Asthma, a prevalent chronic syndrome affecting millions globally, is characterized not as a singular disease, but as a constellation of signs and symptoms. While classic asthma symptoms such as chest tightness, wheezing, coughing, and dyspnea are well-recognized, the reality is that asthma encompasses a spectrum of pulmonary diseases marked by reversible airway obstruction. This obstruction can stem from allergic (immunoglobulin E (IgE)-mediated) or non-allergic etiologies. Given this complexity and the breadth of conditions that can mimic its presentation, establishing an accurate bronchial asthma differential diagnosis is paramount. This article provides an in-depth exploration of the differential diagnoses for bronchial asthma, essential for clinicians to ensure precise diagnosis and effective patient management.
Understanding Asthma: A Brief Overview
Historical Context
The term “asthma” originates from the Greek word “aazein,” meaning “to pant.” Even in ancient times, Hippocrates recognized asthma as a distinct medical entity characterized by lung spasms. Ancient Chinese medicine utilized ephedrine-containing plants, mirroring modern bronchodilator therapies. In the 19th century, Dr. Henry Salter elucidated key asthma characteristics, including airway hyperresponsiveness to triggers like cold air, exercise, and environmental irritants.
Asthma in Modern Medicine
Today, asthma is recognized as a chronic inflammatory disorder of the airways. It’s crucial to understand that “asthma” is a clinical syndrome, not a definitive diagnosis in itself. Diagnosis relies on recognizing patterns of signs and symptoms, as no single definitive diagnostic criterion exists. The hallmark of asthma is reversible airway obstruction, a feature shared across various pulmonary conditions. Asthma is broadly categorized into allergic and non-allergic types, with non-allergic asthma encompassing diverse phenotypes.
Table 1: Common Asthma Symptoms
| Symptom | Description |
|---|---|
| Wheeze | High-pitched whistling sound during breathing |
| Cough | May be dry or productive, often worse at night or early morning |
| Dyspnea | Shortness of breath, difficulty breathing |
| Chest Tightness | Sensation of pressure or constriction in the chest |
Pathology and Histopathology of Asthma
The underlying pathophysiology of asthma involves reversible airway obstruction, airway hyperreactivity, and chronic inflammation. Inflammatory mediators drive recurrent airflow limitation, leading to bronchoconstriction, airway edema, hyperresponsiveness, and airway remodeling. Bronchoconstriction is a rapid response to irritants or allergens, involving bronchial smooth muscle contraction. While reversibility of obstruction is a classic asthma indicator, some patients exhibit only partial or no reversal due to airway remodeling. This remodeling involves persistent inflammation, smooth muscle hypertrophy, collagen production, and other structural changes in the airway.
In allergic asthma, inhaled antigens trigger mast cell and Th2 cell activation, releasing histamine, leukotrienes, and cytokines (IL-4, IL-13, IL-5). IL-5 is crucial for eosinophil differentiation, which further perpetuates airway inflammation through the release of leukotrienes and other inflammatory substances. Histopathology consistently reveals eosinophilic infiltration and mucus plugging in asthma patients.
Regardless of asthma severity (mild, moderate, severe), consistent histopathological changes are observed, including epithelial detachment, goblet cell hyperplasia, subepithelial fibrosis, inflammatory cell infiltration, smooth muscle hypertrophy, and vascular alterations. Despite these consistent changes, asthma’s clinical course varies significantly among individuals.
Common Asthma Triggers
Environmental factors play a significant role in triggering asthma. Common triggers include:
- Perennial allergens: Dust mites, molds, pets, rodents, cockroaches
- Outdoor allergens: Pollen (tree, grass, weed)
- Infections: Viral respiratory infections
- Occupational exposures: Irritants and sensitizers in the workplace
- Air pollution: Particulate matter, ozone
- Exercise: Especially in cold, dry air
While allergen avoidance is recommended, it’s often insufficient to fully control asthma. Treatment strategies are tailored to symptom frequency and severity, ranging from quick-relief medications (short-acting beta2-agonists, anticholinergics) to long-term control medications (inhaled corticosteroids, long-acting beta2-agonists, leukotriene modifiers). Biologic agents and allergen immunotherapy are options for specific asthma phenotypes and triggers. Vaccination against respiratory infections is also crucial to minimize infectious triggers.
