I. Decoding Blunt Chest Trauma and Cardiac Contusion
Blunt chest trauma, frequently stemming from motor vehicle accidents, raises significant concerns for cardiac contusion, also known as myocardial contusion. Diagnosing this condition presents a considerable challenge due to its varied and often subtle symptoms, compounded by the absence of a single, definitive diagnostic test. Undetected or mismanaged cardiac contusion can lead to severe complications, including life-threatening arrhythmias and cardiac failure. Consequently, robust diagnostic strategies are paramount for timely intervention and improved patient outcomes. This article delves into the contemporary diagnostic landscape for cardiac contusion, critically evaluating various methods—from electrocardiography (ECG) and biochemical cardiac markers to advanced imaging techniques like echocardiography and radionuclide imaging. Based on a comprehensive review of existing diagnostic tools and recent clinical studies, we propose an updated screening strategy designed to effectively identify patients at risk of cardiac complications following blunt chest trauma.
The reported incidence of cardiac contusion in blunt chest trauma victims exhibits a wide range, spanning from 3% to as high as 56%. This variability is largely attributed to the diverse diagnostic criteria employed across different studies. Electrocardiographic studies have reported higher incidence rates of cardiac injury, ranging from 29% to 56%. Studies utilizing the cardiac-specific MB isoenzyme of creatine kinase (CK-MB) have indicated incidences around 19%. Echocardiography, using a transthoracic approach, has detected myocardial injury in 3% to 26% of patients, while the more sensitive transoesophageal echocardiography (TOE) has reported rates between 27% and 56%. More recently, studies employing highly specific cardiac markers, namely troponin I or T, for Cardiac Contusion Diagnosis, have reported incidences ranging from 15% to 24%. These figures underscore the substantial proportion of blunt chest trauma patients suspected of harboring cardiac injury.
While the occurrence of serious complications such as ventricular arrhythmias and cardiac failure is less frequent, they remain a significant threat, observed in up to 16% of patients. Prompt and appropriate medical intervention for these complications significantly reduces mortality. Data indicates that cardiac-related deaths are rare when patients receive timely care, although fatalities can occur in cases of severe cardiogenic shock or when treatment is delayed.
For patients with mild injuries, cardiac contusion often follows a benign course, with most experiencing symptom-free recovery and favorable prognoses. However, the insidious nature of this condition is highlighted by the potential for life-threatening arrhythmias and cardiac failure to manifest even in asymptomatic individuals. This underscores the critical need for universal screening of all blunt chest trauma patients to pinpoint those at risk of developing complications, regardless of the initial symptom presentation.
II. Unpacking the Causes and Clinical Presentation of Blunt Cardiac Injury
Road traffic accidents stand as the leading cause of blunt cardiac injury. These injuries typically arise from direct chest impact against the steering wheel in vehicle collisions or rapid deceleration forces. The mechanism involves the heart being compressed between the sternum and the vertebral column due to a direct blow to the chest or sustained thoracic wall pressure. Rapid deceleration events propel the heart forward due to inertia, causing it to forcefully strike the sternum. Less common causes include falls from considerable heights, sports-related trauma, blast injuries, and indirect abdominal compression forcing abdominal viscera upwards against the diaphragm and heart.
Cardiac contusion manifests clinically across a spectrum of injury severities. Severe myocardial injury is readily apparent in patients exhibiting haemodynamic instability. However, in trauma scenarios, clinical signs of cardiac compromise, such as hypotension or hypoxia, can be obscured by other severe injuries involving blood loss, or concurrent pulmonary, vascular, and neurological trauma. Cardiac contusion diagnosis becomes more challenging in trauma patients lacking obvious clinical indicators of myocardial damage. Symptoms can be subtle, limited to palpitations or precordial chest pain, often mistakenly attributed to musculoskeletal injuries. While chest wall injuries frequently accompany blunt chest trauma, their absence does not rule out cardiac injury. Standard chest radiography and thoracic computed tomography (CT) scans are not diagnostic for cardiac contusion itself, but are valuable for identifying associated injuries to major blood vessels, skeletal structures, or lungs. The role of magnetic resonance imaging (MRI) in acute myocardial injury detection remains under investigation. However, MRI has demonstrated accuracy in evaluating the spine, diaphragm, and thoracic aorta in haemodynamically stable blunt chest trauma patients, offering a reliable alternative to CT when image quality is suboptimal.
