A burn is a type of tissue injury resulting from exposure to excessive heat, electricity, radiation, or corrosive chemicals. These agents cause denaturation, or breakdown, of proteins within skin cells. Burns disrupt the body’s homeostatic balance and are classified by severity to guide appropriate medical intervention. For nurses, accurate burn diagnosis and effective nursing care are crucial in patient recovery and minimizing complications.
Types and Classification of Burns in Nursing Diagnosis
Burns are categorized primarily by depth, which ranges from superficial to full thickness. They are also classified by the total body surface area (TBSA) affected and the burn location, as certain areas pose higher risks. Understanding burn classification is fundamental in Burn Diagnosis Nursing.
Burn Classification Chart for Nursing Professionals
| Classification | Description | Clinical Signs | Pain Level | Blistering | TBSA Consideration | Nursing Implications |
|---|---|---|---|---|---|---|
| Superficial (1st Degree) | Epidermis only | Red, dry, blanches easily | Painful | No | Not counted | Cooling, soothing lotions; focus on pain management and patient education. |
| Superficial Partial Thickness (2nd Degree) | Epidermis and part of dermis | Moist, red, blanches, blisters | Very painful | Yes | Counted | Pain management, prevent infection, wound care, monitor for healing, patient education on wound care. |
| Deep Partial Thickness (2nd Degree) | Epidermis and deeper dermis | Drier, pale, less blanching | Less pain | Yes/No | Counted | Specialized wound care, possible grafting, infection monitoring, pain management. |
| Full Thickness (3rd Degree) | Through all skin layers, potentially to deeper tissues (muscle, bone) | Dry, leathery, variable color (white, brown, black), no blanching | Painless | No | Counted | Surgical intervention often required, fluid resuscitation, prevent infection, pain management. |
Superficial Burns (First-Degree Burns) in Nursing
Superficial burns, or first-degree burns, are limited to the epidermis, the outermost skin layer. These burns are typically characterized by:
- Affecting only the epidermis.
- Dry, red appearance.
- Blanching easily to the touch.
- Absence of blisters.
- Pain and discomfort, classic examples being sunburn.
- Not included when calculating Total Body Surface Area (TBSA) for burn extent.
Superficial Partial Thickness Burns (Second-Degree Burns) in Nursing
Superficial partial thickness burns, a type of second-degree burn, extend beyond the epidermis into the dermis. Key features include:
- Reaching into the dermis layer of the skin.
- Moist, red wound bed.
- Blanching with pressure.
- Presence of blisters.
- Significant pain due to nerve involvement.
- Potential for scarring depending on depth and individual healing factors.
Deep Partial Thickness and Full Thickness Burns (Third-Degree Burns) in Nursing
Deep partial thickness and full thickness burns represent more severe injuries. Traditionally classified as third-degree burns, they involve deeper skin layers and potentially underlying tissues.
-
Deep Partial Thickness Burns:
- Extend into the deeper dermis.
- Appear drier and paler compared to superficial partial thickness burns.
- Reduced blanching.
- Decreased pain sensation due to nerve damage.
-
Full Thickness Burns:
- Destroy all layers of the skin, and may involve subcutaneous tissue, muscle, and bone.
- Present a dry, leathery texture.
- Exhibit variable coloration, including white, brown, or black.
- Complete loss of pinprick sensation due to destruction of nerve endings.
Related Educational Videos for Burn Diagnosis Nursing
Epidermis: Cell Types and Layers
Total Body Surface Area (TBSA) in Burn Diagnosis Nursing
TBSA, or Total Body Surface Area, is an essential assessment in burn diagnosis nursing. It estimates the percentage of the body surface affected by the burn. TBSA calculation is vital for determining burn severity, guiding fluid resuscitation protocols, and planning comprehensive treatment strategies.
The “Rule of Nines” is a widely used method for TBSA estimation in adults. This method divides the body into anatomical regions, each representing 9% or multiples of 9% of the total body surface. For instance:
- Each arm: 9% TBSA
- Each leg: 18% TBSA
- Anterior torso: 18% TBSA
- Posterior torso: 18% TBSA
- Head and neck: 9% TBSA
Pediatric burn patients require different TBSA calculation methods due to proportionally larger head sizes in children. Pediatric burn charts are utilized for more accurate TBSA estimation in this population.
