Hydrocele is a prevalent condition, often benign, marked by fluid accumulation within the tunica vaginalis, the sac surrounding the testicle. This leads to scrotal swelling and is commonly observed in newborns and older men. While usually painless, hydroceles can cause discomfort and aesthetic concerns, necessitating proper diagnosis and management. Effective nursing care is crucial in addressing patient needs, providing comfort, and ensuring optimal outcomes. This article delves into the essential aspects of hydrocele, focusing on nursing diagnoses, comprehensive care plans, and targeted interventions to guide healthcare professionals in providing patient-centered care.
Understanding Hydrocele
What is Hydrocele?
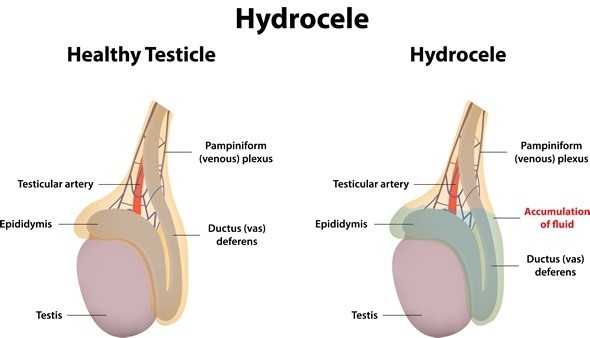
A hydrocele is fundamentally a collection of serous fluid that builds up within the tunica vaginalis, which is a membrane-covered sac enclosing the testicle. In simpler terms, it’s like having a water balloon around the testicle. This fluid originates from the peritoneal cavity and accumulates due to either overproduction or insufficient absorption. Hydroceles can occur on one or both sides of the scrotum.
Types of Hydroceles: Communicating vs. Non-communicating
Hydroceles are broadly classified into two types based on the connection between the tunica vaginalis and the abdominal cavity:
- Communicating Hydrocele: This type occurs when the processus vaginalis, a channel that normally closes after birth, remains open. This open channel allows peritoneal fluid from the abdomen to flow into the scrotum, leading to fluid accumulation. The size of a communicating hydrocele may fluctuate, often increasing during the day with activity and decreasing at night when lying down.
- Non-communicating Hydrocele: In this type, the processus vaginalis is closed, but fluid still accumulates within the tunica vaginalis. This can be due to excessive fluid production by the tunica vaginalis itself or impaired fluid absorption. Non-communicating hydroceles typically maintain a consistent size.
Pathophysiology of Hydrocele
The development of a hydrocele involves an imbalance between the production and absorption of fluid within the scrotum. This imbalance can stem from various factors, leading to either an excess of fluid entering the scrotal sac or a deficiency in the removal of fluid.
- Communicating Hydroceles: Result from the persistence of the processus vaginalis. This patent channel allows peritoneal fluid to drain into the scrotum. Activities that increase abdominal pressure, like coughing or straining, can exacerbate fluid flow and increase hydrocele size.
- Non-communicating Hydroceles: Arise from issues within the scrotum itself.
- Increased Fluid Production: Trauma, inflammation, or infection within the scrotum can stimulate the tunica vaginalis to produce more fluid than can be reabsorbed. In older children, viral infections have been linked to sudden hydrocele onset, possibly due to virus-mediated serositis.
- Impaired Fluid Absorption: Blockage of lymphatic drainage in the scrotum can hinder fluid absorption, leading to hydrocele formation. Filariasis, a parasitic infection common in tropical regions, is a known cause of lymphatic obstruction and hydroceles.
Causes and Risk Factors
Hydroceles can be caused by a range of factors, varying depending on age and geographic location:
- Congenital Factors (Infants): The most common cause in newborns and infants is the failure of the processus vaginalis to close completely after birth, leading to a communicating hydrocele.
- Infection:
- Filariasis: In tropical and subtropical regions, filariasis, caused by parasitic worms like Wuchereria bancrofti, is a major cause of hydroceles in adults. The parasites obstruct lymphatic vessels, impairing fluid drainage.
- Epididymitis or Orchitis: Infections of the epididymis or testicle can cause inflammation and increased fluid production, leading to a secondary hydrocele.
- Trauma or Injury: Direct injury to the scrotum can trigger inflammation and fluid accumulation, resulting in a hydrocele.
- Surgery: Inguinal surgery, hernia repair, or even laparoscopic procedures can sometimes lead to hydrocele formation, possibly due to disruption of lymphatic drainage or inadequate irrigation fluid aspiration post-surgery.
- Testicular Tumors: In rare cases, a hydrocele may develop as a secondary sign of a testicular tumor.
Clinical Manifestations and Assessment
The primary symptom of a hydrocele is a painless swelling in the scrotum. Other clinical manifestations include:
- Scrotal Swelling: A noticeable enlargement of one or both sides of the scrotum is the hallmark sign. The swelling is typically soft and fluid-filled.
- Palpable Fullness: On physical examination, the hydrocele feels like a smooth, cystic mass surrounding the testicle. It is usually non-tender to palpation.
- Transillumination: A key diagnostic sign is positive transillumination. When a light is shone from behind the scrotum, the hydrocele transilluminates, meaning light passes through the fluid-filled sac, creating a reddish glow without internal shadows. This helps differentiate hydroceles from solid masses.
- Discomfort (Variable): While typically painless, large hydroceles can cause a dragging sensation, pressure, or discomfort in the scrotum, especially with prolonged standing or activity.