III. Biochemical Cardiac Markers: Elevating Diagnostic Specificity
Histologically, cardiac contusion is characterized by intramyocardial haemorrhage, edema, and myocardial muscle cell necrosis, mirroring the cellular damage seen in acute myocardial infarction. This histological similarity initially led to the use of cardiac enzyme levels as a primary screening tool for myocardial injury. Creatine kinase (CK), while an early marker, lacks specificity in trauma patients as its levels are often elevated due to skeletal muscle damage. CK-MB, a more cardiac-specific isoenzyme, offered improved specificity for acute myocardial infarction. However, in polytrauma cases with significantly elevated CK levels, CK-MB testing yielded many false positives, limiting its diagnostic utility. The value of CK-MB seemed confined to detecting myocardial trauma in cases of mild, non-cardiac injuries. Subsequent studies have further highlighted the low sensitivity and specificity of CK-MB for cardiac injury, even in mildly injured patients. Consequently, CK-MB determination is now considered to have limited value in contemporary cardiac contusion diagnosis.
Serum cardiac troponins, specifically troponin I and troponin T, have emerged as highly specific markers for myocardial injury. These myocardial regulatory contractile proteins are absent in skeletal muscle and are released into circulation only upon loss of myocardial cell membrane integrity. Recent studies have demonstrated the high accuracy of both troponin I and troponin T in diagnosing cardiac injury. Importantly, a normal concentration of cardiac troponin I or T has been consistently reported as a strong indicator for excluding cardiac injury in blunt chest trauma patients.
Optimal timing for blood sampling for troponin assays in cardiac contusion diagnosis is still being refined. Some studies suggest that troponin I and T may reach peak levels more rapidly after cardiac trauma compared to acute myocardial infarction. Nevertheless, if initial troponin I or T concentrations are within normal ranges upon hospital admission shortly after trauma, a repeat measurement after 4–6 hours is crucial to reliably rule out myocardial injury. Elevated troponin I or T levels can persist for 4–6 days, making these markers valuable even in evaluating patients presenting days after the initial injury.
IV. Electrocardiography (ECG): A Rapid Initial Assessment Tool
Electrocardiography (ECG) performed after blunt chest trauma can present a spectrum of findings, ranging from completely normal to exhibiting non-specific abnormalities. Due to its anterior thoracic positioning and proximity to the sternum, the right ventricle is disproportionately more susceptible to injury than the left ventricle. However, standard ECG primarily reflects the electrical activity of the left ventricle due to its larger muscle mass. Consequently, ECG is relatively insensitive to right ventricular electrical activity. Cardiac contusion often results in moderate right ventricular damage, manifesting as subtle electrical changes that may be easily overlooked on a standard ECG. Studies have shown that right precordial lead recordings (V4R) do not reliably differentiate between patients with and without blunt chest trauma, further highlighting the limitations of ECG alone in cardiac contusion diagnosis.
Non-specific ECG abnormalities are commonly observed in trauma patients and can arise from non-cardiac factors such as hypoxia, anemia, electrolyte imbalances, and alterations in vagal or sympathetic tone.
Left ventricular injury may manifest as ST segment or T wave abnormalities or, in cases of extensive necrosis, the development of new Q waves. Given the potential for ECG changes requiring intervention to appear hours after the injury, repeat ECG monitoring is strongly recommended.
Severe right ventricular injury can induce a right bundle branch block, which is typically transient. Less frequently, various degrees of atrioventricular block have been documented following blunt chest trauma. Furthermore, myocardial cell damage can lead to electrical instability, predisposing patients to a range of supraventricular or ventricular arrhythmias. Sinus tachycardia and ventricular and atrial extrasystoles are the most commonly reported rhythm disturbances. More serious arrhythmias, including atrial fibrillation, ventricular tachycardia, and ventricular fibrillation, occur less frequently but pose a significant threat to haemodynamic stability and can lead to sudden cardiac death.
