Introduction
Bilothorax, characterized by the presence of bile within the pleural space, is an infrequent cause of exudative pleural effusion. While most reported instances involve the right hemithorax, bilateral presentations are exceedingly rare. Typically, bilothorax arises secondary to biliary obstruction, the spread of hepatic infections, or iatrogenic complications stemming from percutaneous procedures or surgical interventions affecting the biliary system. Accurate diagnosis hinges on imaging studies and diagnostic pleural fluid analysis. Early identification and thorough drainage are critical to avert severe, potentially life-threatening complications, notably empyema formation. This article delves into the complexities of Bilothorax Diagnosis, enriched by a detailed case report of a 71-year-old female who developed bilateral bilothorax as a consequence of gallstone pancreatitis, providing a comprehensive understanding for clinicians and medical professionals.
Case Presentation: A Bilateral Bilothorax Case Study
A 71-year-old woman, classified as obese, was admitted to the hospital exhibiting acute abdominal pain, accompanied by chills and fever of 24-hour duration. The pain was described as sharp and shooting, initially localized in the right upper abdomen before radiating to both shoulder joints. Nausea and a single episode of bilious vomiting were also reported. Notably, she denied experiencing cough, chest pain, or urinary symptoms. Her background included retirement as a schoolteacher, a non-smoker status, and no reported excessive alcohol consumption. Her medical history was unremarkable for prior abdominal surgeries.
Upon examination, the patient was afebrile with stable vital signs. Auscultation of the lungs revealed clear breath sounds. However, significant tenderness in the right upper quadrant, guarding, and a positive Murphy’s sign were elicited upon palpation. Laboratory investigations revealed elevated lipase and bilirubin levels (Table 1).
Table 1. Patient Laboratory Values on Admission and Day 3
| Laboratory values (reference range) | Day of admission | Repeat labs (Day 3) |
|---|---|---|
| White Blood Cell Count (WBC) (4.0- 11.0 k/mm3 ) | 11.6 k/mm3 | 9.1 k /mm3 |
| Alkaline Phosphatase (ALP) (35-104 units/L) | 224 units/L | 95 units/L |
| Lipase (13-60 units/L) | 4510 units/L | 114 units/L |
| Aspartate Aminotransferase (AST) (0-32 units/L) | 122 units/L | 21 units/L |
| Alanine Transaminase (ALT) (0-33 units/L) | 227 units/L | 43 units/L |
| Total Bilirubin (0-1.2 mg/dl) | 5.9 mg/dl | 1.4 mg/dl |
| Direct Bilirubin (0-0.3 mg/dl) | 4.1 mg/dl | 1.0 mg/dl |

Initial right upper quadrant ultrasound (US) imaging demonstrated multiple gallstones and gallbladder wall thickening of 8 mm, findings consistent with acute cholecystitis. The common bile duct was noted to be dilated, measuring 0.8 cm. Intravenous fluids and piperacillin-tazobactam were promptly administered. Subsequently, percutaneous cholecystostomy tube placement, guided by interventional radiology, was performed. Repeat US confirmed successful decompression of the distended gallbladder. Liver function tests and lipase levels showed rapid improvement following these interventions (Table 1).
However, the patient’s clinical course took a turn as she developed acute respiratory distress, necessitating intubation for hypoxemic respiratory failure. A subsequent non-contrast computed tomography (CT) scan of the chest revealed bilateral moderate to large pleural effusions. Diagnostic thoracentesis was performed on the left side, yielding 300 ml of cloudy, greenish fluid (Figure 1), suggestive of bilothorax.
