Brugada Syndrome is a critical cardiac condition characterized by an increased risk of sudden cardiac death in individuals with structurally normal hearts. Diagnosis hinges significantly on recognizing specific electrocardiogram (ECG) patterns in conjunction with clinical risk factors. Understanding Brugada Syndrome Ecg Diagnosis is therefore paramount for effective patient management and risk stratification.
First identified in 1992 by the Brugada brothers, this syndrome has garnered increasing recognition worldwide. The average age of sudden death associated with Brugada Syndrome is around 41 years, but diagnoses can occur across a wide age spectrum, from infancy to advanced age. Notably, the incidence is particularly high in Southeast Asia, where it was historically known by various local terms reflecting sudden unexplained nocturnal deaths. These historical descriptions underscore the long-standing, albeit previously less understood, presence of this condition.
Key Aspects of Brugada Syndrome Diagnosis
- Brugada syndrome is fundamentally a single entity, not multiple distinct types, though ECG presentations vary.
- Diagnosis requires both a characteristic ECG finding and specific clinical criteria to be met. The ECG finding alone, often called the “Brugada sign,” is not sufficient for diagnosis.
- Risk stratification following diagnosis remains a complex and debated area in cardiology.
- The established and definitive treatment for Brugada Syndrome is the implantable cardioverter-defibrillator (ICD).
- The isolated presence of a Brugada ECG pattern, without accompanying clinical risk factors, has uncertain clinical significance and should not be considered a definitive diagnosis of Brugada Syndrome.
Unraveling the Etiology: Sodium Channelopathy
At its core, Brugada Syndrome is a genetic disorder resulting from mutations in genes that control cardiac sodium channels. This makes it a type of sodium channelopathy. Over 60 different gene mutations have been linked to Brugada Syndrome. While many cases arise from spontaneous mutations, familial clustering and autosomal dominant inheritance patterns are also observed, indicating a genetic predisposition in many instances.
It’s crucial to recognize that ECG changes in Brugada Syndrome can be dynamic and influenced by various factors. These ECG patterns can be transient, appearing and disappearing, or they can be unmasked or accentuated by:
- Fever: Elevated body temperature can exacerbate the ECG abnormalities.
- Myocardial Ischemia: Reduced blood flow to the heart muscle.
- Pharmacological Agents: Numerous medications can trigger or worsen Brugada ECG patterns, including:
- Sodium channel blockers (e.g., Flecainide, Propafenone) – paradoxically, drugs that block sodium channels can reveal the syndrome.
- Calcium channel blockers
- Alpha-adrenergic agonists
- Beta-adrenergic blockers
- Nitrates
- Cholinergic agents
- Cocaine
- Alcohol
- Electrolyte Imbalances: Both hypokalemia (low potassium) and hyperkalemia (high potassium).
- Hypothermia: Low body temperature.
- Post DC Cardioversion: Following electrical cardioversion.
Diagnostic Criteria: ECG Patterns and Clinical Context
The diagnosis of Brugada Syndrome is not solely based on ECG findings but requires the presence of a specific ECG pattern in conjunction with relevant clinical criteria.
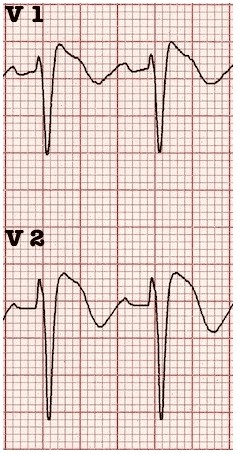
Type 1 Brugada ECG Pattern (Diagnostic)
- Characterized by a coved-type ST-segment elevation of greater than 2mm in at least one of the precordial leads V1-V3, followed by a negative T wave.
- This Type 1 pattern is the only ECG abnormality considered potentially diagnostic for Brugada Syndrome. It is commonly referred to as the Brugada sign.
Crucially, the Type 1 ECG pattern must be associated with at least one of the following clinical criteria to confirm the diagnosis of Brugada Syndrome:
- Documented Ventricular Fibrillation (VF) or Polymorphic Ventricular Tachycardia (VT): A history of these dangerous arrhythmias.
- Family History of Sudden Cardiac Death: Particularly in individuals under 45 years of age.
- Coved-type ECGs in Family Members: Presence of Type 1 Brugada ECG patterns in family members.
- Inducibility of VT with Programmed Electrical Stimulation (EPS): Provocation of ventricular tachycardia during an electrophysiology study.
- Syncope: Unexplained fainting or near-fainting episodes.
- Nocturnal Agonal Respiration: Gasping or labored breathing during sleep, suggestive of nocturnal arrhythmia.
Type 2 and Type 3 Brugada ECG Patterns (Non-Diagnostic)
- Type 2 Brugada ECG Pattern: Exhibits greater than 2mm of saddleback-shaped ST-segment elevation. This pattern, while suggestive, is not considered diagnostic on its own.
- Type 3 Brugada ECG Pattern: Can display either a coved or saddleback morphology, but with ST-segment elevation of less than 2mm. This pattern is also non-diagnostic in isolation.
It’s important to note that while Type 2 and Type 3 patterns are not diagnostic for Brugada Syndrome, their presence, particularly in individuals with suggestive symptoms or family history, may warrant further investigation and risk assessment.
Management Strategies
The primary and most effective therapy for Brugada Syndrome is the implantable cardioverter-defibrillator (ICD). The ICD is designed to detect and correct life-threatening ventricular arrhythmias, preventing sudden cardiac death. In situations where ICDs are not immediately available or are contraindicated (e.g., in neonates), quinidine has been proposed as a pharmacological alternative to reduce arrhythmic risk.
Untreated Brugada Syndrome carries a significant risk of sudden death, with estimates suggesting a mortality rate of approximately 10% per year in undiagnosed individuals. The identification of a Type 1 Brugada ECG pattern, especially in the context of concerning clinical features, often necessitates hospital admission for further evaluation and management.
For patients with asymptomatic Type 1 ECG patterns, or those exhibiting Type 2 or Type 3 patterns, risk stratification is crucial. An electrophysiology study (EPS) may be considered to assess the inducibility of ventricular tachycardia or fibrillation. EPS can help determine the patient’s arrhythmic risk and guide decisions regarding ICD implantation.
However, the role of EPS in risk stratification remains a subject of debate and ongoing research. Some experts advocate for a low threshold for EPS and ICD implantation, while others favor a more conservative approach. One of the limitations of EPS is its imperfect predictive value, with a negative predictive value of less than 50%. Some studies suggest that the clinical significance of the Brugada ECG pattern, particularly in asymptomatic individuals, may be overemphasized.
For example, a study following asymptomatic Japanese patients with the “Brugada sign” for nearly 8 years found no increased mortality compared to a control group. This underscores the importance of clinical criteria in conjunction with ECG findings for accurate diagnosis and risk assessment.
In cases with Type 2 or Type 3 ECG patterns where clinical suspicion for Brugada Syndrome exists, pharmacological provocation testing with sodium channel blocking drugs has been suggested. These drugs can unmask a Type 1 pattern if the underlying predisposition to Brugada Syndrome is present. However, the sensitivity of this provocative testing is not fully established, and individuals with Type 2 and Type 3 patterns, without other high-risk features, may have a very low or negligible increased mortality risk compared to the general population.