Blepharospasm is a neurological movement disorder characterized by involuntary and forceful contractions of the muscles around the eyes, leading to excessive blinking, squinting, and in severe cases, eyelid closure. While mild eyelid twitching is a common and often benign occurrence, blepharospasm is a more persistent and debilitating condition that can significantly impact daily life. Accurate Blepharospasm Diagnosis is crucial for effective management and to differentiate it from other conditions with similar symptoms.
Understanding Blepharospasm: Types and Classifications
Blepharospasm, at its core, involves abnormal muscle contractions around the eyes. It exists on a spectrum, ranging from minor annoyances to severe functional impairment. It’s important to understand the different classifications to better grasp the condition:
- Eyelid Twitching (Tics): Most people experience fleeting episodes of eyelid twitching, often linked to stress, fatigue, or caffeine intake. These are typically mild, short-lived, and not considered blepharospasm in a clinical sense.
- Benign Essential Blepharospasm (BEB): This is the more severe form that doctors typically refer to as blepharospasm. BEB is characterized by chronic, involuntary spasms that cause forceful eyelid closure. The term “benign” indicates it’s not life-threatening, and “essential” means the cause is unknown (idiopathic).
- Meige’s Syndrome: A more complex dystonia that combines blepharospasm with involuntary movements in the lower face, such as jaw clenching, lip pursing, and tongue thrusting. It’s also known as oromandibular dystonia.
Symptoms of Blepharospasm: Recognizing the Progression
The symptoms of blepharospasm are progressive, often starting subtly and gradually increasing in frequency and intensity. Recognizing this progression is vital for timely blepharospasm diagnosis. Common symptoms include:
- Initial Stages: Increased blinking, sensitivity to light (photophobia), and eye irritation or dryness. These early symptoms can be easily dismissed as minor eye strain or allergies.
- Developing Spasms: Involuntary blinking evolves into more forceful spasms, including squinting, winking, and twitching that are difficult to control. These spasms may be triggered by factors like fatigue, bright lights, stress, or wind.
- Severe Blepharospasm: Spasms become more frequent and prolonged, occurring throughout the day regardless of triggers. In severe cases, the eyelids can be forced shut for extended periods, sometimes hours, leading to functional blindness and significant disruption to daily activities. Eyebrows may also be pulled downwards due to muscle involvement.
Causes and Risk Factors Associated with Blepharospasm
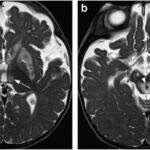
While the exact cause of benign essential blepharospasm remains unknown, research suggests it involves dysfunction in the basal ganglia, an area of the brain responsible for motor control. The prevailing theory points to a disruption in neurotransmitter signaling within these brain regions. While the precise trigger for this dysfunction is unclear, several factors are considered:
- Neurological Dysfunction: The primary suspect is an abnormality in brain function, specifically within the basal ganglia. This disruption may involve imbalances in neurotransmitters, the chemical messengers that facilitate communication between nerve cells.
- Dry Eye Syndrome: Many individuals with blepharospasm also experience or have a history of dry eyes. While the link isn’t fully understood, dry eye may exacerbate or contribute to eyelid spasms in some individuals.
- Medications: Certain medications, particularly antipsychotics and some drugs used for Parkinson’s disease, can induce blepharospasm-like symptoms or trigger the condition in susceptible individuals. Drug-induced blepharospasm is important to rule out during blepharospasm diagnosis.
- Genetic Predisposition: In rare instances, blepharospasm can occur in multiple family members, suggesting a possible genetic component, although this is not a common occurrence.
- Associated Conditions: Blepharospasm can sometimes be associated with other neurological conditions like Parkinson’s disease, Tourette’s syndrome, and Meige’s syndrome, although it often occurs independently.
Blepharospasm Diagnosis: How is it Identified?
There is no specific diagnostic test for blepharospasm. Blepharospasm diagnosis relies primarily on a thorough clinical evaluation, including:
- Physical Examination: A neurologist or ophthalmologist will observe the patient’s eye movements and eyelid spasms. The characteristic involuntary blinking, squinting, and eyelid closure are key indicators.
- Medical History Review: A detailed medical history is crucial. This includes assessing symptoms, their onset and progression, triggers, medications, and any related medical conditions. The doctor will also want to rule out any secondary causes of eyelid spasms.
- Neurological Assessment: A neurological examination may be conducted to assess overall neurological function and rule out other neurological disorders that could mimic or contribute to blepharospasm.
- Differential Diagnosis: Crucially, blepharospasm diagnosis involves ruling out other conditions that can cause similar symptoms. These include:
- Ptosis (Eyelid Drooping): Weakness of the eyelid muscles causing drooping, which can be mistaken for blepharospasm-related eye closure.
- Hemifacial Spasm: Involuntary muscle contractions on one side of the face, including the eyelid, which is distinct from the bilateral nature of blepharospasm.
- Dry Eye Disease: Severe dry eye can cause eye irritation and increased blinking, but lacks the forceful, sustained spasms of blepharospasm.
- Medication-Induced Dystonia: As mentioned, certain drugs can cause dystonic reactions, including eyelid spasms. A careful review of medications is essential.
Treatment Options for Blepharospasm
While there is currently no cure for blepharospasm, several treatments can effectively manage symptoms and improve quality of life. Treatment strategies are typically focused on reducing the severity and frequency of eyelid spasms:
- Botulinum Toxin Injections (Botox/Dysport): This is the gold standard treatment for blepharospasm. Botulinum toxin injections work by temporarily paralyzing the overactive eyelid muscles, reducing spasms. Injections are typically administered every three to four months, and provide significant relief for most patients.
- Medications: Oral medications, such as muscle relaxants (e.g., diazepam) or anticholinergics (e.g., trihexyphenidyl), are sometimes used, but their effectiveness varies and they often have side effects. They are generally less effective than botulinum toxin.
- Stress Management and Support: Stress can exacerbate blepharospasm symptoms. Stress reduction techniques, relaxation therapies, and support groups can be beneficial as adjunctive therapies.
- Surgery (Myectomy): In rare cases where botulinum toxin injections are ineffective, surgery called myectomy may be considered. This procedure involves surgically removing some of the muscles responsible for eyelid spasms.
Seeking Help for Blepharospasm
If you suspect you may have blepharospasm, seeking prompt medical attention is essential for accurate blepharospasm diagnosis and appropriate management. Consult with your primary care physician, who can refer you to a neurologist or ophthalmologist specializing in movement disorders or eye conditions. Early diagnosis and treatment can significantly improve your quality of life and help you manage this challenging condition.