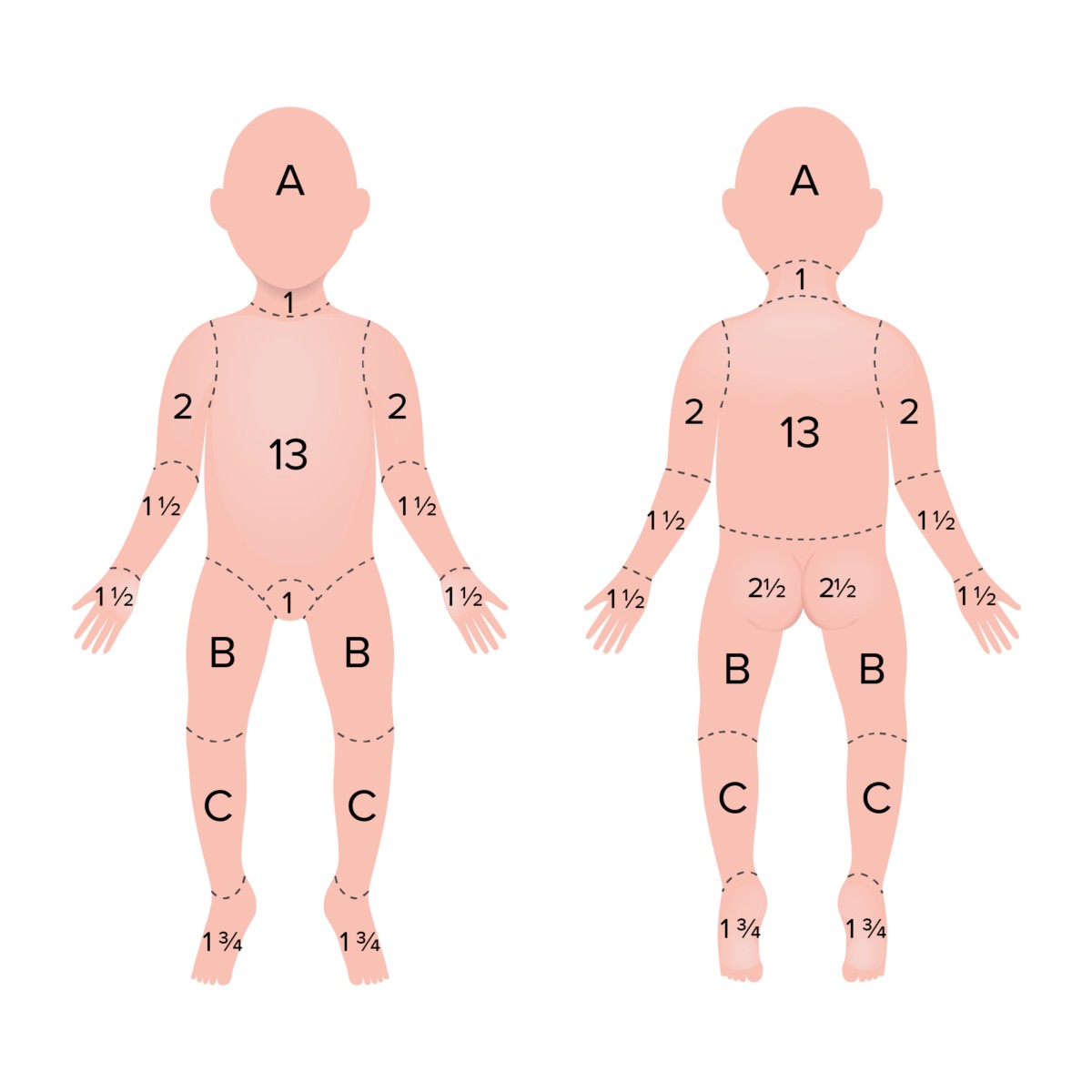 Rule of 9s in children
Rule of 9s in children
Rule of Nines in children: TBSA percentages adjusted for pediatric anatomy.
Area A represents 8.5% TBSA in a 1-year-old, decreasing to 4.5% in a 15-year-old. Area B ranges from 3.25% to 4.5% TBSA across the same age range. Area C varies from 2.5% to 3.25% TBSA in children aged 1 to 15 years.
