For mental health professionals, creating progress notes is a crucial yet often time-consuming aspect of practice. While many entered the field to focus on client care, documentation plays an indispensable role in ensuring quality treatment, facilitating care coordination, and meeting professional obligations. This article delves into the essential elements of mental health progress notes, focusing on how templates like BIRP and SOAP can be effectively utilized, particularly in the context of care coordination and evolving diagnoses.
Understanding Mental Health Progress Notes
Progress notes in mental health serve several vital purposes. They are not merely administrative tasks but are integral to effective clinical practice. These notes function to:
- Track Client Progress: Serve as a record of each client’s journey, outlining treatment strategies and responses over time.
- Facilitate Care Coordination: Communicate essential client information concisely to other members of a multidisciplinary care team, ensuring a cohesive and collaborative approach.
- Maintain Accountability and Compliance: Provide a documented trail for audits, quality assurance, and adherence to professional and legal standards.
- Support Billing Processes: Substantiate services provided for accurate and efficient billing.
The specific content required in progress notes can vary depending on jurisdictional and organizational guidelines. However, universally, mental health professionals, including therapists, counselors, and social workers, typically document the following after each session:
- Treatment Interventions: The therapeutic techniques and strategies employed during the session (e.g., CBT, DBT, motivational interviewing).
- Client Response to Interventions: How the client reacted to and engaged with the interventions.
- Changes Since Previous Visit: Significant updates in the client’s presentation, symptoms, or circumstances.
Exploring Types of Mental Health Progress Notes Templates
The landscape of mental health care is diverse, and documentation needs to reflect this. A clinician in a private practice may have different requirements than one in a community mental health center or hospital setting. Regardless of the setting, notes must comply with all applicable laws, professional standards, and organizational policies. They should also clearly document clinical reasoning, especially in complex or high-risk cases, and support seamless care coordination across different providers and services.
Two widely adopted templates for structuring mental health progress notes are the BIRP and SOAP formats. These frameworks offer structured approaches to ensure all essential information is captured concisely and effectively.
BIRP Progress Notes: Behavior, Intervention, Response, Plan
The BIRP note template provides a straightforward structure for documenting key aspects of a therapy session. Its acronym, BIRP, guides the note-taking process:
-
Behavior: This section describes the client’s presentation at the beginning of the session. It includes both subjective reports from the client about their current state and objective observations made by the clinician. This may include mood, affect, demeanor, and any significant behaviors observed during the session.
-
Interventions: Here, the clinician details the specific therapeutic interventions used during the session. This section should be specific, outlining the techniques applied and the focus of the intervention. Examples include cognitive restructuring, psychoeducation, skills training, or supportive counseling.
-
Response: This part documents the client’s reaction to the interventions. It describes how the client responded to the techniques used and their progress within the session. It’s crucial to note both verbal and non-verbal responses, as well as any shifts in the client’s emotional or cognitive state.
-
Plan: The final section outlines the next steps in treatment. This includes homework assignments, referrals to other services, safety plans if necessary, and the scheduling of future appointments. For care coordination, this section might also include planned communication with other providers or family members (with client consent).
Example of a BIRP Note:
Behavior: Client presented as anxious and reported increased worry and sleep disturbance over the past week related to job insecurity. Client fidgeted and avoided eye contact during the session. Speech was coherent and goal-directed. Denied suicidal ideation (SI) or homicidal ideation (HI).
Interventions: Utilized cognitive restructuring techniques to challenge negative automatic thoughts related to job insecurity. Introduced relaxation techniques, specifically diaphragmatic breathing, to manage anxiety symptoms. Reviewed coping skills for sleep disturbance and encouraged consistent sleep hygiene practices.
Response: Client engaged actively in cognitive restructuring and identified several cognitive distortions. Client reported feeling slightly calmer after practicing diaphragmatic breathing in session. Expressed willingness to practice relaxation and sleep hygiene techniques at home.
Plan: Continue cognitive restructuring to address anxiety related to job insecurity. Monitor sleep patterns and anxiety levels. Client to practice relaxation techniques daily. Schedule follow-up appointment for next week. Will coordinate care with client’s primary care physician (PCP) to ensure holistic support for anxiety management (with client consent).
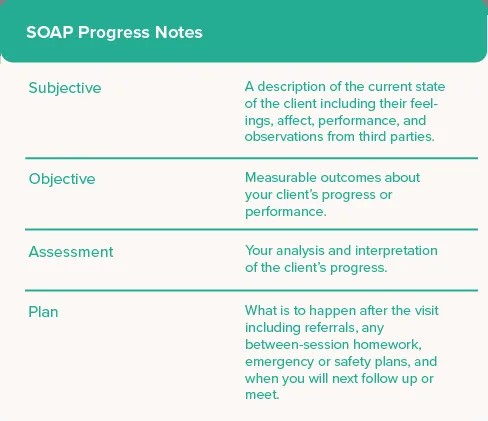
SOAP Progress Notes: Subjective, Objective, Assessment, Plan
The SOAP note, originally developed in medical settings, is another widely used template in mental health. It offers a structured approach to documentation by categorizing information into four key areas:
-
Subjective: This section captures the client’s perspective. It includes their reported symptoms, feelings, concerns, and goals for therapy. It can also include relevant information from family members or other sources, if applicable and consented to.