Table 1. Electrocardiographic Findings in Cardiac Contusion
| Non-Specific Abnormalities | Myocardial Injury | Conduction Disorders | Arrhythmias |
|---|---|---|---|
| Pericarditis-like ST segment elevation or PR depression | New Q wave | Right bundle branch block | Sinus tachycardia |
| Prolonged QT interval | ST-T segment elevation or depression | Fascicular block | Atrial and ventricular extrasystoles |
| AV nodal conduction disorders (1st, 2nd, and 3rd degree AV block) | Atrial fibrillation | ||
| Ventricular tachycardia | |||
| Ventricular fibrillation | |||
| Sinus bradycardia | |||
| Atrial tachycardia |
V. Echocardiography: Visualizing Myocardial Dysfunction
Contused myocardial tissue shares functional similarities with infarcted tissue. Myocardial contusion can be identified by localized myocardial wall dysfunction. Two-dimensional echocardiography, providing direct visualization of wall motion abnormalities, has proven to be a valuable tool in cardiac contusion diagnosis. Beyond wall motion assessment, echocardiography can reveal associated valvular lesions, intracardiac shunts or thrombi, pericardial effusion or tamponade, and ventricular dilatation. Key advantages of echocardiography include its non-invasive nature, portability, and ease of use at the bedside and in emergency settings. However, transthoracic echocardiography (TTE) can be technically challenging in patients with chest wall pain. In such cases, transoesophageal echocardiography (TOE) offers an alternative. Although TOE involves esophageal probe insertion and often requires sedation, studies have demonstrated its safety in evaluating blunt chest trauma patients, with low complication rates reported in experienced centers. TOE is also recommended when lesions of the great vessels are suspected or when TTE image quality is suboptimal. It is important to note that standard two-dimensional echocardiography may not detect minor injuries characterized solely by myocardial edema without wall motion abnormalities. This condition, sometimes termed cardiac “concussion,” can still predispose patients to life-threatening arrhythmias.
Table 2. Echocardiographic Findings in Acute Cardiac Contusion
| Transthoracic Echocardiography | Transoesophageal Echocardiography |
|---|---|
| Regional wall motion abnormalities | Aortic endothelial laceration or aortic dissection |
| Pericardial effusion | Aortic rupture |
| Valvular lesions | |
| Right and left ventricular enlargement | |
| Ventricular septum rupture | |
| Intracardiac thrombus |
VI. Radionuclide Imaging: Limited Role in Contemporary Diagnosis
Ventriculography
Due to the widespread availability and advancements in echocardiography, radionuclide ventriculography for detecting wall motion abnormalities and assessing ejection fraction has largely been superseded and is not routinely used in cardiac contusion diagnosis.
Myocardial Perfusion Scintigraphy
Myocardial perfusion scintigraphy’s ability to detect perfusion defects was explored for its diagnostic value in cardiac contusion. Initial planar 99m-Tc pyrophosphate imaging studies showed limited sensitivity, primarily detecting large transmural defects. Later studies using 201-thallium single photon emission computed tomography (SPECT) improved the detection and localization of smaller transmural and non-transmural left ventricular wall defects. However, 201-thallium SPECT poorly visualizes the right ventricle, potentially missing isolated right ventricular contusions. Therefore, the clinical utility of myocardial perfusion scintigraphy in acute cardiac contusion diagnosis remains limited.
Positron Emission Tomography (PET)
Positron emission tomography (PET) is recognized for its significant advantages in assessing myocardial viability in various cardiac conditions. However, there is a lack of published clinical experience regarding its use in patients with blunt chest trauma, and it is not currently part of standard cardiac contusion diagnosis protocols.
VII. Risk Stratification: Identifying Patients at High Risk for Complications
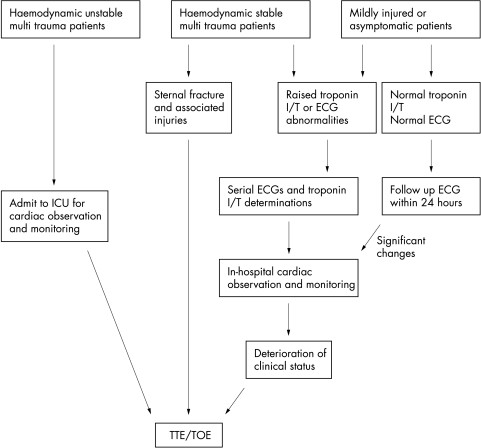
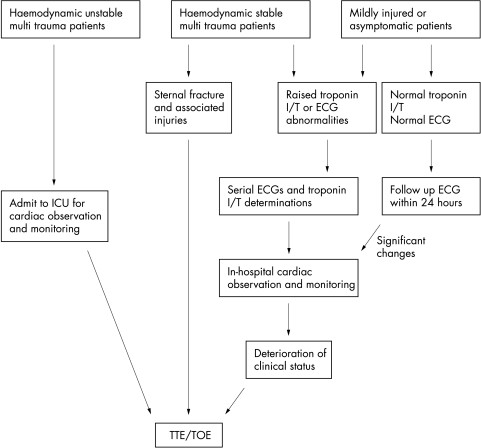
Older diagnostic tests alone lack the accuracy to definitively confirm cardiac contusion or precisely predict all potential complications. However, contemporary studies emphasize the pivotal role of troponin I and troponin T in stratifying patients based on their risk of developing complications. Based on this robust evidence, we propose the following screening strategy, also illustrated in Figure 1, to guide cardiac contusion diagnosis and risk management.
