Campylobacter enteritis presents a diagnostic challenge due to its clinical similarities with various other gastrointestinal illnesses, both viral and bacterial. For children experiencing acute diarrheal conditions, with or without fever or vomiting, pinpointing the exact cause often doesn’t alter the immediate clinical management. Consequently, diagnostic testing isn’t always deemed necessary in these initial stages.
 Campylobacter Outbreak Investigation
Campylobacter Outbreak Investigation
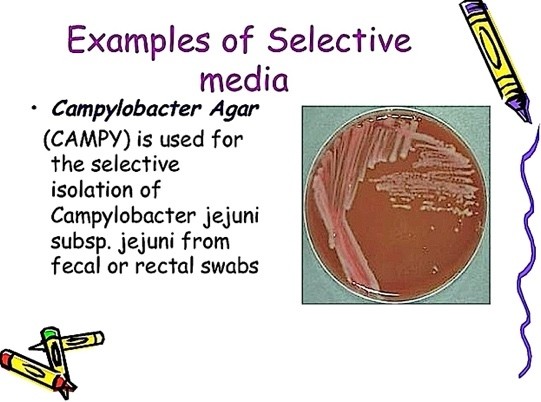
While stool culture remains the established gold standard for identifying Campylobacter species, its isolation using conventional culture media can pose challenges. Optimal Campylobacter growth is achieved on specialized media enriched with selective antibiotics and under microaerobic conditions, characterized by 5% to 10% oxygen, 1% to 10% carbon dioxide, and a trace amount of hydrogen.
A preliminary diagnosis of Campylobacter infection can also be achieved through direct microscopic examination of stool samples. Techniques such as contrast microscopy or Gram staining allow for the visualization of Campylobacter bacteria, distinguished by their characteristic comma-shaped or spiral-shaped morphology as Gram-negative bacilli. While this direct examination offers a rapid presumptive diagnosis, confirmation necessitates subsequent stool culture.
It’s noteworthy that only a fraction of individuals affected by Campylobacter infections seek medical attention and subsequently undergo culture confirmation. For instance, during a Campylobacter outbreak study, a mere 5.4% of identified cases consulted a physician, highlighting potential underreporting and underdiagnosis. Furthermore, instances where patients submit samples for culturing after initiating antibiotic treatment can further impede laboratory Campylobacter growth. Blood cultures are infrequently conducted and, in most instances of Campylobacter infection, bloodstream involvement is absent.
The Role of Culture-Independent Diagnostic Tests (CIDTs) in Campylobacter Detection
In recent years, culture-independent diagnostic tests (CIDTs) have witnessed increased adoption in clinical diagnostics. Data from FoodNET spanning 2016-2019 revealed a significant surge in infections diagnosed via CIDTs, irrespective of whether traditional culture results were positive or negative. Interestingly, the same period also saw an increase in infections diagnosed solely through stool culture methods.
CIDT platforms generally exhibit enhanced sensitivity and offer faster turnaround times compared to traditional culture-based diagnostic approaches. Reverse transcriptase polymerase chain reaction (PCR) testing, a prominent CIDT method, demonstrates a 20% to 40% higher detection rate of Campylobacter in stool samples compared to culture-based methodologies. However, it’s crucial to acknowledge that CIDTs, by detecting nucleic acid presence rather than viable organisms, may present challenges in interpreting clinical significance. The identification of multiple pathogens in a sample is not uncommon with CIDTs and can complicate interpretation. Moreover, CIDTs lack the capability to determine antibiotic susceptibility patterns, a critical aspect in managing Campylobacter infections. Unlike bacteria like Shigella and Salmonella, Campylobacter isolates detected by CIDT are not routinely subjected to culture for further characterization.
Given the prevalent antibiotic resistance to fluoroquinolones and tetracyclines among Campylobacter isolates, culture remains invaluable. In cases necessitating antibiotic treatment, particularly when antibiotic resistance is a concern, culture becomes essential even after initial CIDT identification to guide appropriate antimicrobial therapy.