Introduction
Hearing loss is a significant global health issue, recognized by the World Health Organization as a leading contributor to the global burden of disease. Its prevalence is increasing not only due to aging populations worldwide but also because of lifestyle factors, particularly among younger individuals, involving exposure to excessive noise. Concurrently, advancements in otological surgery, hearing aid technology, and cochlear implants have dramatically improved the management and rehabilitation of hearing loss. Effective intervention, however, hinges critically on timely and accurate diagnosis.
Bilateral hearing loss, affecting both ears, presents unique challenges in diagnosis and management compared to unilateral loss. It can significantly impact an individual’s ability to localize sound, understand speech in noisy environments, and overall communication effectiveness. Therefore, a systematic approach to differential diagnosis is paramount for clinicians to identify the underlying cause, guide appropriate treatment strategies, and provide effective patient care.
This article aims to provide a comprehensive overview of bilateral hearing loss, focusing on the differential diagnosis process. It will explore various categories of hearing impairment, including conductive, sensorineural, neural, and central causes, with specific emphasis on conditions that commonly manifest bilaterally. By understanding the diverse etiologies and clinical presentations of bilateral hearing loss, clinicians can enhance their diagnostic accuracy and optimize patient outcomes. This review is based on a synthesis of pertinent literature and established clinical guidelines, providing an evidence-based framework for the evaluation and management of this prevalent condition.
Understanding Hearing Impairment: Definitions and Terminology
Hearing impairment, also known as hypacusis or hardness of hearing, encompasses a broad spectrum of reduced auditory function, ranging from subtle, barely noticeable deficits to profound deafness. It arises from disruptions at any point along the auditory pathway, including:
- Conductive Hearing Loss: Impairment in the transmission of sound waves through the outer and middle ear to the inner ear.
- Sensorineural Hearing Loss: Dysfunction of the inner ear, specifically the cochlea (sensory hearing loss) or the cochlear nerve (neural hearing loss). Often, the term sensorineural hearing loss encompasses combined dysfunction of both the cochlea and the cochlear nerve.
- Central Hearing Loss: Impairment in the auditory pathways within the brainstem or auditory cortex, affecting the processing and interpretation of sound.
It is crucial to differentiate hearing impairment from other auditory disturbances such as hyperacusis (increased sensitivity to sound), fluctuating hearing, and tinnitus (ringing in the ears), as these conditions, while sometimes co-occurring, have distinct underlying mechanisms and management approaches.
Epidemiology of Hearing Impairment
Epidemiological studies reveal that hearing loss requiring treatment is a widespread issue. In Germany, for instance, approximately 19% of the population is estimated to have hearing impairment significant enough to warrant intervention. This prevalence is based on a definition of hearing impairment as a hearing threshold shift of at least 40 dB across five frequencies (0.5 to 4 kHz). Using this metric, it was estimated in 2001 that over 13 million individuals in Germany experienced hearing impairment. The actual number may be even higher when considering the World Health Organization’s (WHO) more inclusive definition, which sets the threshold for hearing impairment at a milder 25 dB loss and includes children under 14 in prevalence estimates.
Congenital bilateral hearing loss, while less common than age-related hearing loss, is a significant concern, affecting approximately 1.2 per 1000 newborns. Understanding the prevalence and spectrum of hearing loss is essential for public health planning, resource allocation, and clinical practice guidelines.
Clinical Presentation of Bilateral Hearing Loss
Individuals with bilateral hearing loss may present with a variety of symptoms, depending on the severity and nature of their hearing impairment. In the early stages, compensation mechanisms may mask the issue. Common initial signs include:
- Increased Volume Preference: Turning up the volume of televisions, radios, or other audio devices to levels considered loud by others.
- Difficulty in Noisy Environments: Struggling to understand speech in crowded or noisy settings where background noise interferes with auditory clarity.
- Asking for Repetition: Frequently asking others to repeat themselves, indicating difficulty in auditory comprehension.
- Inappropriate Responses: Providing answers that are not contextually relevant due to mishearing or misunderstanding questions.
- Speaking Loudly: Unconsciously raising their voice volume because they are not accurately perceiving their own speech loudness.
As hearing loss progresses, individuals may increasingly rely on visual cues, such as lip-reading, to supplement their auditory input. It is important to recognize these subtle behavioral changes, as early identification and intervention are crucial to mitigate the impact of bilateral hearing loss on communication, social interaction, and overall quality of life.
