Introduction
The calcifying odontogenic cyst (COC), a benign developmental odontogenic cyst first identified in 1962, presents a unique diagnostic challenge in oral pathology. Characterized by its distinctive histopathological features, notably the presence of “ghost” epithelial cells with a tendency to calcify, COC can also be associated with other odontogenic tumors, leading to a spectrum of clinical, histopathological, and radiological variations. While reports of actual transformation are scarce, documented cases often highlight the coexistence of COC with other lesions, underscoring the complexities in its diagnosis and classification. This article aims to provide an in-depth exploration of the differential diagnosis of calcifying odontogenic cysts, enhancing the understanding for dental professionals in English-speaking regions. Building upon existing knowledge, we will delve into the nuances of COC diagnosis, emphasizing the critical distinctions from other odontogenic lesions and periapical pathologies.
In daily clinical practice, dental professionals may encounter uncommon lesions with atypical presentations that can easily mimic routine pathological entities. The signs and symptoms associated with such lesions can be misleading, posing significant diagnostic and therapeutic challenges. Accurate diagnosis is paramount as it dictates the treatment approach and ultimately influences patient outcomes. Rare pathologies, in particular, can often masquerade as more frequently encountered conditions like typical periapical lesions, making a thorough differential diagnosis essential.
True bone cysts within the facial bones are relatively common due to the presence of embryonic epithelial rests, many of which are remnants of the odontogenic apparatus. Among these, the calcifying odontogenic cyst constitutes a small but significant fraction, accounting for approximately 0.3–0.8% of all odontogenic cysts [1]. Since its initial description in the early 20th century and subsequent delineation as a distinct entity in the 1960s, the COC has been subject to extensive classification due to its diverse histopathological presentations. Proposed classifications often categorize COC into multiple groups and subgroups, reflecting its spectrum of variants [2]. The existing literature confirms that COC encompasses a range of entities, from developmental odontogenic cysts to benign and potentially malignant odontogenic tumors [2]. Atypical presentations of COC are not uncommon, with reported associations with other odontogenic entities, most notably the adenomatoid odontogenic tumor (AOT) [3].
This article revisits a compelling case where an asymptomatic presentation initially led to a misdiagnosis, underscoring the diagnostic challenges associated with COC. The histopathological examination in this case revealed a COC with areas suggestive of an adenomatoid odontogenic tumor, highlighting the potential for diagnostic surprises even in seemingly straightforward clinical scenarios. By presenting this case and comprehensively discussing the clinical and histopathological correlations, this article aims to enhance the diagnostic acumen of dental professionals when faced with lesions that could potentially be calcifying odontogenic cysts. We will explore the differential diagnoses, emphasizing the key features that aid in accurate identification and appropriate management of this complex odontogenic lesion.
Case Presentation: A Diagnostic Misdirection
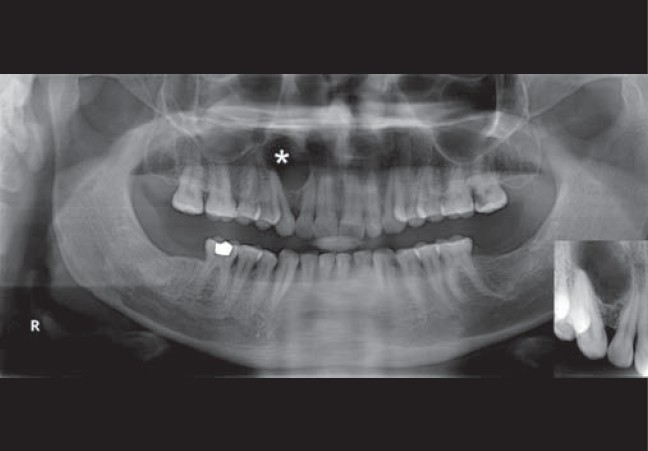
A 43-year-old male electrician presented to our center seeking prosthetic replacement for missing lower posterior teeth. His medical and dental histories were unremarkable, except for previous uneventful extractions of mandibular second and third molars, as well as maxillary third molars, several months prior. Clinical examination revealed no significant abnormalities, except for a subtle, non-tender, hard bulge in the right maxillary canine-lateral incisor region upon palpation. He also exhibited attrition of the anterior teeth. The right maxillary canine and lateral incisor appeared slightly diverged. Several posterior teeth displayed dental caries at various stages. A routine panoramic radiograph unveiled a radiolucent lesion in the right anterior maxilla, measuring 1.7 cm × 1.4 cm Figure 1. This oval, radiolucent lesion was situated in the distal aspect of the lateral incisor root, extending to the apex and mesial part of the maxillary canine root, exhibiting a diffuse margin. Closer examination with periapical radiography indicated that the maxillary right canine root was in close proximity to the lesion, while the lateral incisor showed loss of lamina dura Figure 1. Pulp vitality tests revealed a delayed response in both teeth, suggesting compromised pulpal vitality.
