Understanding Bilateral Leg Swelling
Bilateral leg swelling, also known as edema, refers to the palpable swelling in both legs due to an expansion of the interstitial fluid volume. This condition arises when there’s an imbalance in fluid movement between blood vessels and tissues, or when the body retains excessive sodium and water. Clinically evident edema typically requires an increase of 2.5 to 3 liters in interstitial volume. Identifying the underlying cause of bilateral leg swelling is crucial for effective management. This article provides a comprehensive overview of the differential diagnosis and diagnostic process for bilateral leg swelling, aimed at healthcare professionals.
Diagnostic Process for Bilateral Leg Swelling
When evaluating a patient with bilateral leg swelling, a systematic approach is essential to narrow down the potential etiologies. The diagnostic process involves considering the acuity of the swelling (acute vs. chronic) and ruling out life-threatening conditions such as bilateral deep vein thrombosis (DVT).
Table 1: Possible Etiologies of Leg Edema in Adult Patients
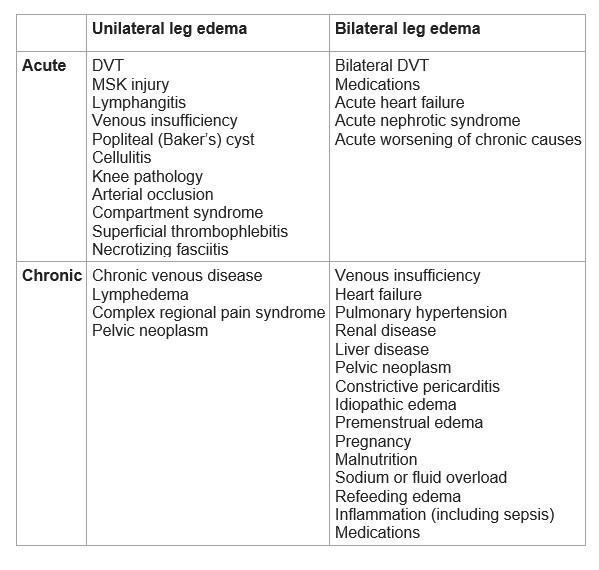 Table 1: Possible etiologies of leg edema in adult patients
Table 1: Possible etiologies of leg edema in adult patients
Acute Bilateral Leg Edema
Acute onset of bilateral leg swelling requires prompt evaluation to identify and manage potentially serious underlying conditions.
1. Rule out Bilateral Deep Vein Thrombosis (DVT):
Although less common than unilateral DVT, bilateral DVT can occur, especially in association with malignancy. If there is a high pre-test probability of DVT, Doppler ultrasound of the legs should be performed immediately to evaluate for thrombi.
2. Medication Review:
Certain medications are known to cause or exacerbate edema. A thorough medication history is crucial. Common culprits include:
- Dihydropyridine Calcium Channel Blockers (CCBs): Amlodipine, nifedipine, felodipine. These agents can cause peripheral vasodilation, leading to increased capillary hydrostatic pressure and edema.
- Vasodilators: Minoxidil, hydralazine. Similar to CCBs, these can contribute to edema through vasodilation.
- Hormone Therapies: Estrogen and progesterone-containing medications, including hormone replacement therapy and oral contraceptives, can lead to sodium and water retention.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs can impair renal function and promote sodium and water retention.
- Thiazolidinediones (TZDs): Pioglitazone, rosiglitazone. These antidiabetic drugs can cause fluid retention and edema.
Discontinuation or substitution of these medications should be considered if they are deemed to be contributing to the edema, after careful consideration of the risks and benefits.
3. Heart Failure:
Acute worsening of heart failure is a significant cause of acute bilateral leg edema. Assess for signs and symptoms of heart failure:
- History: Previous diagnosis of heart failure, coronary artery disease, hypertension, valvular heart disease.
- Physical Examination: Elevated jugular venous pressure (JVP), S3 gallop, displaced apical impulse, pulmonary rales, cardiomegaly.