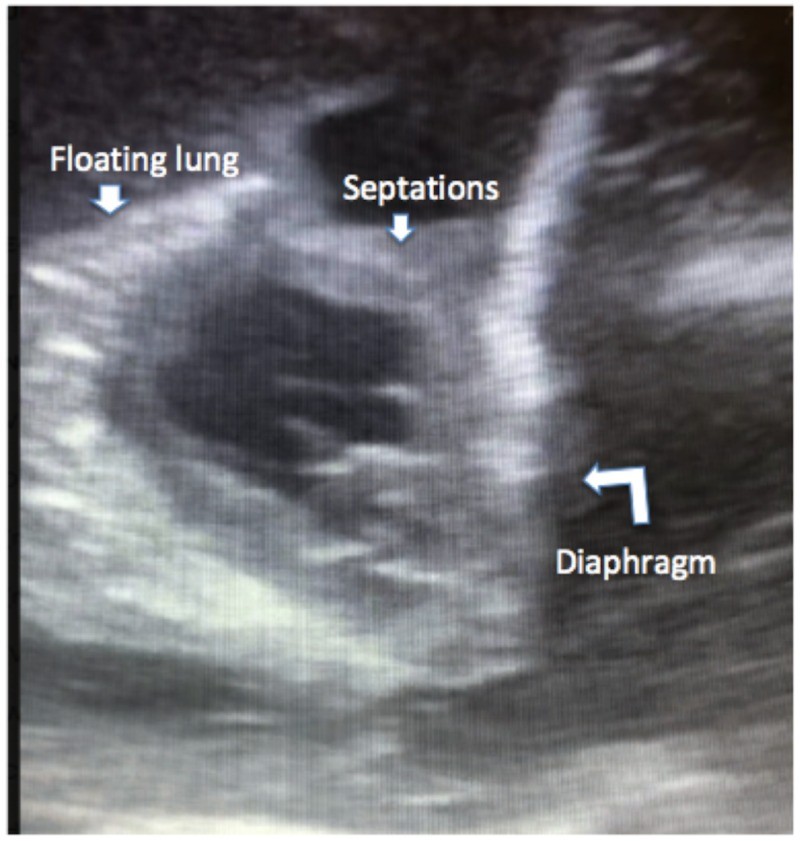
Bedside ultrasound of the right chest revealed a complex fluid collection with septations (Figure 2), further indicating pleural involvement on the contralateral side.
Right-sided chest tube insertion resulted in immediate drainage of 1700 ml of cloudy, green-colored fluid. A left-sided chest tube was also placed, draining an additional 450 ml of similar fluid. Pleural fluid analysis confirmed an exudative effusion based on Light’s criteria (Table 2).
Table 2. Pleural Fluid Analysis from Right and Left Sides
| Pleural fluid analysis | Right side | Left side |
|---|---|---|
| White Blood Cell Count (WBC) (per cc3) | 288 | 771 |
| pH | 7.62 | 7.37 |
| Pleural Fluid / Serum Protein (gm/dl) | 2.4 / 4.8 | 2.9 / 4.8 |
| Glucose (mg/dl) | 57 | 98 |
| Pleural Fluid / Serum Lactate Dehydrogenase (LDH) (units/ L) | 2,781 / 376 | 2,810 / 376 |
| Bilirubin (mg/dl) | 4.7 | 9.1 |
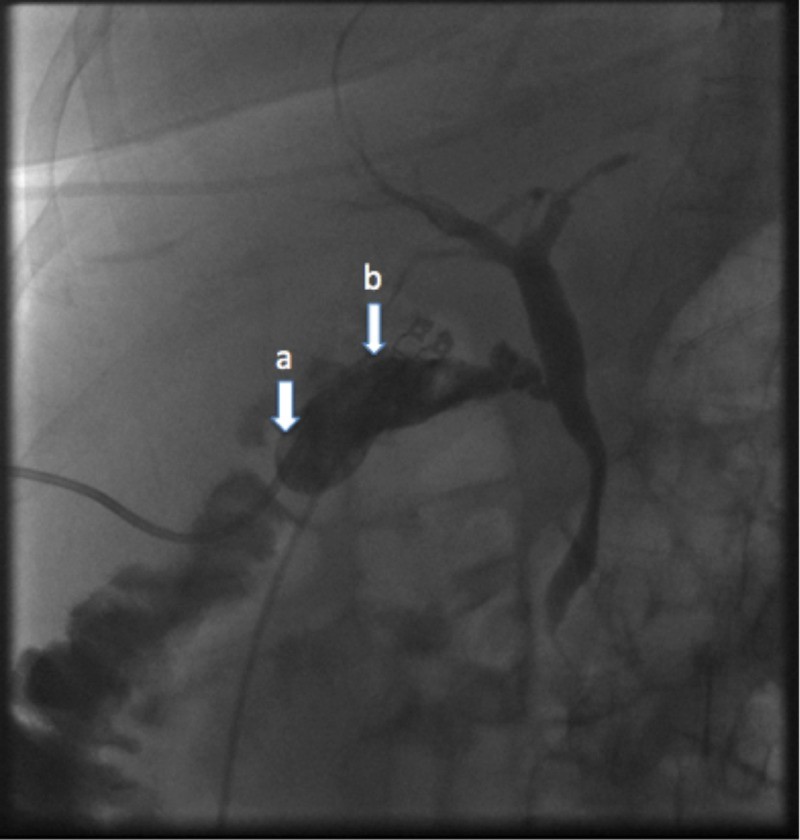
The pleural fluid to serum total bilirubin ratio was significantly elevated on both sides: 3.9 on the right (4.7: 1.2 mg/dl) and 7.5 on the left (9.1:1.2 mg/dl). Microbiology cultures of the pleural fluid were negative. Based on the pleural fluid bilirubin ratios exceeding 1.0 bilaterally, a diagnosis of bilateral bilothorax was established. The clinical context of acute cholecystitis and recent percutaneous procedure prompted consideration of differential diagnoses, including extension of a subphrenic abscess, gastric perforation, and iatrogenic biliary fistula formation. Further investigations, encompassing abdominal CT, upper gastrointestinal (GI) series, hepatobiliary iminodiacetic acid (HIDA) scan, and cholecystogram (Figure 3), were conducted but yielded no definitive findings to support these alternative diagnoses.
