Introduction
Lung cancer remains the most prevalent cancer globally, and while the lungs are frequent sites for metastases from other primary cancers, the concurrent presentation of primary lung cancer alongside metastatic tumors within the lung is notably rare. Even more exceptional is the phenomenon of tumor-to-tumor metastasis, where one cancer metastasizes into another. This article delves into an extraordinary case involving a patient who presented with primary lung adenocarcinoma, metastasis from colon adenocarcinoma, and the highly unusual occurrence of colon adenocarcinoma metastasizing to lung adenocarcinoma, all discovered simultaneously. This case highlights the complexities of Cancer Differential Diagnosis, particularly in scenarios with multiple lung nodules and diverse tumor origins. Understanding the nuances of differential diagnosis in such cases is crucial for accurate staging, prognosis, and treatment strategies.
Case Presentation
A 61-year-old male with a history of colon adenocarcinoma, for which he underwent a curative colectomy four years prior, presented for routine follow-up. Adjuvant chemotherapy had been administered post-surgery, and annual check-ups were conducted. However, a routine axial CT scan revealed the presence of three distinct pulmonary nodules. One nodule was located in the left upper lobe, exhibiting local pleural adhesion. The remaining two nodules were found in the right upper lobe; one was smaller and in close proximity to the parietal pleura, while the other, larger nodule displayed a pleural tag (Fig 1).
Figure 1.
Subsequent surgical intervention involved wedge resection of the left upper lobe and lumpectomy of the right upper lobe to investigate these findings further and establish a definitive diagnosis through pathological examination. The patient remained under observation and was alive at the last follow-up in January 2013.
Pathology and Differential Diagnosis
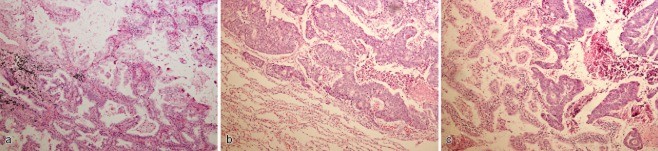
Pathological analysis of the resected specimens revealed distinct characteristics for each nodule, crucial for differential diagnosis. The left upper lobe nodule, measuring 2.5 cm, displayed a peripheral tumor with pleural puckering. Microscopically, this tumor showed a mixed composition of mucinous (30%) and non-mucinous cells (70%). The mucinous component exhibited an acinar growth pattern, while the non-mucinous component displayed a papillary pattern (Fig 2a). Immunohistochemical staining revealed the mucinous cells to be diffusely positive for Cytokeratin 7 (CK7) and focally positive for CK20 and Thyroid Transcription Factor 1 (TTF-1). The non-mucinous cells were diffusely positive for CK7 and TTF-1 but completely negative for CK20. Both cell types were negative for CDX-2. Elastin staining did not indicate visceral pleural invasion. Based on these findings, the differential diagnosis considered primary lung adenocarcinoma, specifically a mixed mucinous and non-mucinous subtype.
The right upper lobe contained two peripheral tumors. The larger nodule (5.5 cm) was homogeneous, exhibiting glandular structures lined by tall-columnar cells with nuclear pseudostratification (Fig 2b). Immunohistochemically, it was CK20+/CDX-2+/CK7−/TTF-1−. These features strongly suggested metastatic colon adenocarcinoma.
The smaller nodule (3.5 cm) in the right upper lobe presented a heterogeneous composition. Approximately one-third mirrored the morphology and immunophenotype of the larger nodule (CK20+/CDX-2+/CK7−/TTF-1−), while the remaining two-thirds displayed a lepidic/papillary structure lined by non-mucinous cells (Fig 2c) with an immunophenotype of CK7+/TTF-1+/CDX-2−/CK20−. Elastin staining confirmed visceral pleural invasion in both right upper lobe tumors. This complex presentation necessitated a differential diagnosis that accounted for both primary lung adenocarcinoma and metastatic colon adenocarcinoma within the same lesion. The final interpretation was colon adenocarcinoma metastasizing to lung adenocarcinoma, representing a tumor-to-tumor metastasis.
