Idiopathic Multicentric Castleman Disease (iMCD) is a rare and severe condition that can be life-threatening if not diagnosed and treated promptly. For years, the absence of clear diagnostic guidelines has posed a significant challenge for clinicians. This article delves into the groundbreaking consensus diagnostic criteria for iMCD, providing a detailed understanding for healthcare professionals and those seeking in-depth information on this complex disease. These newly established Castleman Disease Diagnosis Criteria are crucial for accurate identification, effective treatment, and advancing research in iMCD.
Major Criteria for iMCD Diagnosis: Essential Cornerstones
The diagnosis of iMCD hinges on meeting two major criteria, ensuring a solid foundation for identifying this distinct condition. These criteria, developed by an international panel of experts, are based on extensive clinical data and histopathological analysis.
Histopathologic Lymph Node Features: Unveiling the Microscopic Hallmarks
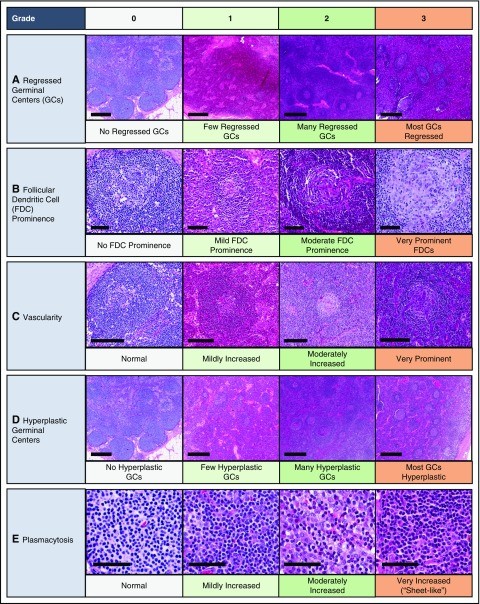
The first major criterion focuses on the characteristic changes observed in lymph node tissue under a microscope. A biopsy of an enlarged lymph node is essential to assess these histopathologic features. The castleman disease diagnosis criteria emphasize that the lymph node must exhibit features consistent with the iMCD spectrum. These features include a combination of:
- Regressed/Atrophic Germinal Centers: Often displaying concentric rings of lymphocytes in an “onion skinning” pattern around the atrophied centers.
- Follicular Dendritic Cell (FDC) Prominence: An increased visibility and presence of FDCs within the lymph node structure.
- Vascularity: Increased blood vessel formation, often with prominent endothelial cells in the areas between follicles and vessels penetrating into the germinal centers, sometimes described as a “lollipop” appearance.
- Polytypic Plasmacytosis: An abundance of plasma cells in the interfollicular regions, indicating a polyclonal proliferation.
- Hyperplastic Germinal Centers: In some cases, germinal centers may be enlarged and overactive.
To meet this major criterion for castleman disease diagnosis criteria, the lymph node histopathology must demonstrate at least a grade 2 or 3 severity for either regressed germinal centers or plasmacytosis, alongside other features within the iMCD spectrum.
Multicentric Lymphadenopathy: Widespread Lymph Node Enlargement
The second major criterion is multicentric lymphadenopathy, meaning enlarged lymph nodes in multiple regions of the body. Specifically, this criterion requires enlarged lymph nodes (≥1 cm in short-axis diameter) in two or more lymph node stations. This widespread lymph node involvement distinguishes iMCD from unicentric Castleman disease, which affects only a single lymph node region. Imaging techniques like CT scans are crucial to assess the extent of lymph node involvement and fulfill this aspect of the castleman disease diagnosis criteria.
Minor Criteria for iMCD Diagnosis: Supporting Evidence
In addition to the major criteria, the castleman disease diagnosis criteria include a set of minor criteria. For a diagnosis of iMCD, a patient must present with at least two of the eleven minor criteria, with at least one being a laboratory abnormality. These minor criteria further strengthen the diagnostic accuracy and encompass both laboratory findings and clinical manifestations.
Laboratory Minor Criteria: Blood Test Abnormalities
These laboratory abnormalities serve as crucial indicators of the systemic inflammation and dysfunction associated with iMCD. The laboratory minor criteria are:
- Elevated C-reactive protein (CRP) or Erythrocyte Sedimentation Rate (ESR): CRP >10 mg/L or ESR >15 mm/h, indicating systemic inflammation.
- Anemia: Hemoglobin levels below the normal range, reflecting the impact of chronic inflammation on red blood cell production.
- Thrombocytopenia or Thrombocytosis: Platelet counts either abnormally low (<150 k/μL) or high (>400 k/μL), demonstrating dysregulation of platelet production.
- Hypoalbuminemia: Albumin levels below the normal range (<3.5 g/dL), indicative of systemic inflammation and potential liver involvement.
