Introduction
Experiencing pain in both hands can significantly hinder daily activities, from simple tasks to complex work. When bilateral hand pain arises, especially with symptoms like stiffness, swelling, and redness, differentiating between various underlying conditions becomes crucial for effective management and treatment. While several conditions can manifest as bilateral hand pain, osteoarthritis (OA) and rheumatoid arthritis (RA) are two of the most prevalent, yet distinctly different, causes. This article explores the diagnostic challenges posed by bilateral hand pain, particularly in distinguishing between hand OA and RA, and highlights the importance of a comprehensive differential diagnosis approach, including the use of diagnostic ultrasound. Understanding the nuances of each condition is paramount, as OA is often managed conservatively, while RA requires specialized rheumatological care and early intervention for optimal outcomes.
Clinical Presentation: When Hand Osteoarthritis Mimics Rheumatoid Arthritis
Hand osteoarthritis is a widespread condition, affecting a significant portion of the population over 60 years old and leading to pain and functional limitations. The underlying mechanisms of hand OA are multifaceted, involving not only mechanical wear and tear but also local and systemic inflammation. Risk factors for developing hand OA include aging, obesity, being female, and previous hand injuries.
Patients with hand OA commonly report activity-related pain, morning stiffness, joint swelling, bony enlargements (hypertrophy), and impaired hand function. These clinical signs, especially when present in both hands, can create diagnostic ambiguity, often mimicking inflammatory arthritides like rheumatoid arthritis. In such cases, relying solely on clinical examination might be insufficient, necessitating further investigations, including laboratory tests and imaging studies, to reach an accurate diagnosis.
Case Report: Unmasking Osteoarthritis with Ultrasound
Consider the case of a 48-year-old Hispanic woman presenting with a year-long history of bilateral hand pain, stiffness, swelling, and weakness affecting the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints. The pain, rated as severe, significantly impacted her ability to work as a house cleaner. Initial physical examination revealed redness and swelling in the IP joints bilaterally, accompanied by weakness in finger movements and pain upon palpation of the PIP and DIP joints.
Initial laboratory tests conducted a year prior showed no signs of inflammation (normal erythrocyte sedimentation rate and C-reactive protein, negative rheumatoid factor, and negative anti-nuclear antibodies). However, given the persistent symptoms and suspicion of inflammatory disease, radiographic imaging was performed. Previous radiographs of the left hand showed periarticular osteopenia and a possible erosion at the fifth metacarpal base (Fig 1A). Current bilateral hand radiographs revealed similar symmetrical findings in the right hand and no changes in the left hand (Figs 1B and C). Due to the inconclusive radiographic findings and the need to rule out inflammatory synovitis and erosions definitively, diagnostic ultrasound imaging was employed. The ultrasound examination revealed no evidence of synovitis or marginal erosions in the hand joints bilaterally (Figs 2A, B, C, and D). Based on these findings, a diagnosis of symptomatic hand osteoarthritis was established, rather than rheumatoid arthritis as initially considered.
Fig 1.
Posteroanterior radiograph of the left hand obtained May 12, 2017 (A), demonstrates periarticular osteopenia and a marginal erosion (arrow) at the base of the fifth metacarpal. Repeat posteroanterior radiograph of the left hand obtained August 9, 2017 (B), demonstrates no interval change of the findings. Posteroanterior radiograph of the right hand obtained August 9, 2017 (C), demonstrates symmetrical findings, including apparent erosion (arrow) at the fifth metacarpal.
Fig 2.
 Ultrasound images showing no synovitis or erosion in hand osteoarthritis
Ultrasound images showing no synovitis or erosion in hand osteoarthritis
Long-axis B-mode (A) and power Doppler (B) ultrasound images of the right metacarpophalangeal joint are normal, without evidence of bony erosion or synovitis. Long-axis B-mode (C) and power Doppler (D) ultrasound images of the right proximal interphalangeal joint are also normal.
Conservative Intervention and Positive Outcome
The patient underwent a course of conservative care, including manual joint mobilizations to the PIP and DIP joints, instrument-assisted soft tissue therapy targeting the same joints, and low-level laser therapy. She was also prescribed a home exercise program focusing on progressive finger extension and flexion exercises. After one month of treatment, the patient showed significant improvement. While some tenderness remained upon palpation, she regained full, pain-free finger range of motion and strength. Importantly, she reported no pain during daily activities and was able to return to her work as a house cleaner without limitations. No adverse effects were reported throughout the treatment.
Discussion: Navigating the Differential Diagnosis of Bilateral Hand Pain
Osteoarthritis is a highly prevalent rheumatologic condition in the United States, with hand OA being the second most common site after the knee. While rheumatoid arthritis is the most common inflammatory arthritis, it affects fewer people than OA. Both conditions are more common in women; however, RA typically manifests earlier in life, often in the third decade, whereas OA usually presents later, typically after age 50. In this case, the patient’s age and presentation with inflammatory-like symptoms and ambiguous radiographs made the initial differentiation challenging.