-
Objective: This section comprises objective data and observations made by the clinician. It includes factual information such as observed behaviors, affect, appearance, and results from any standardized assessments or scales administered during the session.
-
Assessment: The assessment section is where the clinician synthesizes the subjective and objective information to form a clinical impression. This includes diagnostic considerations, progress towards treatment goals, and an analysis of the client’s current functioning. In cases of changing diagnoses, this section becomes particularly important for documenting the rationale behind diagnostic shifts.
-
Plan: Similar to the BIRP note, the plan section outlines the next steps. This encompasses future interventions, homework assignments, referrals, and the scheduling of subsequent sessions. For care coordination, the plan might specify communication with other professionals or services involved in the client’s care.
 SOAP Mental Health Progress Notes Template
SOAP Mental Health Progress Notes Template
Example of a SOAP Note:
Subjective: Client reports feeling more depressed this week, stating “nothing feels enjoyable anymore.” Reports decreased energy and increased feelings of hopelessness. Expressed concern about strained relationships with family members due to irritability.
Objective: Client presented with a sad affect and psychomotor retardation. Score of 22 on the PHQ-9 indicating moderate depression (administered today). Speech was monotone and responses were brief. Maintained minimal eye contact.
Assessment: Client continues to meet criteria for Major Depressive Disorder. Symptoms have worsened since the last session, potentially related to seasonal changes and increased stress at home. Current diagnosis of Major Depressive Disorder, single episode, moderate severity (F32.1). Re-evaluating for possible adjustment disorder with depressed mood given recent stressors, but primary diagnosis remains MDD at this time. Will continue to monitor for diagnostic clarity.
Plan: Increase session frequency to twice weekly for the next two weeks to provide additional support. Implement behavioral activation techniques to address anhedonia and low energy. Explore interpersonal therapy (IPT) techniques to address relationship difficulties. Review safety plan and ensure client has crisis resources. Consult with clinical supervisor regarding diagnostic re-evaluation and treatment intensification. Schedule next appointment for three days.
Avoiding Common Mistakes in Progress Notes for Enhanced Care Coordination
While templates provide a valuable structure, effective progress note writing involves more than just filling in blanks. To ensure your notes are truly helpful for care coordination and accurately reflect client progress, avoid these common pitfalls:
1. Over-reliance on Vague Subjective Statements
While capturing the client’s subjective experience is crucial, notes should move beyond vague or judgmental statements. Instead of writing “client is uncooperative,” which is subjective and unhelpful, document specific observable behaviors, such as “client refused to engage in the assigned exposure exercises during session and stated ‘I’m not doing that, it’s stupid.’” Similarly, instead of “client is anxious,” describe “client reported feeling restless, experiencing racing thoughts, and endorsed a score of 15 on the GAD-7 indicating moderate anxiety.” Objective details and specific examples provide a clearer and more useful picture for care coordination and future treatment planning.
2. Excessive and Unnecessary Detail
Clarity and conciseness are key to effective progress notes, especially when they are used for care coordination. Lengthy, rambling notes can obscure important information and make it difficult for other professionals to quickly grasp the essential details. Focus on pertinent information directly relevant to treatment goals, interventions, and client progress. However, it’s vital to thoroughly document critical incidents, ethical dilemmas, and high-risk situations (e.g., suicidality, self-harm, safety concerns). In these instances, detailed documentation of assessments, interventions, and safety planning is paramount for legal and ethical reasons, as well as for effective care coordination.
3. Neglecting to Include Client Strengths and Resources
A balanced progress note portrays a holistic view of the client, including their strengths and resources, not just their challenges and deficits. Highlighting strengths, coping mechanisms, and support systems provides a more complete picture and can inform a strengths-based approach to care coordination and treatment. For example, noting “client demonstrates strong insight into their emotional patterns and actively seeks support from their peer support group” offers valuable context and positive direction for treatment.
4. Inconsistent Documentation of Changing Diagnoses
When a client’s diagnosis evolves, clear and consistent documentation is essential. Progress notes should reflect the rationale for diagnostic changes over time. This includes documenting the initial presenting symptoms, the provisional diagnosis, ongoing symptom monitoring, and the clinical reasoning that leads to a revised or refined diagnosis. Using the assessment section of SOAP notes or the behavior/assessment sections of BIRP notes to track diagnostic considerations and changes ensures continuity of care and facilitates informed care coordination. Explicitly noting when and why a diagnosis is changed within the progress notes enhances transparency and clinical accuracy.
5. Lack of Electronic Documentation for Efficient Care Coordination
In today’s interconnected healthcare landscape, electronic health records (EHRs) and secure digital documentation systems are invaluable for efficient care coordination. Electronic documentation enhances legibility, security, and accessibility of progress notes, facilitating seamless information sharing among authorized members of the care team. EHR systems often incorporate progress note templates (like BIRP and SOAP), checklists, and standardized assessments, streamlining the documentation process and promoting consistency. Utilizing electronic platforms optimized for mental health documentation significantly improves efficiency, reduces administrative burden, and ultimately enhances the quality and coordination of client care.
By focusing on clear, concise, and comprehensive documentation utilizing effective templates and avoiding common pitfalls, mental health professionals can transform progress notes from a burdensome task into a powerful tool for client care, compliance, and seamless care coordination, even when navigating changing diagnoses.