ganglia and thalamic FASIs, characteristic of neurofibromatosis.
Alt Text: Axial T2 MRI showing asymmetric basal ganglia and thalamic FASIs in NF-1.
Primary Familial Brain Calcification (PFBC)
Primary familial brain calcification (PFBC), formerly Fahr disease, is characterized by abnormal calcium deposits in the basal ganglia and other brain regions. Like mineral deposits in a car’s cooling system, PFBC involves abnormal mineral accumulation in the brain. CT is best for detecting calcifications in the basal ganglia, thalami, and cerebellar dentate nuclei.
Alt Text: Axial CT of a 30-year-old with primary familial brain calcification showing extensive calcifications in the basal ganglia and thalami.
Alt Text: Sagittal T1 MRI of a 57-year-old with primary familial brain calcification showing calcifications in the basal ganglia and thalamus.
Acquired Metabolic/Toxic Disorders
Ethylene Glycol Intoxication
Ethylene glycol (EG) intoxication, often from antifreeze ingestion, is toxic to the brain. Like corrosive antifreeze damaging vehicle parts, EG is highly toxic to brain tissue. MRI shows symmetric T2 hyperintensity in the basal ganglia, thalami, and brainstem.
Alt Text: Axial FLAIR and T2 MRI of a 25-year-old with ethylene glycol intoxication showing bilateral basal ganglia and thalamic hyperintensity.
Osmotic Demyelination Syndrome (ODS)
Osmotic demyelination syndrome (ODS), often triggered by rapid correction of hyponatremia, can affect the basal ganglia and thalami. Like improper fluid balance causing vehicle system failure, rapid electrolyte shifts damage brain myelin. Extrapontine myelinolysis (EPM) in ODS shows symmetric T2 hyperintensity in the striatum, thalamus, and external capsule.
Alt Text: Axial T2 and T1 MRI of a 46-year-old with osmotic demyelination syndrome showing bilateral basal ganglia hyperintensity (EPM) and pontine lesion (CPM).
Alt Text: Axial CT of a 7-year-old with osmotic demyelination syndrome showing bilateral basal ganglia hypodensity.
Brain MRI Changes with Vigabatrin Therapy
Vigabatrin, an antiepileptic drug, can cause reversible MRI changes in infants. Like medication side effects in humans, certain drugs can have unintended imaging consequences. MRI shows symmetric T2 hyperintensity and restricted diffusion in the thalami, basal ganglia, brainstem, and cerebellar dentate nuclei.
Alt Text: Axial T2 MRI of a 50-week-old with vigabatrin-associated MRI changes showing bilateral thalamic and basal ganglia hyperintensity.
Alt Text: Axial ADC map and DWI of a 42-week-old with vigabatrin-associated MRI changes showing thalamic restricted diffusion and globus pallidus hyperintensity.
Endocrinological Disorders Related to Parathyroid Hormone Disturbances
Parathyroid hormone disturbances, particularly hypoparathyroidism, can cause bilateral intracranial calcifications. Like mineral scale buildup in pipes due to water chemistry imbalance, parathyroid disorders lead to abnormal calcium deposition in the brain. CT shows calcifications in the basal ganglia, thalami, and dentate nuclei.
Alt Text: Axial CT of a 28-year-old with hyperparathyroidism showing bilateral basal ganglia and dentate nuclei calcifications.
Infectious/Inflammatory Disorders
Creutzfeldt-Jakob Disease (CJD)
Creutzfeldt-Jakob disease (CJD), a prion disease, is a rapidly progressive neurodegenerative disorder. Like a rapidly spreading computer virus causing system crash, CJD is a devastating brain disease. MRI, especially DWI, shows cortical and deep gray matter hyperintensity, often asymmetrically, involving the basal ganglia and thalami. The “hockey stick” sign, involving the striatum and dorsomedial thalamus, is suggestive.
Alt Text: Axial DWI of a 69-year-old with Creutzfeldt-Jakob Disease showing bilateral striatal and thalamic hyperintensity (“hockey stick” sign) and cortical ribboning.
Alt Text: Axial DWI of a 61-year-old with Creutzfeldt-Jakob Disease showing bilateral basal ganglia, thalamic, and cortical hyperintensity.
Acute Disseminated Encephalomyelitis (ADEM)
Acute disseminated encephalomyelitis (ADEM), an immune-mediated inflammatory disease, can involve the brain and spinal cord. Like a system-wide software glitch causing malfunction, ADEM is a widespread brain inflammatory process. MRI shows asymmetric T2 hyperintensities in the white matter, basal ganglia, and thalami, often with variable enhancement.
Alt Text: Axial T2 MRI and ADC map of a 4-year-old with ADEM showing asymmetric thalamic and white matter hyperintensity and increased diffusivity.