Figure 1.
The patient reported a parafunctional habit, related to his occupation, of repeatedly traumatizing his canines. Based on the patient’s history, radiographic findings, clinical presentation, and pulp vitality tests, a provisional diagnosis of periapical granuloma was established. The clinical differential diagnosis included lateral periodontal cyst, squamous odontogenic tumor, and globulomaxillary cyst. The non-tender clinical bulge was attributed to reactive buccal cortical expansion secondary to a presumed long-standing periapical condition. Root canal treatment was performed on the canine and lateral incisor in a single visit. Curettage of the periapical granuloma was planned post-endodontic treatment.
During surgery, upon elevating a wide semilunar flap, a well-circumscribed area of elevated, thinned buccal cortex was identified Figure 2. Removal of the overlying bone exposed an ovoid, fluctuant swelling, clinically suggestive of a thick capsule. The lesion margins were carefully explored, and the entire lesion was meticulously removed en bloc through blunt dissection Figure 3. The residual bone appeared clear, devoid of any cystic lining Figure 4A. Thorough curettage was performed until healthy bone with pinpoint bleeding was observed. Apicoectomy and retrograde filling were carried out on the lateral incisor and canine. The surgical site was irrigated with Povidone-Iodine and saline, and primary closure was achieved.
Figure 2.
Figure 3.
Figure 4.
Macroscopically, the lesion exhibited a non-specific appearance, except for prominent superficial vasculature Figure 4B and C. The cystic mass was submitted for histopathological examination. Microscopic analysis revealed a cystic lumen lined by a thin layer of odontogenic epithelium (OE). The basal layer of this OE consisted of palisaded columnar or cuboidal cells, resembling ameloblasts, with varying thickness. The hyperchromatic nuclei of these cells were polarized away from the basement membrane. These cells were overlain by loosely arranged epithelial cells resembling stellate reticulum. Notably, numerous epithelial ghost cells, devoid of nuclei, eosinophilic, and retaining their basic cellular outline were present. These ghost cells were often enlarged, of varying shapes, and exhibited well-defined outlines. Some contained nuclear remnants Figure 5.
Figure 5.
In one area of the section, thickening of the OE was observed. In these regions, islands of odontogenic cells were arranged in thin, anastomosing strands exhibiting a plexiform and lattice-work pattern. Towards the center of the lesion in this area, ameloblast-like cells were arranged in ductal or rosette patterns Figure 6. Within the center of this ductal arrangement, a pale, eosinophilic material with varying texture and pattern was identified. Cholesterol clefts were also identified in a specific focus Figure 6B. Based on the comprehensive histopathological findings, a diagnosis of Calcifying Odontogenic Cyst (COC) with Adenomatoid Odontogenic Tumor (AOT)-like areas was rendered.
Figure 6.
Post-operative healing was uneventful, and the patient was followed up for 6 months with no evidence of recurrence.
Differential Diagnosis of Calcifying Odontogenic Cyst
The differential diagnosis of calcifying odontogenic cyst is broad and encompasses a variety of odontogenic cysts and tumors, as well as non-odontogenic lesions that can present with similar clinical or radiographic features. A systematic approach, integrating clinical, radiographic, and histopathological findings, is crucial for accurate diagnosis. Key considerations in the differential diagnosis of COC include:
1. Periapical Lesions (Granuloma and Cyst)
As demonstrated in the presented case, periapical pathologies are common in dental practice and often considered in the initial differential diagnosis of radiolucent lesions in the periapical region. Periapical cysts, in particular, are highly prevalent among odontogenic cysts [1]. Asymptomatic periapical lesions are not uncommon, and their radiographic appearance, typically described as round or ovoid radiolucencies often with a radiopaque margin extending from the lamina dura, can overlap with COC. In enlarging cysts, this sclerotic margin may be less distinct, further complicating differentiation.
Distinguishing Features:
- Clinical Context: Periapical lesions are usually associated with non-vital teeth, often resulting from pulpal necrosis secondary to caries or trauma. COC, while it can be associated with teeth, is developmental in origin and not directly linked to pulpal status in the same way.