- Investigations:
- Chest X-ray (CXR): To assess for cardiomegaly, pulmonary edema, and pleural effusions.
- Brain Natriuretic Peptide (BNP) or N-terminal pro-BNP (NT-proBNP): Elevated levels strongly support the diagnosis of heart failure.
- Echocardiography: To evaluate cardiac function, valve abnormalities, and structural heart disease.
- Point-of-Care Ultrasound (POCUS): In the emergency department, POCUS can be a rapid tool to assess for B-lines indicating pulmonary edema and to evaluate cardiac function.
4. Nephrotic Syndrome:
Acute nephrotic syndrome can lead to rapid onset of bilateral edema due to significant protein loss in the urine, resulting in decreased plasma oncotic pressure.
- Urine Dipstick: Test for proteinuria. A positive result warrants further investigation.
- Urine Protein-Creatinine Ratio (PCR) or 24-hour urine protein: To quantify the degree of proteinuria.
- Serum Albumin: Hypoalbuminemia is a hallmark of nephrotic syndrome.
Chronic Bilateral Leg Edema
Chronic bilateral leg edema develops gradually over time and is often associated with systemic conditions.
1. Chronic Venous Disease:
Chronic venous insufficiency is the most common cause of chronic bilateral leg edema. It results from impaired venous return, leading to increased hydrostatic pressure in the lower extremities.
- History: Varicose veins, history of deep vein thrombosis, symptoms worsen with prolonged standing or sitting and improve with leg elevation.
- Physical Examination: Hyperpigmentation (especially around the ankles), stasis dermatitis, venous ulcers, varicosities, induration.
2. Heart Failure:
Chronic heart failure is a frequent cause of chronic bilateral leg edema.
- History: Chronic dyspnea, orthopnea, paroxysmal nocturnal dyspnea (PND), fatigue, abdominal distention, known heart failure.
- Physical Examination: Signs of chronic heart failure as mentioned in acute bilateral edema, but often less pronounced in stable chronic heart failure.
3. Pulmonary Hypertension:
Pulmonary hypertension, particularly when caused by conditions like sleep apnea or chronic obstructive pulmonary disease (COPD), can lead to right heart failure and subsequent bilateral leg edema.
- History: Excessive daytime sleepiness, loud snoring, witnessed apneas during sleep (suggestive of sleep apnea), underlying lung disease.
- Physical Examination: Signs of right heart failure, such as elevated JVP, hepatomegaly, and potentially cyanosis.
4. Renal Disease:
Chronic kidney disease can cause bilateral edema through various mechanisms, including fluid and sodium retention and proteinuria.
- History: Known chronic kidney disease, diabetes, hypertension, family history of kidney disease.
- Investigations:
- Urine Dipstick and Urinalysis: To assess for proteinuria and other signs of renal disease.
- Serum Creatinine and Estimated Glomerular Filtration Rate (eGFR): To evaluate kidney function.
- Serum Albumin: May be low in nephrotic syndrome or advanced kidney disease.
5. Liver Disease:
Advanced liver disease (cirrhosis) can lead to bilateral edema due to decreased albumin synthesis (hypoalbuminemia) and portal hypertension.
- History: Known liver disease, alcohol abuse, viral hepatitis, jaundice, abdominal distention (ascites).
- Physical Examination: Jaundice, ascites, hepatomegaly, splenomegaly, spider angiomata, palmar erythema.
- Liver Function Tests (LFTs): Elevated bilirubin, transaminases (AST, ALT), alkaline phosphatase, and decreased albumin.
- Prothrombin Time/International Normalized Ratio (PT/INR): Prolonged PT/INR indicates impaired liver synthetic function.
6. Pelvic Neoplasm:
Pelvic tumors can obstruct venous and lymphatic drainage, leading to bilateral leg edema, although this is less common. Consider this especially if edema is unexplained and associated with other concerning symptoms.
- History: Unexplained weight loss, pelvic pain, changes in bowel or bladder habits.
- Imaging: CT pelvis with contrast may be necessary to rule out pelvic masses if other causes are not identified.