Table 2: Common Asthma Triggers
| Trigger Category | Examples |
|---|---|
| Perennial Allergens | Dust mites, pet dander, mold |
| Outdoor Allergens | Pollen, ragweed |
| Infections | Viral respiratory infections (e.g., rhinovirus) |
| Occupational Exposures | Chemicals, dusts, fumes |
| Air Pollution | Smog, particulate matter |
| Exercise | Cold air exercise |
Differential Diagnosis: Conditions Mimicking Asthma
When asthma symptoms persist despite treatment, or when atypical features are present, a thorough bronchial asthma differential diagnosis is crucial. Several conditions can mimic asthma, and accurate differentiation is vital for appropriate management.
Chronic Obstructive Pulmonary Disease (COPD)
COPD, like asthma, is an umbrella term for various lung conditions characterized by airflow obstruction. Chronic bronchitis and emphysema are key COPD phenotypes. Asthma-COPD overlap syndrome (ACOS) further complicates diagnosis, as it shares features of both conditions.
COPD is generally considered less reversible than asthma, although reversibility can occur in COPD as well. Symptoms like wheezing, cough, and dyspnea are common to both. Diagnosis relies on patient history and pulmonary function tests (PFTs). COPD is defined by a post-bronchodilator FEV1/FVC ratio of <0.7.
Distinguishing features of COPD include:
- Limited reversibility: Airflow obstruction may not fully reverse with bronchodilators.
- Smoking history: Strong association with cigarette smoking or exposure to biomass smoke. Pack-years history is crucial.
- Reduced DLCO: Decreased diffusing capacity for carbon monoxide, reflecting emphysema.
- Emphysema on CT scan: Alveolar destruction and dilation. In contrast, asthma typically involves air trapping without alveolar destruction and normal DLCO.
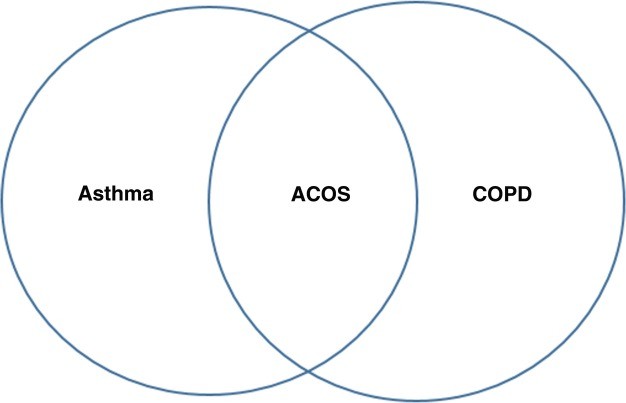 Fig. 1: Asthma-COPD overlap syndrome
Fig. 1: Asthma-COPD overlap syndrome
Pneumonia
Pneumonia, an infection of the lung parenchyma, should be considered in the bronchial asthma differential diagnosis, especially in patients with acute respiratory symptoms, fever, tachypnea, and pulmonary infiltrates on chest radiographs. Pneumonia can be caused by bacteria, viruses, or fungi.
Viral infections are major triggers for asthma exacerbations and common causes of pneumonia. Influenza virus is a significant concern, particularly during outbreaks. Secondary bacterial infections should also be considered in viral pneumonia. Common viral causes include respiratory syncytial virus (RSV), parainfluenza virus, and others. In children, viruses are the most frequent pneumonia etiology.
Community-acquired pneumonia (CAP) refers to pneumonia acquired outside of a hospital setting. Common bacterial causes of CAP include Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus. Mycoplasma pneumoniae is an atypical bacterium associated with both early and late-onset asthma, often presenting with milder symptoms.
Uncommon pneumonia causes include fungal infections, such as Histoplasma and Coccidioides in endemic regions, and opportunistic fungi like Candida and Aspergillus in immunocompromised patients.
