Borderline Personality Disorder (BPD) is a complex mental health condition characterized by instability in various aspects of life, including interpersonal relationships, self-image, emotions, and behavior. In English-speaking countries like Australia and the United States, the diagnosis of BPD typically relies on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). This article will delve into the DSM-5 diagnostic criteria for BPD, providing a clear and comprehensive overview for better understanding.
DSM-5 Diagnostic Criteria for Borderline Personality Disorder
The DSM-5 establishes specific criteria that must be met for a BPD diagnosis. It’s important to note that a diagnosis should always be made by a qualified mental health professional after a thorough evaluation. According to the DSM-5, Borderline Personality Disorder is defined as:
“A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by five (or more) of the following:”
Let’s break down each of these nine criteria:
-
Frantic efforts to avoid real or imagined abandonment: Individuals with BPD often experience intense fear and anxiety surrounding abandonment, whether real or perceived. This fear can lead to desperate actions to prevent separation or rejection, which can paradoxically push people away. Note: Suicidal or self-harming behaviors related to abandonment are covered under criterion 5.
-
A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation: Relationships are often tumultuous and unpredictable. Individuals may quickly idealize someone, developing intense attachment and expectations, only to abruptly shift to devaluation, viewing the person as worthless or bad. This “splitting” of perception creates significant instability in relationships.
-
Identity disturbance: markedly and persistently unstable self-image or sense of self: A core feature of BPD is a lack of a stable and consistent sense of self. Individuals may experience frequent shifts in self-perception, values, goals, and even sexual orientation. They may feel confused about who they are, leading to feelings of emptiness and a lack of direction in life.
-
Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating): Impulsive behaviors that can lead to harm are common. These are often engaged in as a way to cope with distress or emptiness. Note: Suicidal or self-harming behaviors are covered under criterion 5 and should not be counted here.
-
Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior: Suicidal thoughts and behaviors, as well as self-harm, are significant concerns in BPD. These actions may be attempts to cope with overwhelming emotions, seek attention, or express anger and despair.
-
Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days): Moods can shift rapidly and intensely in response to triggers. Episodes of intense sadness, irritability, or anxiety can occur, often resolving within a few hours, though sometimes lasting a bit longer. This emotional reactivity is a key characteristic of BPD.
-
Chronic feelings of emptiness: A persistent sense of emptiness, void, or nothingness is frequently reported. This feeling can be deeply distressing and contribute to other BPD symptoms, such as impulsivity and unstable relationships, as individuals seek to fill this void.
-
Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights): Anger in BPD can be intense, disproportionate to the situation, and difficult to control. This can manifest as frequent outbursts, irritability, or even physical aggression, causing problems in relationships and daily life.
-
Transient, stress-related paranoid ideation or severe dissociative symptoms: Under stress, individuals with BPD may experience brief periods of paranoid thinking or dissociation. Paranoid ideation involves suspiciousness or mistrust of others, while dissociation can involve feeling detached from oneself or reality. These symptoms are typically temporary and triggered by stress.