- Radiographic Features: While both can present as radiolucencies, COC may exhibit radiopaque foci due to calcifications, which are not typical of periapical lesions unless secondary infection leads to dystrophic calcification. COC can also be associated with unerupted teeth or be located in inter-radicular areas, locations less common for typical periapical lesions.
- Histopathology: The definitive differentiation lies in histopathology. Periapical lesions are characterized by inflammatory infiltrate, granulation tissue, and epithelial rests of Malassez, whereas COC exhibits the characteristic ghost cells and odontogenic epithelial lining described earlier.
2. Lateral Periodontal Cyst
Lateral periodontal cysts are developmental odontogenic cysts that occur along the lateral root surface of vital teeth, typically in the mandibular canine and premolar region. Radiographically, they present as small, well-defined radiolucencies lateral to the root.
Distinguishing Features:
- Tooth Vitality: Lateral periodontal cysts are associated with vital teeth, while the tooth vitality in COC cases can vary depending on the location and size of the lesion.
- Location: Lateral periodontal cysts are strictly lateral to the root, whereas COC can be more variable in location, including periapical, inter-radicular, and supra-osseous locations.
- Radiographic Appearance: Both can be well-defined radiolucencies, but COC may exhibit calcifications and can be larger and more expansile than typical lateral periodontal cysts.
- Histopathology: Histologically, lateral periodontal cysts are lined by thin, non-keratinized stratified squamous epithelium, lacking the ghost cells characteristic of COC.
3. Squamous Odontogenic Tumor (SOT)
Squamous odontogenic tumor is a rare, benign odontogenic neoplasm that can mimic odontogenic cysts radiographically. It typically presents as a triangular radiolucency associated with the cervical region of tooth roots.
Distinguishing Features:
- Radiographic Appearance: SOT often has a triangular shape and is closely associated with the periodontal ligament space, while COC is more variable in shape and location and may contain radiopacities.
- Histopathology: SOT is characterized by islands of benign squamous epithelium within a fibrous stroma, lacking the cystic cavity and ghost cells of COC.
4. Globulomaxillary Cyst (Nasopalatine Duct Cyst – Anterior location)
Globulomaxillary cyst is a historical term for a cyst thought to arise between the maxillary globule and maxillary process. Currently, most lesions in this location are considered to be of odontogenic origin or anteriorly located nasopalatine duct cysts. They typically present in the midline between maxillary central incisors, but lateral presentations can occur.
Distinguishing Features:
- Location: Globulomaxillary cysts (anterior nasopalatine duct cysts) are typically in the midline or paramedian anterior maxilla, while COC can occur in various locations throughout the jaws.
- Radiographic Appearance: Globulomaxillary cysts are often heart-shaped radiolucencies between the roots of central incisors. COC radiographically is more variable and may contain calcifications.
- Histopathology: Nasopalatine duct cysts are lined by respiratory, squamous, or cuboidal epithelium and may contain neurovascular bundles. They lack the ghost cells and odontogenic epithelium characteristic of COC.
5. Adenomatoid Odontogenic Tumor (AOT)
Adenomatoid odontogenic tumor is a benign epithelial odontogenic tumor that often occurs in the anterior maxilla and is frequently associated with impacted canines. The association of COC with AOT, as seen in the presented case, adds complexity to the differential diagnosis.
Distinguishing Features:
- Association with Impacted Teeth: AOT is strongly associated with impacted teeth, particularly canines. COC can also be associated with unerupted teeth, but the association is not as strong or specific as with AOT.
- Radiographic Appearance: AOT typically presents as a well-defined unilocular radiolucency often encompassing the crown and sometimes part of the root of an impacted tooth. COC may have similar radiographic features but can also be multilocular and contain calcifications.
- Histopathology: While the presented case highlights the potential for overlap, classic AOT is characterized by duct-like structures, rosette formations, and eosinophilic amorphous material, lacking the cystic cavity and prominent ghost cells of a pure COC. The presence of both AOT-like areas and classic COC features, including ghost cells, is key to diagnosing the combined lesion.
6. Other Odontogenic Cysts and Tumors
Other odontogenic cysts such as dentigerous cysts, keratocystic odontogenic tumors (KCOTs), and ameloblastomas should also be considered in the differential diagnosis, particularly when COC presents with atypical features or in unusual locations. Each of these lesions has distinct clinical, radiographic, and histopathological characteristics that aid in differentiation.