Viral Encephalitis
Viral encephalitis can affect the gray matter, often involving the basal ganglia and thalami. Like a computer virus infecting multiple systems, viral encephalitis can broadly affect brain regions. MRI shows asymmetric T2 hyperintensity in the thalami and/or basal ganglia, often with cortical involvement.
Alt Text: Coronal FLAIR MRI of a 71-year-old with West Nile viral encephalitis showing right thalamic and cortical hyperintensity.
Alt Text: Axial FLAIR MRI of a 6-year-old with EBV viral encephalitis showing left caudate and putamen hyperintensity and cortical lesions.
Cerebral Toxoplasmosis
Cerebral toxoplasmosis, an opportunistic infection in immunocompromised patients, often affects the deep gray matter. Like parasitic infestation in a vehicle system, toxoplasmosis is an invasive infection. CT and MRI show enhancing lesions in the basal ganglia and corticomedullary junction, sometimes with the “eccentric target sign” or “concentric target sign”.
Alt Text: Axial post-contrast T1 MRI of a 32-year-old with cerebral toxoplasmosis showing an enhancing lesion in the basal ganglia with the “eccentric target” sign.
Alt Text: Axial FLAIR MRI of a 38-year-old with cerebral toxoplasmosis showing a lesion with the “concentric target” sign.
Vascular/Ischemic Disorders
Hypoxic-Ischemic Encephalopathy (HIE) and Status Marmoratus
Hypoxic-ischemic encephalopathy (HIE), from global hypoxia, severely affects the central gray matter. Like engine seizure from oil starvation, HIE is severe brain damage due to oxygen deprivation. MRI shows symmetric involvement of the basal ganglia and thalami with restricted diffusion acutely and T1 hyperintensity later. In neonates, the “absent posterior limb” sign is characteristic. Status marmoratus, a chronic sequela of HIE, shows a marbled appearance of the basal ganglia and thalami.
Alt Text: Axial DWI and ADC map of a 44-year-old with hypoxic-ischemic encephalopathy showing bilateral striatal, cortical, and thalamic hyperintensity with restricted diffusion.
Alt Text: Axial ADC map and T1 MRI of a term neonate with hypoxic-ischemic encephalopathy showing bilateral basal ganglia and thalamic restricted diffusion and “absent posterior limb” sign.
Alt Text: Axial T1 and T2 MRI of a 5-day-old term neonate with hypoxic-ischemic encephalopathy showing bilateral basal ganglia and thalamic signal changes.
Hypertensive Hematoma
Hypertensive hemorrhages commonly occur in the basal ganglia and thalami. Like pressure buildup causing hydraulic line rupture, hypertension can cause brain hemorrhage. CT in acute hypertensive hematoma shows hyperdense lesions in the putamen and thalamus. Bilateral hemorrhages are rare but possible. Chronic lesions evolve into slit-like cavities with hemosiderin staining.
Alt Text: Axial CT of a 75-year-old with hypertensive hematomas showing bilateral lentiform nucleus hemorrhages.
Alt Text: Axial CT and follow-up T2 MRI of a 59-year-old with hypertensive hematomas showing acute putaminal hemorrhages and chronic slit-like lesions.
Posterior Reversible Encephalopathy Syndrome (PRES)
Posterior reversible encephalopathy syndrome (PRES), often triggered by hypertension, causes vasogenic edema. Like fluid leaks in a pressurized system causing malfunction, PRES involves vascular dysregulation. MRI shows near-symmetric T2 hyperintensities in the posterior cerebral hemispheres, often involving the cortex. Basal ganglia and thalamic involvement is less common but can occur, especially in the “central variant” PRES.
Alt Text: Axial T2 MRI and ADC map of a 2-month-old with PRES showing bilateral parieto-occipital and basal ganglia hyperintensity with vasogenic edema.
Alt Text: Axial FLAIR MRI and ADC map of a 68-year-old with PRES “central variant” showing bilateral basal ganglia, thalamic, and periventricular white matter hyperintensity.
Conclusion
Diagnosing bilateral basal ganglia hyperintensity requires a systematic approach, integrating imaging findings with clinical and demographic data. Just as we use diagnostic tools and experience to pinpoint vehicle problems, a comprehensive understanding of imaging characteristics and clinical contexts is essential for differentiating the diverse causes of bilateral basal ganglia hyperintensity. Key considerations include lesion location, MRI signal characteristics, patient age, and clinical presentation (acute vs. chronic). By systematically analyzing these factors, we can narrow the differential diagnosis and guide appropriate management strategies.
Alt Text: Summary overview image of bilateral basal ganglia and thalamic pathologies and their characteristic imaging patterns for differential diagnosis.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of medical conditions.