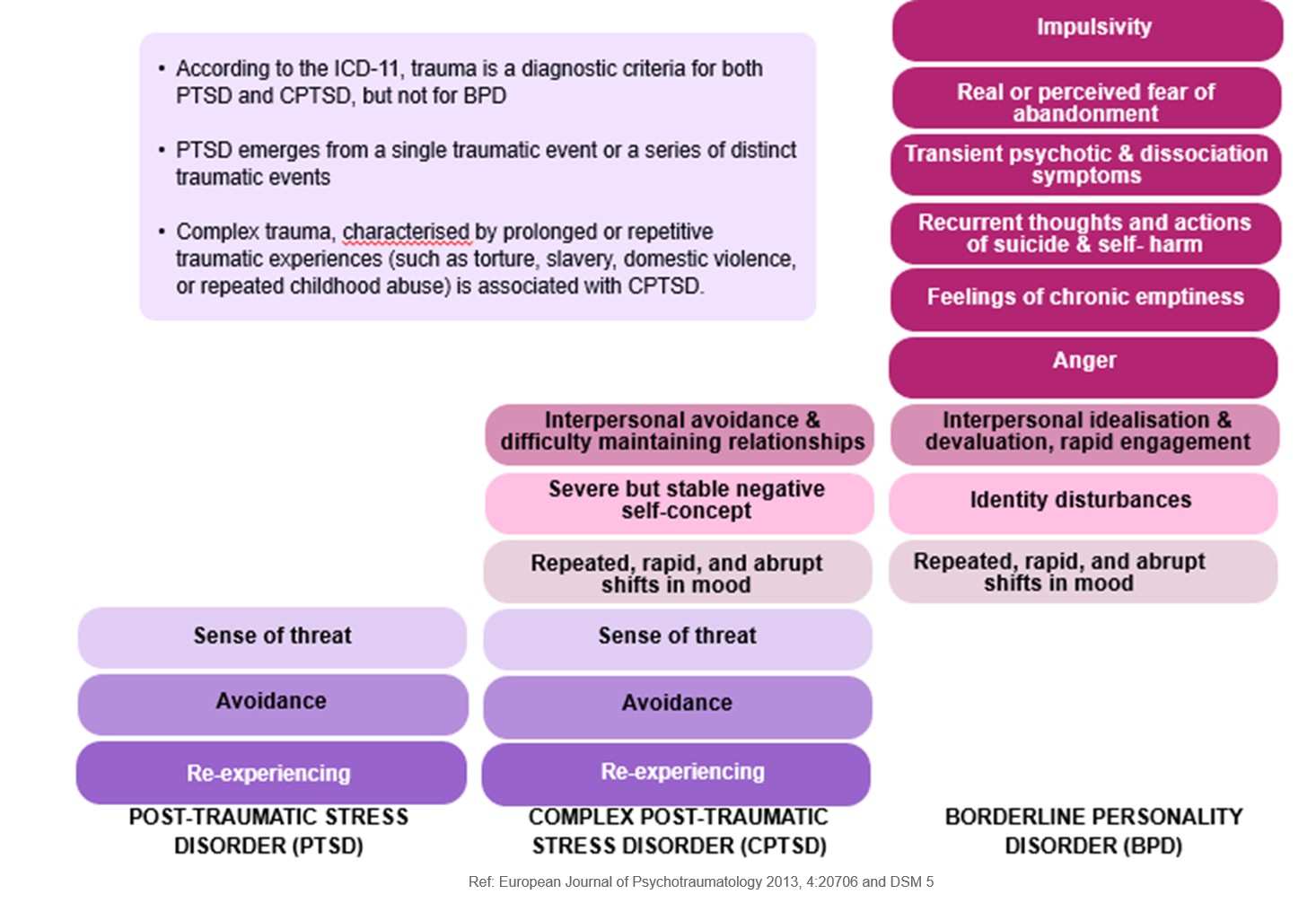 Diagnostic overlap and distinctions between PTSD, CPTSD and BPD
Diagnostic overlap and distinctions between PTSD, CPTSD and BPD
Proposed Alternative DSM-5 Criteria
It’s worth noting that the DSM-5 also includes proposed alternative criteria in the appendix. These proposed criteria emphasize core features such as:
- Instability of self-image
- Instability of personal goals
- Instability of interpersonal relationships
- Instability of affect
- Impulsivity
- Risk-taking
- Hostility
- Difficulties in identity
- Difficulties in self-direction
- Difficulties in empathy
- Difficulties in intimacy
- Maladaptive traits in negative affectivity, antagonism, and disinhibition
While these were proposed, the official DSM-5 criteria remained unchanged from the DSM-IV-TR for the main diagnostic guidelines. This highlights the ongoing discussion and evolution in understanding and diagnosing BPD.
Conclusion
The DSM-5 diagnostic criteria provide a framework for understanding and diagnosing Borderline Personality Disorder. Meeting five or more of the nine criteria points to a potential diagnosis, which should always be confirmed by a mental health professional. Understanding these criteria is a crucial step for individuals seeking diagnosis, loved ones supporting someone with BPD, and professionals working in the field of mental health. It is important to remember that BPD is a treatable condition, and accurate diagnosis is the first step towards effective treatment and improved quality of life.