- Size Fluctuation (Communicating Hydrocele): Communicating hydroceles may vary in size throughout the day, being smaller in the morning and larger in the evening or after physical exertion.
Diagnosis of Hydrocele
Diagnosis is usually straightforward and based on clinical assessment.
- Physical Examination: A thorough physical exam, including palpation of the scrotum and transillumination, is often sufficient for diagnosis.
- Ultrasound: Scrotal ultrasound is a valuable imaging technique to confirm the diagnosis, especially when the physical exam is inconclusive. It can visualize the fluid collection, rule out testicular masses or hernias, and differentiate between cystic and solid lesions.
- Blood and Urine Tests: May be ordered to rule out infection or other underlying conditions, especially if there are signs of inflammation or pain.
Nursing Diagnoses for Hydrocele
Based on the assessment findings, relevant nursing diagnoses for a patient with hydrocele may include:
- Pain related to scrotal swelling and pressure.
- Risk for Infection related to surgical intervention (if performed).
- Anxiety related to the condition, potential treatment, and body image concerns.
- Disturbed Body Image related to scrotal enlargement and perceived cosmetic changes.
- Deficient Knowledge regarding hydrocele, treatment options, and self-care measures.
Nursing Care Plan and Interventions
The nursing care plan for a patient with hydrocele is tailored to address the specific nursing diagnoses and patient needs. Key nursing interventions include:
Pain Management
- Assess Pain: Regularly assess the patient’s pain level using a pain scale. Note the location, character, onset, duration, and aggravating/relieving factors of pain.
- Comfort Measures: Provide comfort measures such as scrotal support using a rolled towel or athletic supporter to reduce pressure and discomfort.
- Pharmacological Management: Administer prescribed analgesics, such as mild pain relievers like acetaminophen or ibuprofen, as needed for pain relief.
- Non-pharmacological Pain Relief: Encourage non-pharmacological methods like rest, elevation of the scrotum, and application of cool compresses (as prescribed) to reduce swelling and pain.
Infection Prevention (Post-Surgical)
- Monitor Surgical Site: Assess the surgical site for signs of infection, including redness, warmth, swelling, drainage, and increased pain.
- Wound Care: Perform wound care as prescribed, maintaining aseptic technique during dressing changes.
- Hygiene: Educate the patient on maintaining proper hygiene, including handwashing and keeping the surgical site clean and dry.
- Administer Antibiotics: Administer prophylactic antibiotics as prescribed to prevent post-operative infections.
Anxiety Reduction
- Provide Information: Educate the patient about hydrocele, its causes, treatment options, and prognosis in a clear and understandable manner. Address any misconceptions or fears.
- Therapeutic Communication: Encourage the patient to express their concerns and anxieties. Provide emotional support and reassurance.
- Address Body Image Concerns: Acknowledge the patient’s potential concerns about scrotal appearance. Offer reassurance and emphasize that hydrocele treatment can restore normal appearance.
Body Image Improvement
- Education and Reassurance: Provide education about the benign nature of most hydroceles and the availability of effective treatments.
- Promote Acceptance: Encourage open communication and address any feelings of self-consciousness or embarrassment related to the condition.
- Support Groups (If Applicable): If appropriate, suggest support groups or online forums where patients can connect with others who have experienced similar conditions.
Patient Education
- Hydrocele Information: Explain what a hydrocele is, its causes, and the importance of treatment if recommended.
- Treatment Options: Discuss available treatment options, including observation, aspiration, sclerotherapy, or surgery, outlining the benefits and risks of each.
- Post-operative Care (If Surgical): Provide detailed instructions on post-operative care, including wound care, pain management, activity restrictions, and follow-up appointments.
- Signs and Symptoms to Report: Educate the patient on signs and symptoms that warrant immediate medical attention, such as increased pain, redness, swelling, fever, or drainage from the surgical site.
- Self-Care Measures: Advise on self-care measures like scrotal support, avoiding heavy lifting or strenuous activity during recovery, and maintaining good hygiene.
Medical and Surgical Management
Medical and surgical management options for hydrocele include:
- Observation: For asymptomatic hydroceles, especially in newborns, observation may be the initial approach, as many resolve spontaneously within the first year of life.
- Needle Aspiration: Involves draining the fluid from the hydrocele using a needle. However, recurrence rates are high with aspiration alone.
- Sclerotherapy: Following aspiration, a sclerosing agent (e.g., tetracycline or doxycycline) is injected into the hydrocele sac to cause scarring and prevent fluid re-accumulation. Sclerotherapy is also associated with recurrence and potential complications.
- Surgery (Hydrocelectomy): Surgical removal of the hydrocele sac is the most definitive treatment, especially for large, symptomatic, or communicating hydroceles. Surgical approaches include inguinal or scrotal incisions, with techniques like sac excision or eversion and suturing.
Prognosis and Prevention
The prognosis for hydrocele treatment is generally excellent. Surgical correction is usually successful in resolving the hydrocele with low recurrence rates. Preventing hydroceles is not always possible, particularly congenital hydroceles. However, minimizing scrotal trauma and promptly treating infections of the testicles and epididymis may help reduce the risk of acquired hydroceles.
Conclusion
Effective nursing care is integral to the comprehensive management of hydrocele. By utilizing appropriate nursing diagnoses, developing individualized care plans, and implementing targeted interventions, nurses play a vital role in alleviating patient discomfort, reducing anxiety, promoting positive body image, and ensuring successful treatment outcomes. Patient education is paramount in empowering individuals to understand their condition, actively participate in their care, and adhere to recommended self-care measures for optimal recovery and well-being.