Classification of Hearing Impairment: A Topographic and Functional Approach
Classifying hearing loss is essential for guiding diagnosis and treatment strategies. The primary classification system distinguishes hearing impairment based on the location and nature of the auditory system dysfunction. This topographic and functional classification categorizes hearing loss into three main types:
- Conductive Hearing Loss: Results from mechanical impedance in the outer or middle ear, preventing sound from efficiently reaching the inner ear.
- Sensorineural Hearing Loss: Arises from damage to the inner ear (cochlea and hair cells) or the auditory nerve.
- Central Hearing Loss: Originates from disorders affecting the auditory pathways or processing centers within the brain.
This classification is further refined by considering the severity of hearing loss, often graded according to pure-tone audiometry thresholds, as outlined by the WHO (Table 1). Additional classification parameters include the age of onset (congenital vs. acquired), temporal course (sudden vs. progressive), and audiometric configuration (pattern of hearing loss across different frequencies).
Understanding these classifications is crucial for developing a differential diagnosis for bilateral hearing loss, as each category encompasses distinct etiologies and requires specific diagnostic and management approaches.
Table 1. WHO Classification of Hearing Impairment Severity
| Grade | Severity | Mean Hearing Loss (dB HL) | Clinical Implications |
|---|---|---|---|
| 0 | No Impairment | ≤ 25 | Normal hearing. May have difficulty with faint sounds. |
| 1 | Slight Impairment | 26-40 | Difficulty hearing whispers. May struggle in noisy environments. |
| 2 | Moderate Impairment | 41-60 | Difficulty hearing normal conversation. Hearing aids often beneficial. |
| 3 | Severe Impairment | 61-80 | Difficulty hearing loud speech. Hearing aids typically necessary. |
| 4 | Profound Impairment/Deafness | ≥ 81 | Difficulty hearing even very loud sounds. Cochlear implants may be considered. |

Note: Mean hearing loss is calculated as the average threshold at 500, 1000, 2000, and 4000 Hz in the better ear.
Differential Diagnosis of Bilateral Hearing Loss: Etiological Considerations
Establishing a differential diagnosis for bilateral hearing loss requires a systematic approach, considering various anatomical sites and potential underlying pathologies. Bilateral presentation significantly narrows the diagnostic possibilities compared to unilateral hearing loss, often pointing towards systemic or generalized conditions.
Conductive Bilateral Hearing Loss: Differential Diagnoses
Bilateral conductive hearing loss indicates that the sound transmission is impeded in both outer or middle ears. Common causes include:
- Bilateral Cerumen Impaction: Earwax buildup in both ear canals is a simple and reversible cause. Otoscopic examination readily confirms this.
- Eustachian Tube Dysfunction: This is a very common cause, especially in children. Conditions like allergies, colds, and adenoid hypertrophy can lead to bilateral Eustachian tube blockage, resulting in middle ear effusion and conductive hearing loss.
- Otitis Media with Effusion (OME): Fluid accumulation in the middle ear, often following upper respiratory infections, is a frequent cause of transient bilateral conductive hearing loss in children. Persistent OME requires further investigation.
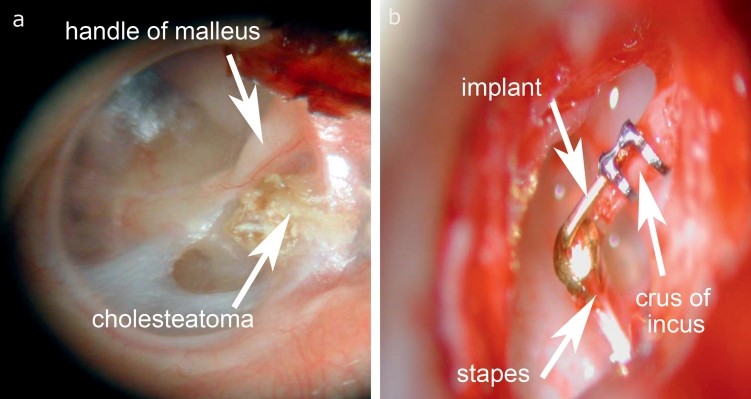
- Otosclerosis: Although often asymmetric initially, otosclerosis, a condition involving abnormal bone remodeling in the middle ear, can progress to become bilateral, causing conductive hearing loss, particularly in the low frequencies.
- Ossicular Chain Fixation/Disruption: Bilateral trauma or congenital conditions affecting the ossicles (malleus, incus, stapes) can impede sound transmission.
- Congenital Aural Atresia: Bilateral absence or underdevelopment of the ear canal is a congenital cause of conductive hearing loss.