- Renal Dysfunction or Proteinuria: Reduced kidney function (eGFR <60 mL/min/1.73 m²) or protein in the urine (total protein >150 mg/24 h or >10 mg/100 ml), reflecting kidney involvement.
- Polyclonal Hypergammaglobulinemia: Elevated levels of total gamma globulin or immunoglobulin G (>1700 mg/dL), indicating an overproduction of antibodies, a hallmark of iMCD.
Clinical Minor Criteria: Systemic Symptoms and Signs
The clinical minor criteria capture the diverse systemic symptoms and physical signs that patients with iMCD may experience:
- Constitutional Symptoms: Unexplained night sweats, fever (>38°C), unintentional weight loss, or significant fatigue.
- Large Spleen and/or Liver (Hepatosplenomegaly): Enlargement of these organs, detectable through physical examination or imaging.
- Fluid Accumulation: Edema (swelling), anasarca (generalized swelling), ascites (fluid in the abdominal cavity), or pleural effusion (fluid around the lungs).
- Eruptive Cherry Hemangiomatosis or Violaceous Papules: Skin lesions that can be characteristic of iMCD.
- Lymphocytic Interstitial Pneumonitis (LIP): Inflammation of the lung tissue, identified through imaging or biopsy.
Exclusion Criteria for iMCD Diagnosis: Ruling Out Mimicking Conditions
A critical aspect of the castleman disease diagnosis criteria is the exclusion of other diseases that can mimic iMCD. These exclusion criteria are essential to ensure diagnostic specificity and avoid misdiagnosis. It is imperative to rule out the following categories of conditions:
Infection-Related Disorders:
- HHV-8 Associated MCD: Human Herpesvirus-8 (HHV-8) infection is a known cause of multicentric Castleman disease. Excluding HHV-8 infection, typically through negative LANA-1 staining in lymph node tissue, is mandatory for diagnosing iMCD.
- Clinical EBV-Lymphoproliferative Disorders: Conditions like infectious mononucleosis or chronic active Epstein-Barr virus (EBV) infection must be considered and ruled out based on clinical presentation and relevant testing.
- Other Uncontrolled Infections: Inflammation and lymph node enlargement caused by other uncontrolled infections, such as cytomegalovirus (CMV), toxoplasmosis, HIV, or active tuberculosis, must be excluded.
Autoimmune/Autoinflammatory Diseases:
- Systemic Lupus Erythematosus (SLE)
- Rheumatoid Arthritis (RA)
- Adult-Onset Still Disease (AOSD)
- Juvenile Idiopathic Arthritis (JIA)
- Autoimmune Lymphoproliferative Syndrome (ALPS)
These autoimmune conditions can sometimes present with similar clinical and histopathological features to iMCD. Diagnosis requires meeting full clinical criteria for these conditions, not just the presence of autoantibodies alone.
Malignant/Lymphoproliferative Disorders:
- Lymphoma (Hodgkin and Non-Hodgkin)
- Multiple Myeloma
- Primary Lymph Node Plasmacytoma
- Follicular Dendritic Cell (FDC) Sarcoma
- POEMS Syndrome: While POEMS syndrome is related to Castleman disease, it is considered a distinct entity (“POEMS-associated MCD”) due to its association with a monoclonal plasma cell disorder. POEMS syndrome must be excluded to diagnose iMCD.
These malignancies must be diagnosed before or at the same time as iMCD to be considered exclusionary. Malignancies diagnosed more than a year after iMCD diagnosis typically do not negate the iMCD diagnosis. Bone marrow biopsy is often recommended to evaluate for malignancy and POEMS-associated MCD.
Additional Supportive Features: Further Diagnostic Clues
While not part of the major or minor criteria, certain additional features can support an iMCD diagnosis. These include elevated blood levels of Interleukin-6 (IL-6), soluble IL-2 receptor (sIL-2R), Vascular Endothelial Growth Factor (VEGF), IgA, IgE, LDH, and β-2-microglobulin. Reticulin fibrosis in the bone marrow is also a supportive finding, particularly in patients with TAFRO syndrome, a severe subtype of iMCD.
Conclusion: Advancing iMCD Diagnosis and Care
The establishment of these consensus castleman disease diagnosis criteria marks a significant step forward in the field of iMCD. By providing clear and evidence-based guidelines, these criteria will facilitate more consistent and accurate diagnoses, reduce delays in treatment, and promote collaborative research efforts. For clinicians, a thorough evaluation including lymph node biopsy, relevant laboratory tests, and careful exclusion of mimicking conditions is essential when considering iMCD. These criteria promise to improve patient outcomes and deepen our understanding of this rare and challenging disease.
References (References would be listed here if needed, but as per instruction to only include title and content, references are omitted for now).