Image courtesy of Lecturio.
Essential Nursing Interventions and Burn Care Tips
Effective burn diagnosis nursing encompasses a range of critical interventions and care strategies.
Initial Nursing Interventions for Burn Patients
- Hypothermia Monitoring: Burn patients are at risk of hypothermia due to skin damage; continuous temperature monitoring is essential.
- Airway Assessment and Breathing: Assess for respiratory distress, particularly in burns involving the face, mouth, or signs of smoke inhalation (singed nasal hair, soot around the mouth). Intubation may be necessary to secure the airway.
- Cervical Spine Precautions: Maintain C-spine stabilization, especially in trauma cases.
- Neurological Assessment: Conduct thorough neurological evaluations to identify any concurrent injuries or changes in patient status.
- Burn Unit Referral: Facilitate timely transfer to specialized burn centers for extensive burns, burns to sensitive areas (genitalia), high-voltage electrical or chemical burns, and pediatric burns, as these require specialized multidisciplinary care.
- Hyperkalemia Management: Monitor for hyperkalemia, a common complication due to cell lysis releasing intracellular potassium into the circulation.
Nursing Care for Second-Degree Burns
Nursing care for patients with second-degree burns involves a comprehensive approach:
- Burn Wound and Patient Status Assessment: Regularly evaluate the burn wound characteristics and the patient’s overall condition.
- Pain Management: Implement effective pain management strategies, including pharmacological and non-pharmacological methods.
- Wound Care and Infection Prevention: Clean and dress the burn wound using sterile techniques. Monitor for signs of infection regularly and implement preventive measures.
- Patient Education: Educate the patient and family on wound care at home, nutritional support for healing, and infection prevention strategies.
- Emotional and Psychological Support: Provide emotional support to address pain, anxiety, and concerns related to changes in physical appearance and functional abilities.
- Detailed Documentation: Maintain thorough and accurate documentation of all assessments, interventions, and patient responses.
Management of Burn Blisters in Nursing
Burn blister management is a key aspect of burn diagnosis nursing and wound care:
- Blister Assessment: Evaluate blisters for size, location, signs of infection (redness, purulent drainage), and the patient’s pain level.
- Sterile Dressing Application: Apply sterile burn dressings to intact blisters to protect them and promote healing.
- Pain Medication Administration: Administer prescribed pain medications to manage blister-related pain.
- Infection Monitoring: Vigilantly monitor for any signs of infection around the blister and the surrounding skin.
- Patient Education on Blister Care: Instruct patients not to intentionally rupture blisters. De-roofing or drainage should only be performed by healthcare professionals in specific circumstances.
- Documentation of Blister Care: Document all aspects of blister assessment and management in the patient’s record.
Common Nursing Diagnoses Related to Burns
Nursing diagnoses for burn patients are diverse and depend on burn severity, location, and individual patient factors. Common nursing diagnoses in burn care include:
- Impaired Skin Integrity: related to thermal injury, evidenced by disruption of skin layers.
- Acute Pain: related to exposed nerve endings and inflammatory processes at the burn site.
- Fluid Volume Deficit: related to fluid loss through the burn wound and increased capillary permeability.
- Impaired Physical Mobility: related to pain, edema, wound dressings, or potential joint contractures.
- Ineffective Thermoregulation: related to loss of the skin’s thermoregulatory function.
- Altered Nutrition: less than body requirements, related to the hypermetabolic state associated with burn injuries and increased nutritional demands.
- Risk for Infection: related to loss of the skin’s protective barrier and potential for pathogen invasion.
Becoming a Burn Care Nurse: Specialization and Expertise
Burn unit nurses are specialized critical care nurses dedicated to treating patients with burn injuries. These nurses may work in specialized burn units, emergency departments, intensive care units, or outpatient burn clinics. Burn diagnosis nursing and ongoing care require advanced clinical skills, empathy, and the ability to support patients and their families through extended and challenging recovery periods.
To become a burn unit nurse, typically, nurses gain experience in acute care or critical care settings after obtaining their nursing licensure. Certifications such as Certified Wound Care Nurse (CWCN) or Certified Pediatric Emergency Nurse (CPEN) can enhance qualifications for burn unit positions, demonstrating specialized knowledge and commitment to burn patient care.