Table 3: Differential Diagnosis of Asthma
| Common | Less Frequent | Uncommon |
|---|---|---|
| COPD | Idiopathic anaphylaxis with predominant respiratory manifestations | Lymphangioleiomyomatosis (LAM) |
| Infectious etiologies: Bacterial, Viral, Fungal | Aspirin or nonsteroidal exacerbated respiratory disease (AERD/Samter’s triad) | Cystic fibrosis |
| Gastroesophageal reflux disease (GERD) | Malignancy | Loeffler’s syndrome and other eosinophilic lung diseases |
| Chronic rhinosinusitis (CRS) | Sarcoidosis and other autoimmune processes | Vasculitides: Churg-Strauss vasculitis (EGPA), Wegener’s granulomatosis (GPA), Microscopic polyangiitis |
| Congestive heart failure (CHF) | Hypersensitivity pneumonitis | |
| Vocal cord dysfunction (VCD) and upper airway disorders | Pulmonary hypertension | |
| Drug-induced bronchospasm |
Table 4: Common Pneumonic Etiologies with Asthma-like Symptoms
| Bacterial | Viral | Fungal |
|---|---|---|
| Streptococcus pneumoniae | Respiratory syncytial virus (RSV) | Histoplasma, Coccidioidomycosis (endemic areas) |
| Haemophilus influenzae | Parainfluenza and influenza virus | Candida, Aspergillus, Zygomycetes (ICU setting) |
| Staphylococcus aureus | Human metapneumovirus | |
| Mycoplasma pneumoniae |
Gastroesophageal Reflux Disease (GERD)
GERD, characterized by stomach acid reflux into the esophagus, can present with extraesophageal symptoms mimicking asthma, such as chronic cough, wheezing, and bronchospasm. Heartburn, the classic GERD symptom, is not always present. Certain foods and drinks can trigger GERD symptoms. GERD can coexist with asthma in a significant number of patients and may act as an asthma trigger.
Diagnosis of GERD is primarily clinical. pH probe or barium swallow may aid in differentiation from asthma. Treatment with proton pump inhibitors (PPIs) may improve asthma-like symptoms in patients with GERD-related respiratory issues. However, persistent asthma symptoms despite GERD treatment warrant further investigation for other diagnoses.
Chronic Sinusitis
Chronic sinusitis (CRS), inflammation of the sinuses lasting 12 weeks or longer, can also mimic asthma. Symptoms like shortness of breath due to nasal congestion and cough from postnasal drip overlap with asthma. Both conditions share inflammatory mediators and can be triggered by infections, air pollution, and allergens.
Diagnosis of CRS involves symptom assessment and evidence of sinus inflammation via endoscopy or CT scan. Allergic rhinosinusitis and bacterial sinusitis are common etiologies. Treatment depends on the underlying cause, ranging from intranasal corticosteroids for allergic rhinitis to antibiotics for bacterial sinusitis.
Congestive Heart Failure (CHF)
CHF, resulting from ventricular dysfunction, is a leading cause of acute dyspnea, particularly in the elderly. Cardiac wheezing, occurring in a significant proportion of CHF patients, can be mistaken for asthma. Wheezing in CHF arises from increased pulmonary vascular pressure and interstitial edema, leading to bronchial narrowing.
Diagnosis of CHF involves history, physical exam, echocardiogram, electrocardiogram, and chest X-ray. Treatment focuses on reducing preload and afterload with medications like diuretics, ACE inhibitors, and beta-blockers.
Vocal Cord Dysfunction (VCD)
VCD involves paradoxical vocal cord adduction during inspiration, causing asthma-like symptoms such as wheezing, dyspnea, and cough. VCD can be triggered by similar factors as asthma, including irritants, exercise, and emotional stress. Inspiratory wheezing, dysphonia, and throat tightness are suggestive of VCD.
Diagnosis of VCD involves clinical history, physical exam, questionnaires (VCDQ, Pittsburgh VCD index), spirometry (inspiratory flow loop abnormalities), and laryngoscopy (gold standard). Treatment includes reassurance, speech therapy, and breathing techniques.
Anaphylaxis
Anaphylaxis, a severe, systemic allergic reaction, can present with respiratory symptoms resembling asthma, such as wheezing and dyspnea. Anaphylaxis is typically triggered by medications or foods and involves multiple organ systems. Exercise-induced anaphylaxis (EIA) can mimic exercise-induced asthma. Idiopathic anaphylaxis, with no identifiable trigger, is also in the bronchial asthma differential diagnosis.
Diagnosis of anaphylaxis is clinical, based on rapid onset and multisystem involvement. Epinephrine is the primary treatment. Management of idiopathic anaphylaxis involves prophylactic medications and epinephrine auto-injectors.
Samter’s Triad (Aspirin-Exacerbated Respiratory Disease – AERD)
AERD, or Samter’s triad, consists of asthma, nasal polyps, and aspirin/NSAID sensitivity. NSAID ingestion triggers upper and lower airway symptoms, including wheezing and chest tightness, mimicking asthma exacerbations. AERD is considered an asthma phenotype.
Diagnosis of AERD is confirmed by oral aspirin challenge. Treatment includes aspirin desensitization and management of asthma and sinusitis.