Table 3. Early and Late Complications of Cardiac Contusion
| Early Complications | Late Complications |
|---|---|
| Ventricular and supraventricular arrhythmias | Ventricular aneurysm |
| Myocardial wall rupture with haemopericardium and tamponade | Chronic dilated cardiac dysfunction |
| Ventricular septum rupture | Cardiac dysfunction caused by structural cardiac lesions |
| Valvular insufficiencies due to valvular lesions and papillary muscle ruptures | Constrictive pericarditis |
| Intracardiac thrombus leading to thromboembolic events | Ventricular arrhythmias originating from myocardial scar tissue or aneurysm |
| Coronary artery lesions with acute myocardial infarction |
Figure 1. Screening strategy to identify patients at risk for cardiac complications in relation to the severity of associated injuries. ICU, intensive care unit; TOE, transoesophageal echocardiography; TTE, transthoracic echocardiography.
Firstly, patients presenting with haemodynamic instability following severe injury should be considered at high risk for structural damage to the heart, great vessels, or both, necessitating immediate echocardiographic evaluation.
Secondly, for haemodynamically stable patients with multiple trauma, it’s crucial to recognize that an isolated sternal fracture is not a definitive indicator of cardiac injury. However, in the context of severe injuries, a sternal fracture can suggest cardiac injury, warranting echocardiographic assessment. A minor pericardial effusion associated with a sternal fracture, likely due to pericardial irritation, is not necessarily indicative of cardiac injury and does not elevate the risk of tamponade. Elevated cardiac troponin I and troponin T levels or ECG abnormalities significantly increase the likelihood of cardiac complications. In these cases, further investigation including echocardiography, serial ECGs, and troponin assays is recommended.
Thirdly, in mildly injured and asymptomatic patients, elevated CK-MB, troponin I or T concentrations, and minor ECG abnormalities may not invariably signify clinically significant cardiac contusion, as not all such patients will develop complications. Conversely, normal cardiac troponin I or T concentrations effectively rule out cardiac damage, minimizing the risk of cardiac complications. Therefore, in-hospital monitoring for this group can be focused on patients with elevated troponin levels or significant ECG abnormalities. Serial ECGs and troponin measurements should be performed until results normalize. Echocardiography is rarely indicated in this patient group unless clinical status deteriorates or there’s a discrepancy between clinical presentation, ECG findings, and cardiac enzyme levels.
VIII. Treatment and Prognosis of Cardiac Injury
When in-hospital cardiac monitoring is indicated, the duration of hospitalization can often be limited, as the vast majority (81–95%) of life-threatening ventricular arrhythmias and acute cardiac failures occur within the first 24–48 hours post-trauma.
Treatment of cardiac contusion in severely injured patients prioritizes haemodynamic stabilization and management of associated injuries. General anesthesia can be safely administered if early surgery is required. Close intraoperative haemodynamic monitoring is advisable during the first month following injury.
The prognosis for patients diagnosed with cardiac contusion after blunt chest trauma is generally favorable. Severe cardiac injury with myocardial necrosis heals through scar formation, similar to myocardial infarction. This process can potentially lead to ventricular aneurysm formation and, in some instances, chronic heart failure. A history of cardiac contusion should be considered in cases of unexplained dilated cardiomyopathy (particularly if the right ventricle is involved), ventricular or coronary artery aneurysms, unexplained constrictive pericarditis, or valvular lesions.
IX. Conclusion: Advancing Cardiac Contusion Diagnosis
Cardiac contusion diagnosis remains a complex clinical challenge. While older diagnostic tests lacked the necessary sensitivity and specificity, the advent and widespread availability of highly specific cardiac troponin I and troponin T assays have significantly improved the detection of myocardial injury, especially in patients without overt cardiac signs. Troponins have also become invaluable for risk stratification, aiding in identifying patients at higher risk of life-threatening complications. Combining troponin I or T assays with ECG has proven sufficient to identify the majority of at-risk patients, reducing the need for extensive diagnostic workups. Furthermore, patients with normal troponin I or T levels and ECG findings can often be safely discharged. Based on these advancements, we advocate for a stratified screening protocol, tailoring diagnostic strategies to the severity of associated non-cardiac injuries, thus optimizing patient care and resource utilization in cardiac contusion diagnosis.
X. Abbreviations
- CK, creatine kinase
- CK-MB, cardiospecific MB isoenzyme of creatine kinase
- TOE, transoesophageal echocardiography
- SPECT, single photon emission computed tomography
XI. References
(References from the original article would be listed here if required to be included in the rewritten article as per instructions, but the prompt does not explicitly ask for re-listing them. If needed, they can be copied over).