Diagnostic Modalities for Calcifying Odontogenic Cyst
Accurate diagnosis of COC relies on a combination of diagnostic modalities:
- Clinical Examination: Thorough clinical examination, including palpation, assessment of tooth vitality, and evaluation of any associated signs or symptoms, is the first step.
- Radiographic Evaluation: Radiographs, including periapical radiographs and panoramic radiographs, are essential to assess the location, size, shape, and radiographic characteristics of the lesion. Computed tomography (CT) may be beneficial in complex cases to better visualize calcifications and the extent of the lesion, as noted in the original article [9].
- Histopathological Examination: Histopathological examination of the excised lesion is the gold standard for definitive diagnosis. The identification of ghost cells, odontogenic epithelium, and any associated features, such as AOT-like areas, is crucial for confirming the diagnosis of COC and differentiating it from other lesions.
Discussion: Unraveling the Diagnostic Enigma of COC
The presented case underscores the diagnostic challenges that calcifying odontogenic cysts can pose. Initially misdiagnosed as a periapical lesion due to its asymptomatic nature and radiographic presentation, the case highlights the importance of considering a broad differential diagnosis even for seemingly common presentations. The parafunctional habits of the patient, leading to potential pulpal compromise, further contributed to the initial diagnostic misdirection.
The histopathological findings in this case revealed a COC with areas suggestive of AOT, corroborating existing literature on the association between these two odontogenic entities [3, 5, 6]. Odontogenic epithelium, the origin of odontogenic pathologies, possesses a remarkable capacity for diverse differentiation under the influence of ectomesenchyme. In this context, the proliferation of lesional tissue resembling inner enamel epithelium suggests an inherent ectomesenchymal induction potential. The combined occurrence of COC and other odontogenic pathologies may stem from this inherent plasticity of odontogenic epithelium, allowing for a spectrum of differentiation pathways [7].
The etiopathogenesis of COC in this case could involve a mutated clone of presecretory or postsecretory ameloblasts acquiring mesenchymal induction potential. The characteristic ghost cells, a hallmark of COC, are likely a product of this process. The presence of AOT-like features in certain areas suggests a potential for divergent differentiation within the COC, possibly driven by inductive signals and the inherent pluripotency of the odontogenic epithelium lining the cyst. The observation that duct-forming cells in AOT share similarities with preameloblasts further supports the hypothesis that AOT could potentially evolve from the pluripotent cell lining of COC [8]. This case, along with similar reports, provides evidence for this hypothesis, suggesting that COC may represent a precursor lesion capable of giving rise to other odontogenic tumors.
The presence of cholesterol clefts in this uninfected COC is an unusual finding. While cholesterol clefts are commonly associated with inflammatory cysts like radicular cysts, their presence in COC, particularly in the absence of infection, is less frequently reported. The original article suggests that these cholesterol clefts could be related to degenerating cells within the lesion or possibly associated with bleeding within the cyst [9, 10]. The absence of a sclerotic border radiographically, coupled with the presence of cholesterol clefts, may indicate an actively enlarging lesion.
The case emphasizes the critical importance of clinicopathological correlation in diagnosing rare odontogenic lesions. While conventional radiography may not always reveal pathognomonic features, advanced imaging like CT can enhance diagnostic accuracy, particularly in detecting calcifications. Enucleation remains the standard treatment for COC, and prognosis is generally favorable, especially in cases without aggressive features or associated tumors [2]. Given the benign nature of AOT and the complete removal of the lesion in this case, recurrence is considered unlikely. However, ongoing follow-up is essential to monitor for any potential recurrence and to further document the long-term outcome.
Conclusion
This case report and discussion highlight the diagnostic complexities associated with calcifying odontogenic cysts and emphasize the importance of a comprehensive approach to differential diagnosis. Initial misdiagnosis as a periapical pathology underscores the need for clinicians to maintain a high index of suspicion for unusual lesions, even in seemingly routine clinical scenarios. Intraoperative findings and histopathological examination are crucial for accurate diagnosis and appropriate management. This case serves as a compelling example of a COC exhibiting features suggestive of another odontogenic pathology, reinforcing the concept of COC as a potentially diverse entity within the spectrum of odontogenic lesions. Furthermore, it underscores the necessity of histopathological examination for all enucleated specimens to confirm working diagnoses and to guide appropriate treatment and follow-up strategies, ultimately ensuring optimal patient care.