A brain hemorrhage, also known as intracranial hemorrhage, refers to bleeding within the skull. Diagnosing the source and location of this bleeding is critical for effective treatment and management. If a brain hemorrhage is suspected, healthcare professionals employ a range of diagnostic tests to quickly and accurately identify the issue. This article will explore the primary methods used in Brain Hemorrhage Diagnosis, providing an overview of each technique and its role in detecting this serious condition.
Diagnostic Methods for Brain Hemorrhage
When a person presents with symptoms suggestive of a brain hemorrhage, such as a sudden, severe headache, seizures, or neurological deficits, prompt diagnosis is essential. Several imaging techniques and procedures are available to identify and characterize brain bleeding.
CT Scan
Computed Tomography (CT) scans are frequently the first-line imaging test used in the diagnosis of a brain hemorrhage. CT scans utilize X-rays to create detailed cross-sectional images of the brain. They are particularly effective at rapidly detecting the presence of blood within the brain tissue or the space surrounding the brain.
A CT scan is advantageous due to its speed and availability, especially in emergency settings. It can quickly reveal whether bleeding has occurred and its approximate location. In some cases, a contrast dye may be injected intravenously to enhance the visualization of blood vessels. This is known as a CT angiogram and can help identify abnormalities in blood vessels, such as aneurysms, which may be the cause of the hemorrhage.
However, it’s important to note that CT scans may have limitations. In individuals with a low red blood cell count (anemia) or in cases of very minor bleeding, a CT scan might not detect the hemorrhage.
MRI
Magnetic Resonance Imaging (MRI) is another powerful imaging technique that can be used to diagnose brain hemorrhages. MRI utilizes strong magnetic fields and radio waves to create detailed images of the brain. While often not the first-line test in emergency situations due to longer scan times, MRI can be highly sensitive in detecting brain bleeding, sometimes even when CT scans are inconclusive.
MRI can be particularly useful in identifying older hemorrhages or subtle signs of bleeding that might be missed on a CT scan. Like CT scans, MRI can also be performed with contrast dye (MR angiogram) to visualize blood vessels in greater detail, aiding in the detection of underlying vascular abnormalities.
Cerebral Angiography
Cerebral angiography is a more invasive diagnostic procedure used to get a highly detailed view of the brain’s blood vessels. This test is typically considered when other imaging, like CT or MRI, suggests a subarachnoid hemorrhage, but the cause of the bleeding is not clear or needs further investigation.
During cerebral angiography, a thin, flexible tube called a catheter is inserted into an artery, usually in the groin or arm, and carefully guided to the blood vessels in the brain. Once the catheter is in place, a contrast dye is injected, making the blood vessels visible under X-ray imaging. This allows healthcare professionals to visualize the arteries and veins of the brain in real-time and identify any abnormalities, such as aneurysms or arteriovenous malformations (AVMs), that could be the source of bleeding.
It’s worth noting that in some instances, even cerebral angiography may not immediately reveal an aneurysm, particularly if it is very small or has clotted off. If a subarachnoid hemorrhage is strongly suspected despite a negative angiogram, a repeat angiogram may be performed later to ensure no underlying aneurysm was missed.
Lumbar Puncture
In certain situations, particularly when a subarachnoid hemorrhage is suspected but initial CT or MRI scans do not show bleeding, a lumbar puncture (spinal tap) may be necessary. This procedure involves inserting a needle into the lower back to collect a sample of cerebrospinal fluid (CSF), the fluid that surrounds the brain and spinal cord.
The CSF sample is then analyzed in the laboratory to check for the presence of blood. Blood in the CSF can be a strong indicator of a subarachnoid hemorrhage, even if it was not visible on initial imaging. Lumbar puncture is particularly useful in cases where the hemorrhage occurred several days prior to the diagnostic evaluation, as blood in the CSF can persist for a longer duration than it might be visible on CT scans.
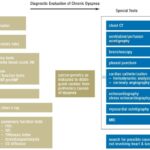
Understanding the Diagnostic Process
The selection of diagnostic tests for a suspected brain hemorrhage depends on various factors, including the patient’s symptoms, clinical presentation, and the initial findings from neurological examinations and preliminary imaging. In emergency situations, the speed and availability of CT scans often make them the primary initial diagnostic tool. MRI and cerebral angiography are typically used for more detailed evaluation or when CT findings are inconclusive. Lumbar puncture serves as a supplementary diagnostic procedure in specific scenarios.
It is important to remember that brain hemorrhage diagnosis is a complex process that requires the expertise of neurologists, neurosurgeons, and neuroradiologists. These specialists work together to interpret the results of diagnostic tests and determine the most appropriate course of treatment to stabilize the patient’s condition, address the underlying cause of the bleeding, and prevent potential complications.
Early and accurate diagnosis is paramount in improving outcomes for individuals experiencing a brain hemorrhage. Prompt medical attention and appropriate diagnostic evaluation are crucial steps in ensuring the best possible care and management of this critical medical condition.