Figure 2.
Lymph-vascular invasion and lymph node metastasis were not detected in any of the specimens. The final diagnoses were thus established as: (i) lung adenocarcinoma, mixed mucinous and non-mucinous, in the left upper lobe; (ii) metastasis of colon adenocarcinoma in the right upper lobe (larger nodule); and (iii) colon adenocarcinoma metastasizing to lung adenocarcinoma in the right upper lobe (smaller nodule).
Further molecular analysis using mutation-specific immunohistochemistry for Epidermal Growth Factor Receptor (EGFR) gene mutations revealed additional diagnostic insights. The left upper lobe tumor was positive for the E746_A750 deletion, a common EGFR mutation in lung adenocarcinoma. In contrast, both tumors in the right upper lobe were negative for both E746_A750 and L858R mutations (Fig 3).
Figure 3.
Discussion: Diagnostic Challenges and Tumor-to-Tumor Metastasis
The differential diagnosis in this case was particularly challenging due to the synchronous presentation of multiple lung nodules with varying histopathological and immunohistochemical profiles. In lung adenocarcinoma, the enteric variant, which shares features with colorectal adenocarcinoma, can complicate differential diagnosis. Enteric adenocarcinomas often exhibit glandular structures with columnar cells, similar to metastatic colorectal cancer, and express enteric markers like CDX-2 and CK20. However, primary enteric lung adenocarcinomas can also display features of typical lung adenocarcinoma, such as lepidic growth and CK7/TTF-1 positivity. In this case, the larger right upper lobe nodule displayed a homogeneous enteric morphology and immunophenotype (CK7−/TTF-1−/CDX-2+/CK20+), consistent with metastatic colon adenocarcinoma. The smaller right upper lobe nodule, with its heterogeneous nature – combining enteric and lepidic/papillary patterns with corresponding immunophenotypes – was crucial in establishing the diagnosis of colon adenocarcinoma metastasizing to lung adenocarcinoma.
The 7th Edition of the AJCC Staging Manual emphasizes the reclassification of multiple lung nodules as intrapulmonary metastases rather than synchronous lung primaries (SLP) unless distinct histological types or growth patterns are evident. Adenocarcinomas, with their inherent heterogeneity, pose a greater diagnostic challenge in this regard. Quantifying morphological subtypes and assessing molecular markers like EGFR or KRAS mutations can aid in determining the clonal relationship between multiple nodules. In this case, the left upper lobe tumor (mucinous and non-mucinous adenocarcinoma, EGFR Exon 19 deletion positive) and the pulmonary component of the tumor-to-tumor metastasis in the right upper lobe (non-mucinous, EGFR negative) were considered SLP based on distinct histology and EGFR mutation status, favoring a pT2a(2) staging rather than pT4.
Tumor-to-tumor metastasis, while documented since 1930, remains a rare phenomenon. Renal cell carcinoma is often reported as a recipient tumor, and lung cancer as a donor. The mechanisms behind this are poorly understood, with the seed-and-soil theory suggesting a permissive microenvironment. Molecular biology advancements have implicated various molecules and pathways in site-specific metastasis, such as Kiss-1/metastatin in melanoma lung metastasis. This case underscores the lung’s capacity to act as a recipient in tumor-to-tumor metastasis, adding to the limited literature and highlighting the need for further investigation into the genetic mechanisms driving this unusual event.
Conclusion
This unique case presents a diagnostic challenge in differentiating between primary and metastatic lung cancers, further complicated by the rare occurrence of tumor-to-tumor metastasis. Thorough pathological examination, immunohistochemistry, and molecular analysis were crucial in establishing the accurate differential diagnosis and subsequent staging. This case highlights the importance of considering the possibility of multiple primary cancers and tumor-to-tumor metastasis in patients presenting with complex lung lesions, especially in those with a history of prior malignancies. Further research is warranted to elucidate the underlying mechanisms of tumor-to-tumor metastasis and refine diagnostic approaches for such complex oncological scenarios.
Disclosure
No authors report any conflict of interest.