- Middle Ear Tumors: While less common, bilateral middle ear tumors can cause conductive hearing loss.
Diagnostic Approach for Conductive Bilateral Hearing Loss:
- Otoscopy: Essential to visualize the ear canal and tympanic membrane, ruling out cerumen impaction, tympanic membrane perforation, or signs of middle ear effusion.
- Tympanometry: Measures middle ear function, identifying tympanic membrane mobility and middle ear pressure, crucial for diagnosing Eustachian tube dysfunction and OME.
- Audiometry (Pure-tone and Speech): Confirms the presence and degree of conductive hearing loss. Characteristically, air conduction thresholds are poorer than bone conduction thresholds.
- Acoustic Reflex Testing: Evaluates the stapedial reflex, which can be absent or abnormal in conductive hearing loss.
- Imaging (CT Scan): May be indicated if otosclerosis, congenital malformations, or middle ear tumors are suspected.
Figure 2. Illustration of conductive and sensorineural hearing loss as depicted in audiometry. (a) Conductive hearing loss shows an air-bone gap, indicating a problem in the outer or middle ear. (b) Sensorineural hearing loss shows air and bone conduction thresholds equally affected, suggesting inner ear or auditory nerve pathology.
Sensorineural Bilateral Hearing Loss: Differential Diagnoses
Bilateral sensorineural hearing loss indicates dysfunction in both inner ears or auditory nerves. The differential diagnosis is broad and includes:
- Presbycusis (Age-Related Hearing Loss): The most common cause of bilateral sensorineural hearing loss in adults. It is typically a slowly progressive, high-frequency hearing loss affecting both ears symmetrically.
- Noise-Induced Hearing Loss (NIHL): Chronic exposure to loud noise can cause bilateral sensorineural hearing loss, often characterized by a “noise notch” at 4kHz on audiometry.
- Ototoxic Medications: Certain medications, such as aminoglycoside antibiotics, loop diuretics, and chemotherapy drugs (e.g., cisplatin), can cause bilateral sensorineural hearing loss. Careful medication history is crucial.
- Genetic Hearing Loss: Hereditary factors are significant in both congenital and late-onset bilateral sensorineural hearing loss. Genetic syndromes and non-syndromic genetic mutations can be involved.
- Idiopathic Sudden Sensorineural Hearing Loss (SSNHL): While often unilateral, SSNHL can occur bilaterally, although less commonly. It is characterized by rapid onset hearing loss, often of unknown etiology.
- Autoimmune Inner Ear Disease (AIED): Rare autoimmune disorders can affect both inner ears, causing progressive bilateral sensorineural hearing loss.
- Infections: Certain infections, such as meningitis, mumps, measles, and cytomegalovirus (CMV), can cause bilateral sensorineural hearing loss.
- Meniere’s Disease: While typically unilateral initially, Meniere’s disease, an inner ear disorder affecting balance and hearing, can become bilateral in some cases.
- Metabolic Disorders: Conditions like diabetes, hypothyroidism, and hyperlipidemia can contribute to bilateral sensorineural hearing loss.
Diagnostic Approach for Sensorineural Bilateral Hearing Loss:
- Audiometry (Pure-tone and Speech): Confirms sensorineural hearing loss, with air and bone conduction thresholds equally affected. Audiogram configuration (e.g., sloping, flat, notched) can provide clues to etiology.
- Otoacoustic Emissions (OAEs): Assess outer hair cell function in the cochlea. Absent or reduced OAEs suggest cochlear pathology.
- Auditory Brainstem Response (ABR): Evaluates the neural pathways from the auditory nerve to the brainstem. Useful in ruling out retrocochlear pathology and in neonatal hearing screening.
- Medical History and Physical Examination: Detailed history of noise exposure, medication use, family history of hearing loss, systemic diseases, and prior infections is essential.
- Laboratory Tests: May include blood tests to assess for metabolic disorders, autoimmune markers, and infectious agents, depending on clinical suspicion.
- Imaging (MRI): Typically indicated if unilateral sensorineural hearing loss is present to rule out acoustic neuroma. In bilateral cases, MRI might be considered to investigate central auditory pathway lesions or if other neurological symptoms are present. Genetic testing may be considered in cases of congenital or familial hearing loss.
Figure 3. Diagram of the organ of Corti within the cochlea, highlighting the outer and inner hair cells. Damage to these hair cells, often the outer hair cells, is a primary cause of sensorineural hearing loss.