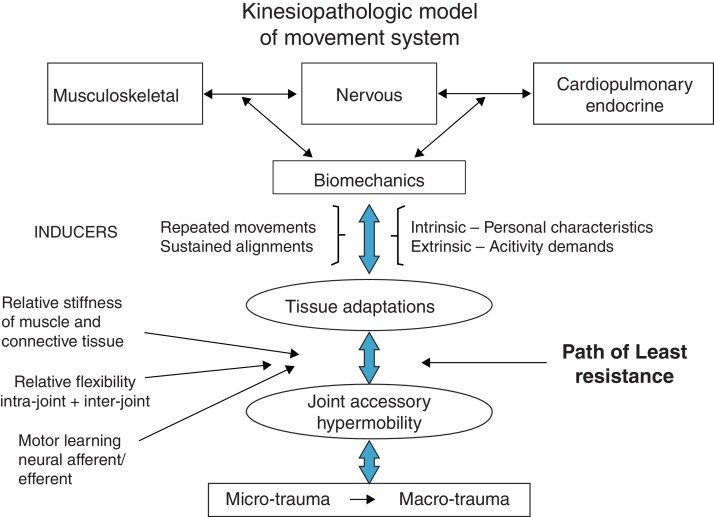
The underlying pathology of OA and RA differs significantly. OA is characterized by mechanical stress, anatomical changes, and both local and systemic inflammatory processes. These processes involve pro-inflammatory cytokines that contribute to cartilage breakdown, bone changes, and low-grade synovitis. Consequently, hand OA can present with symptoms that mimic inflammatory arthritis, such as pain, stiffness, swelling, and redness, creating diagnostic confusion with RA. Rheumatoid arthritis, on the other hand, is a systemic autoimmune disease primarily affecting the synovial lining of joints. It involves synovial hypertrophy, inflammatory cell infiltration, and pannus formation, leading to cartilage and bone destruction. Radiographic findings in this case, such as periarticular osteopenia and potential erosions, initially raised suspicion for RA. However, in the absence of supporting laboratory markers, further imaging was essential.
Risk factors for both OA and RA can overlap, including age, female gender, obesity, and family history of arthritis. Smoking is a risk factor specific to RA, while mechanical stress is more associated with OA. In this case, the patient had multiple shared risk factors, highlighting the necessity for comprehensive diagnostic workup beyond risk factor assessment.
The clinical features of hand OA and RA can also be overlapping and non-specific. Both conditions can have insidious or abrupt onset. Inflammatory features like morning stiffness (lasting over an hour), swelling, and redness can be seen in hand OA, mimicking RA. Bony enlargements in OA can be mistaken for the soft tissue pannus seen in RA. While functional limitations are generally more severe in RA, hand OA can still significantly impact daily life and work, particularly when grip strength and range of motion are compromised. Early RA may present with milder symptoms and no deformities, further complicating the differentiation from OA. The typical joint distribution differs, with OA commonly affecting DIP, PIP, and the first carpometacarpal joints, while RA typically involves PIP and metacarpophalangeal joints, although DIP involvement can occur in RA as well. The patient’s bilateral elbow pain, in addition to hand joint involvement, initially raised further concern for RA, although it ultimately resolved and was deemed non-specific.
Laboratory tests are not routinely required for diagnosing OA. In this case, the negative inflammatory markers did not exclude RA entirely, as rheumatoid factor can be negative in a significant proportion of RA patients, and inflammatory markers may be absent in early RA. Therefore, imaging became crucial. While radiographs showed periarticular osteopenia and questionable erosions, raising initial concerns for RA, these findings proved to be non-specific. The osteopenia was likely due to disuse, and the “erosions” were interpreted as anatomical variations rather than true inflammatory erosions.
Diagnostic ultrasound played a pivotal role in this case. It effectively ruled out synovitis and bone erosions, which are characteristic of RA, thus confirming the diagnosis of hand OA. Ultrasound is more sensitive than radiography in detecting synovitis and erosions, and it offers advantages such as wide availability, lower cost, no ionizing radiation, and the ability to compare both hands simultaneously.
The management strategies for hand OA and RA are distinctly different. Hand OA management focuses on symptom relief, as disease-modifying drugs are unavailable. In contrast, early diagnosis and rheumatology referral for RA are critical, as disease-modifying antirheumatic drugs can significantly improve outcomes and alter the disease course.
Conclusion
This case underscores the importance of considering hand osteoarthritis in the differential diagnosis of bilateral hand pain, even when inflammatory-like symptoms are present. Clinical features alone can be misleading, as symptoms traditionally associated with inflammatory arthritis can also manifest in OA. In cases with suspected inflammatory arthritis but negative or equivocal laboratory and radiographic findings, diagnostic ultrasound is a valuable tool to differentiate between hand OA and RA, guiding appropriate management strategies. Accurate differential diagnosis is crucial to ensure timely and effective treatment, directing patients with OA towards conservative management and patients with RA to rheumatological care for early intervention.
Practical Applications
- Symptomatic hand OA can present with clinical features that closely mimic rheumatoid arthritis, highlighting the challenges in differential diagnosis based on clinical presentation alone.
- In cases of bilateral hand pain with inflammatory features, a diagnostic strategy combining laboratory analysis and imaging, particularly diagnostic ultrasound, is essential to differentiate between osteoarthritis and rheumatoid arthritis effectively.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
- Concept development (provided idea for the research): K.L.L., P.J.B.
- Design (planned the methods to generate the results): K.L.L., P.J.B.
- Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): K.L.L., P.J.B.
- Literature search (performed the literature search): K.L.L., P.J.B.
- Writing (responsible for writing a substantive part of the manuscript): K.L.L., P.J.B.
- Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): K.L.L., P.J.B.