Malignancy
Malignancies, particularly lung cancer and carcinoid tumors, can present with respiratory symptoms like cough, dyspnea, and wheezing, mimicking asthma. Persistent respiratory symptoms despite asthma treatment warrant consideration of malignancy in the bronchial asthma differential diagnosis.
Lung cancer is a leading cause of cancer death. Symptoms can be subtle initially. Carcinoid tumors are rare, slow-growing lung tumors that can also mimic asthma. Diffuse idiopathic pulmonary neuroendocrine hyperplasia (DIPNECH), a premalignant condition, can also cause asthma-like symptoms.
Sarcoidosis
Pulmonary sarcoidosis, a granulomatous disease affecting multiple organs, can present with dyspnea and cough, mimicking asthma. Diagnosis is based on clinical, radiographic, and histopathologic findings, excluding other causes.
Sarcoidosis pathogenesis is not fully understood. Treatment may not be necessary in mild cases. Severe pulmonary sarcoidosis is treated with glucocorticoids and other immunosuppressants.
Hypersensitivity Pneumonitis (HP)
HP, or extrinsic allergic alveolitis, results from an inflammatory response to inhaled environmental antigens. HP can present acutely, subacutely, or chronically, with symptoms overlapping with asthma, including cough, dyspnea, and chest tightness.
Diagnosis of HP involves detailed history (environmental and occupational exposures), clinical presentation, imaging, and laboratory findings. Antigen avoidance is crucial.
Pulmonary Arterial Hypertension (PAH)
PAH, characterized by elevated pulmonary arterial pressures, can cause symptoms like breathlessness, dyspnea, and chest discomfort, which can be mistaken for asthma. Echocardiogram is used for screening, and right heart catheterization is the gold standard for diagnosis.
Lymphangioleiomyomatosis (LAM)
LAM, a rare cystic lung disease affecting women of reproductive age, can present with dyspnea, cough, and chest pain, mimicking asthma. Chest CT showing characteristic cysts aids in diagnosis. Serum VEGF-D testing and lung biopsy may be needed.
Cystic Fibrosis (CF)
CF, an autosomal recessive disorder, can mimic asthma due to cough and dyspnea. Newborn screening programs often lead to early diagnosis. CF involves mutations in the CFTR gene, leading to mucus retention and chronic lung infections. Sweat test confirms diagnosis.
Eosinophilic Pulmonary Diseases
Eosinophilic pulmonary diseases encompass various conditions characterized by lung eosinophilia, which can present with asthma-like symptoms. Löffler syndrome, chronic eosinophilic pneumonia (CEP), and eosinophilic granulomatosis with polyangiitis (Churg-Strauss Syndrome) are examples.
CEP is characterized by peripheral pulmonary infiltrates and eosinophilia. Churg-Strauss syndrome (EGPA) is a rare vasculitis associated with asthma and eosinophilia, often presenting with refractory asthma and multisystem involvement.
Other Pulmonary Vasculitis Syndromes
Wegener’s granulomatosis (granulomatosis with polyangiitis – GPA) and microscopic polyangiitis are systemic vasculitides that can involve the lungs and mimic asthma. GPA typically involves upper and lower airways and kidneys. Microscopic polyangiitis often presents with alveolar hemorrhage. ANCA testing and biopsy are crucial for diagnosis.
Summary: The Importance of Differential Diagnosis in Bronchial Asthma
While asthma is a common condition, numerous other diseases can mimic its symptoms. A comprehensive bronchial asthma differential diagnosis is essential for accurate diagnosis and appropriate patient care. Careful history taking, physical examination, and judicious use of diagnostic tests (imaging, spirometry, laboratory studies) are crucial to differentiate asthma from its mimics. Clinical vigilance is paramount, particularly when asthma symptoms are atypical or unresponsive to standard asthma therapies. Considering the broad spectrum of conditions in the differential diagnosis ensures that patients receive the correct diagnosis and targeted treatment, ultimately improving outcomes and quality of life.
Contributor Information
John Johnson, Email: [email protected].
Tina Abraham, Email: [email protected].
Monica Sandhu, Email: [email protected].
Robert Hostoffer, Email: [email protected].
Theodore Sher, Email: [email protected].
Dennis K. Ledford, Email: [email protected]
Timothy Craig, Email: [email protected], Email: [email protected].
Collaborators: Massoud Mahmoudi, Dennis K. Ledford, Timothy Craig, Dennis K. Ledford, and Timothy Craig