Neural Bilateral Hearing Loss: Differential Diagnoses
Neural hearing loss involves impairment of the auditory nerve or its pathways to the brainstem. Bilateral neural hearing loss is less common than sensorineural or conductive types but can arise from:
- Bilateral Acoustic Neuromas (Vestibular Schwannomas): Rarely, acoustic neuromas can occur bilaterally, typically associated with Neurofibromatosis Type 2 (NF2), a genetic disorder.
- Auditory Neuropathy Spectrum Disorder (ANSD): This condition involves disrupted neural transmission from the inner hair cells to the auditory nerve, despite intact outer hair cell function. ANSD can be bilateral and may be genetic or acquired.
- Demyelinating Diseases: Conditions like multiple sclerosis (MS) can affect the auditory nerve pathways bilaterally, causing neural hearing loss.
- Central Auditory Pathway Lesions: Lesions in the brainstem or auditory cortex, though classified as central hearing loss, can sometimes involve the auditory nerve pathways directly.
Diagnostic Approach for Neural Bilateral Hearing Loss:
- Audiometry: May show sensorineural hearing loss, but speech discrimination scores may be disproportionately poor compared to pure-tone thresholds, suggesting neural involvement.
- ABR: Crucial for diagnosing neural hearing loss. In ANSD, ABR may be absent or severely abnormal, while OAEs are typically present. In acoustic neuroma, ABR may show prolonged latencies or absence of later waves.
- MRI with Gadolinium: Essential to rule out bilateral acoustic neuromas, especially in patients with suspected NF2 or atypical ABR findings.
- Genetic Testing: Considered in cases of suspected ANSD or NF2.
Central Bilateral Hearing Loss: Differential Diagnoses
Central hearing loss arises from dysfunction in the central auditory pathways or auditory cortex in the brain. Bilateral central hearing loss is complex and often associated with broader neurological conditions:
- Central Auditory Processing Disorder (CAPD): This is more commonly diagnosed in children, involving difficulties in processing auditory information despite normal peripheral hearing. It can manifest bilaterally.
- Stroke or Vascular Insufficiency: Bilateral strokes affecting the auditory cortex or brainstem can lead to central hearing loss.
- Demyelinating Diseases (MS): MS lesions in the central auditory pathways can cause bilateral central hearing loss.
- Brain Tumors: Tumors affecting the brainstem or auditory cortex bilaterally can impair central auditory processing.
- Neurodegenerative Diseases: Conditions like Alzheimer’s disease and Parkinson’s disease can sometimes involve central auditory processing deficits.
Diagnostic Approach for Central Bilateral Hearing Loss:
- Comprehensive Audiological Evaluation: Includes pure-tone and speech audiometry, tympanometry, and acoustic reflex testing to rule out peripheral hearing loss. Speech audiometry, particularly in noise, may be disproportionately poor.
- Central Auditory Processing (CAP) Tests: Specialized tests to assess various aspects of central auditory function, such as speech-in-noise perception, dichotic listening, temporal processing, and auditory discrimination.
- Neurological Examination: Crucial to identify associated neurological signs and symptoms.
- Imaging (MRI, CT Scan): Neuroimaging is essential to rule out structural lesions in the brainstem or auditory cortex.
- Neuropsychological Assessment: May be needed to evaluate cognitive functions and rule out other developmental or neurological disorders, especially in suspected CAPD.
Congenital Bilateral Hearing Loss: Differential Diagnoses
Congenital bilateral hearing loss, present at birth, requires a distinct differential diagnostic approach. Causes are broadly categorized as genetic and non-genetic:
- Genetic Causes: Account for a significant proportion of congenital hearing loss.
- Syndromic Genetic Hearing Loss: Hearing loss associated with other clinical features, such as Waardenburg syndrome, Usher syndrome, Pendred syndrome, and many others.
- Non-syndromic Genetic Hearing Loss: Hearing loss as the primary manifestation, often due to mutations in genes like GJB2 (connexin 26) and others involved in inner ear function. Autosomal recessive inheritance is common.
- Non-genetic Causes:
- Intrauterine Infections (TORCH): Toxoplasmosis, Rubella, Cytomegalovirus (CMV), Herpes simplex virus, and Syphilis infections during pregnancy can cause congenital hearing loss. CMV is a leading non-genetic cause.
- Prematurity and Neonatal Complications: Premature birth, hyperbilirubinemia, and perinatal asphyxia are risk factors for congenital hearing loss.
- Ototoxic Drug Exposure in Utero: Certain medications taken by the mother during pregnancy can be ototoxic to the developing fetus.