7. Constrictive Pericarditis:
Constrictive pericarditis is a rare condition where the pericardium becomes thickened and rigid, impairing cardiac filling and leading to systemic venous congestion and bilateral edema.
- History: Previous pericarditis, chest radiation, tuberculosis.
- Physical Examination: Elevated JVP with prominent y descent (Kussmaul’s sign), pericardial knock, signs of right heart failure.
- Echocardiography: May show thickened pericardium and diastolic dysfunction.
8. Idiopathic Edema:
In some cases, bilateral leg edema may be idiopathic, meaning no identifiable underlying cause is found after thorough evaluation. This diagnosis is made after excluding other potential etiologies.
9. Premenstrual Edema:
Hormonal fluctuations during the menstrual cycle can cause mild, cyclical edema in some women. This is typically benign and resolves spontaneously.
10. Malnutrition:
Severe malnutrition, particularly protein deficiency, can lead to decreased oncotic pressure and bilateral edema (nutritional edema).
11. Myxedema (Severe Hypothyroidism):
While technically not true edema, myxedema associated with severe hypothyroidism can cause non-pitting swelling, often in the lower legs, along with other signs and symptoms of hypothyroidism.
Initial Investigations for Chronic Bilateral Leg Edema
If the history and physical examination do not clearly point to a specific etiology for chronic bilateral leg edema, initial investigations should include:
- Urine Dipstick for Protein: To screen for proteinuria.
- Serum Creatinine: To assess renal function.
- Serum Albumin: To evaluate for hypoalbuminemia.
- Liver Function Tests (LFTs): To assess liver function.
- Thyroid Stimulating Hormone (TSH): To rule out hypothyroidism.
- PT/INR: To assess liver synthetic function.
If these initial tests are unremarkable, further investigations may be warranted:
- Echocardiogram: To evaluate for heart failure or pulmonary hypertension.
- CT Pelvis with Contrast: To exclude pelvic neoplasm, particularly if other investigations are negative and there are suggestive symptoms.
Quality of Evidence
The diagnostic approach and etiologies discussed are based on clinical experience, observational studies, and expert consensus. The quality of evidence is generally considered moderate, as it is derived from a range of studies addressing the diagnosis of leg edema, with reasonable agreement among them, although some studies may have limitations and variations.
Conclusion
Bilateral leg swelling is a common clinical presentation with a broad differential diagnosis ranging from benign to life-threatening conditions. A systematic diagnostic approach, including a thorough history, physical examination, and appropriate investigations, is crucial to identify the underlying cause and guide management. Ruling out serious conditions such as heart failure, renal disease, liver disease, and DVT is paramount. Understanding the potential etiologies and diagnostic pathways for bilateral leg edema allows healthcare professionals to provide timely and effective care for their patients.
Reference List
- GarcÃa, Jorge Pedraza, et al. “Comparison of the accuracy of emergency department-performed point-of-care-ultrasound (POCUS) in the diagnosis of lower-extremity deep vein thrombosis.” The Journal of emergency medicine 54.5 (2018): 656-664.
- Hull R, Hirsh J, Sackett DL, et al. Clinical validity of a negative venogram in patients with clinically suspected venous thrombosis. Circulation 1981; 64:622.
- Gorman WP, Davis KR, Donnelly R. ABC of arterial and venous disease. Swollen lower limb-1: general assessment and deep vein thrombosis. BMJ 2000; 320:1453.
- Chiesa R, Marone EM, Limoni C, et al. Chronic venous disorders: correlation between visible signs, symptoms, and presence of functional disease. J Vasc Surg 2007; 46:322.
- Executive Committee of the International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology 2020; 53:3.
- Marinus J, Moseley GL, Birklein F, et al. Clinical features and pathophysiology of complex regional pain syndrome. Lancet Neurol 2011; 10:637.
- Blankfield RP, Finkelhor RS, Alexander JJ, et al. Etiology and diagnosis of bilateral leg edema in primary care. Am J Med 1998; 105:192.