On the third day post-chest tube insertion, reduced drainage from the left-sided tube was observed, accompanied by persistent radiographic evidence of a moderate pleural effusion. To address this, 10 mg of alteplase in 40 ml of normal saline was instilled into the left pleural space via the chest tube, resulting in the immediate drainage of 1200 cc of pleural fluid (Figure 4).
Both chest tubes continued to drain effectively and were removed on Day 6, with chest X-rays showing complete resolution of the pleural effusions. The patient was successfully extubated and discharged home with the cholecystostomy tube in place. Four months post-discharge, she underwent a laparoscopic cholecystectomy. The procedure was well-tolerated, and she was discharged home after a smooth recovery.
Discussion: Diagnostic Approaches and Pathophysiology of Bilothorax
The mechanisms by which bile gains access to the pleural space are varied. Potential pathways include passive migration of bile across the diaphragm or through lymphatic channels, diaphragmatic defects of traumatic or congenital origin, and the formation of bilious fistulas. Other recognized etiologies encompass the extension of biliary peritonitis, blunt trauma leading to biliopleural fistula formation, or complications arising from open or percutaneous hepatobiliary interventions. In the context of bilothorax diagnosis, a high degree of clinical suspicion is paramount.
Initial diagnosis of pleural effusion typically involves physical examination and conventional imaging modalities such as chest X-ray, ultrasound, and CT scans. However, definitive bilothorax diagnosis necessitates pleural fluid analysis. The most diagnostically specific marker is a pleural fluid-to-serum bilirubin ratio exceeding 1.0. Once bilothorax is confirmed, elucidating the source of bile leakage into the pleural space becomes the subsequent critical step. Various diagnostic tools have been employed to investigate the etiology of bilothorax, including HIDA scans to pinpoint biliary leaks. In select cases, exploratory laparotomy has been considered as a diagnostic and potentially therapeutic approach, particularly when surgically correctable fistulas are suspected.
In this particular case, the patient’s initial presentation with acute cholecystitis prompted an abdominal CT scan to exclude a subphrenic abscess. A cholecystogram was performed to investigate potential bilious fistula formation. Given the negative findings from these investigations and the absence of any identifiable anatomical defect, we postulate that the bilateral bilothorax in this patient resulted from the passive movement of bile across the diaphragm or through lymphatic channels, exacerbated by the setting of obstructive jaundice secondary to gallstone pancreatitis.
The observed decrease in drainage from the left-sided chest tube prompted repeat imaging, which confirmed appropriate chest tube positioning. To enhance drainage, alteplase, a tissue plasminogen activator, was administered intrapleurally. This strategy aligns with reports by Zuckerman et al., who demonstrated the efficacy and safety of tissue plasminogen activator in managing complex pleural effusions without increasing hemorrhagic risks.
Currently, definitive guidelines for bilothorax management are lacking. Standard management principles emphasize immediate and complete drainage, given the heightened risk of empyema associated with bilothorax. This case underscores the importance of considering bilothorax in the differential diagnosis of pleural effusions, especially in patients with biliary pathology.
Conclusion: Key Takeaways for Bilothorax Diagnosis
Bilateral bilothorax, while a rare clinical entity, should be considered in the differential diagnosis of pleural effusions, particularly in patients with underlying biliary disease or a history of hepatobiliary procedures. A high index of clinical suspicion combined with pleural fluid bilirubin analysis is crucial for accurate bilothorax diagnosis. Prompt diagnosis, addressing the underlying cause, and ensuring complete pleural drainage are essential components of successful management, minimizing the risk of complications and improving patient outcomes. Further research and case studies are needed to refine diagnostic and therapeutic strategies for this rare condition and establish standardized management protocols for bilothorax diagnosis and treatment.
References