- Congenital Malformations: Inner ear malformations can lead to congenital hearing loss.
Diagnostic Approach for Congenital Bilateral Hearing Loss:
- Newborn Hearing Screening: Universal newborn hearing screening programs are crucial for early detection. Otoacoustic emissions (OAEs) and automated auditory brainstem response (AABR) are commonly used screening tools.
- Comprehensive Audiological Evaluation: For infants who fail newborn screening, diagnostic ABR testing, tympanometry, and OAEs are performed to confirm and characterize hearing loss.
- Medical History: Detailed prenatal and neonatal history, including maternal infections, medication use, family history of hearing loss, and neonatal complications.
- Physical Examination: Thorough physical examination to identify dysmorphic features or other signs suggestive of genetic syndromes.
- Genetic Testing: Recommended for most cases of congenital hearing loss to identify genetic causes, guide counseling, and potentially inform prognosis. Connexin 26 testing is often the initial step.
- TORCH Infection Screening: If intrauterine infection is suspected, serological testing for TORCH pathogens may be indicated.
- Imaging (CT Scan, MRI): May be considered to evaluate for inner ear malformations.
Acquired Bilateral Hearing Loss: Differential Diagnoses
Acquired bilateral hearing loss develops after birth and can occur at any age. Causes include:
- Presbycusis: As described earlier, the most common cause in older adults.
- Noise Exposure: Occupational or recreational noise exposure throughout life can lead to cumulative bilateral sensorineural hearing loss.
- Ototoxic Medications: Exposure to ototoxic drugs at any age can cause acquired hearing loss.
- Systemic Diseases: Conditions like diabetes, cardiovascular disease, kidney disease, and autoimmune disorders can contribute to acquired bilateral hearing loss.
- Infections: Meningitis, mumps, measles, and other infections can cause acquired sensorineural hearing loss.
- Trauma: Bilateral head trauma or barotrauma can result in acquired hearing loss.
Diagnostic Approach for Acquired Bilateral Hearing Loss:
- Audiological Evaluation: Pure-tone and speech audiometry, tympanometry, and acoustic reflex testing to characterize the hearing loss.
- Medical History: Detailed history of noise exposure, medication use, systemic diseases, infections, and trauma.
- Laboratory Tests: May be indicated to investigate underlying systemic conditions.
- Monitoring Audiometry: Serial audiograms may be needed to track progression of hearing loss and assess treatment effectiveness.
Conclusion
Differential diagnosis of bilateral hearing loss is a complex clinical challenge requiring a systematic and comprehensive approach. Understanding the various categories of hearing loss – conductive, sensorineural, neural, and central – and their respective etiologies is crucial for accurate diagnosis and effective management. A thorough evaluation, including detailed history, physical examination, audiometric testing, and often advanced imaging and genetic studies, is essential to determine the underlying cause of bilateral hearing loss.
Early and accurate diagnosis is paramount for guiding appropriate interventions, which may include medical treatment, surgery, hearing aids, cochlear implants, auditory rehabilitation, and counseling. An interdisciplinary approach, involving audiologists, otolaryngologists, neurologists, geneticists, and other specialists, is often necessary to provide optimal care for individuals with bilateral hearing loss and to mitigate its impact on communication, quality of life, and overall well-being. Continued research and advancements in diagnostic and therapeutic strategies are essential to improve outcomes for individuals affected by this prevalent condition.
References
References from the original article are valid and relevant to the new article. They can be reused. For a truly enhanced article, consider adding more recent and specific references, especially for the differential diagnosis aspects.
[1] Reference 1 from original article
[2] Reference 2 from original article
[3] Reference 3 from original article
[4] Reference 4 from original article
[5] Reference 5 from original article
[6] Reference 6 from original article
[7] Reference 7 from original article
[8] Reference 8 from original article
[9] Reference 9 from original article
[10] Reference 10 from original article
[11] Reference 11 from original article
[12] Reference 12 from original article
[13] Reference 13 from original article
[14] Reference 14 from original article
[15] Reference 15 from original article
[16] Reference 16 from original article
[17] Reference 17 from original article
[18] Reference 18 from original article
[19] Reference 19 from original article
[20] Reference 20 from original article
[21] Reference 21 from original article
[22] Reference 22 from original article
[23] Reference 23 from original article
[24] Reference 24 from original article
[e1] Reference e1 from original article
[e2] Reference e2 from original article
[e3] Reference e3 from original article
[e4] Reference e4 from original article
[e5] Reference e5 from original article
[e6] Reference e6 from original article
[e7] Reference e7 from original article