Understanding Central Fever in Neurocritical Care
Central fever, a non-infectious elevation in body temperature, poses a significant challenge in neurocritical care, particularly following intracranial hemorrhage (ICH) or intraventricular hemorrhage (IVH). Unlike fevers caused by infection, central fever originates from neurological dysfunction, often stemming from damage to the brain’s thermoregulatory centers. This condition is not only prevalent, affecting up to 23% of neurocritical intensive care patients, but also strongly correlated with poorer patient outcomes. Accurate and timely Central Fever Diagnosis is therefore crucial for effective patient management and improved prognosis.
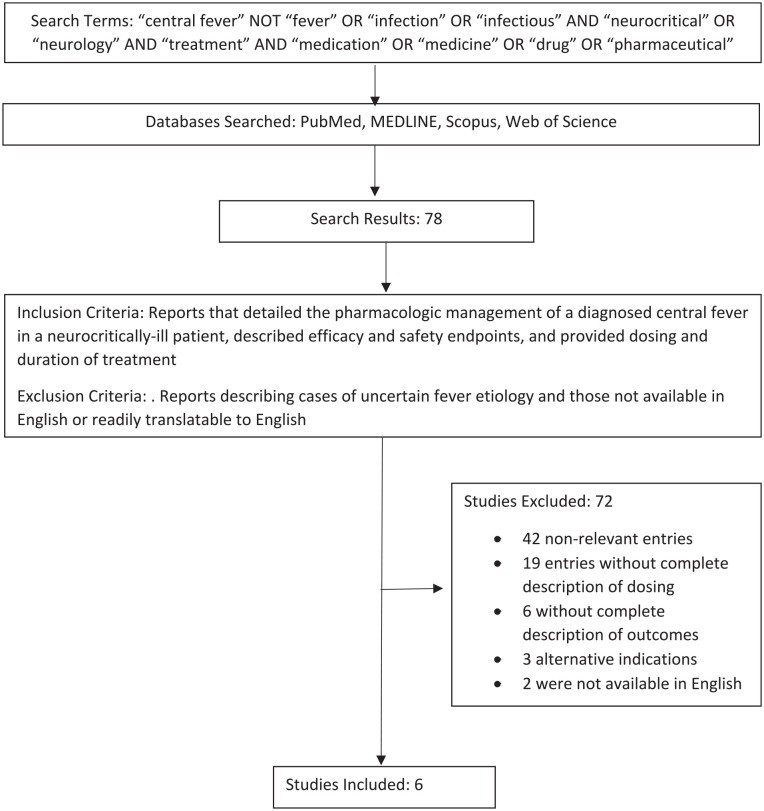 Search Methodology for Central Fever Review
Search Methodology for Central Fever Review
The Link Between Intracranial Hemorrhage and Central Fever
Research has firmly established a link between ICH, IVH, and the development of central fever. A prospective study highlighted a 30% incidence of central fever in patients with ICH. Furthermore, the study identified IVH and the expansion of ICH volume as significant predictors of central fever. Critically, central fever has been directly associated with adverse outcomes. Patients developing central fever after intracranial hemorrhage showed significantly poorer outcomes at 90 days compared to those who remained afebrile. These findings underscore the urgent need for clinicians to prioritize the identification, accurate central fever diagnosis, and effective management of this condition to enhance patient recovery.
Central Fever Diagnosis: A Diagnosis of Exclusion
The diagnosis of central fever is primarily one of exclusion. This means that it is typically diagnosed after ruling out infectious causes of fever. A retrospective study aimed to define diagnostic criteria for central fever in neurocritically ill patients. The research identified independent risk factors including the need for blood transfusion, subarachnoid hemorrhage (SAH), IVH, intracranial tumors, and fever onset within 72 hours of neurocritical intensive care unit admission. When these risk factors are combined with a negative infectious work-up, the probability of central fever is significantly elevated, reaching up to 90%.
Despite these proposed criteria, establishing a definitive central fever diagnosis remains challenging. There is no single, definitive test for central fever. Clinicians must rely on a combination of clinical assessment, patient history, risk factor analysis, and, crucially, the exclusion of infectious etiologies. This process often involves comprehensive infectious disease testing to ensure that the fever is not due to an underlying infection.
Pharmacological Management and Diagnostic Implications
While this article primarily focuses on central fever diagnosis, it’s important to understand that the pharmacological management strategies also play a role in confirming the diagnosis. Currently, the pharmacologic management of central fever, after diagnosis, often involves medications like bromocriptine, propranolol, and baclofen. These medications, while not directly diagnostic tools, are used to manage the condition, and their effectiveness can further support a central fever diagnosis, particularly after infectious causes are ruled out and the fever responds to these specific agents.
Bromocriptine in Central Fever Management
Bromocriptine, a dopamine D2 receptor agonist, is thought to work in central fever by targeting hypothalamic dysfunction. Case reports have shown bromocriptine’s effectiveness in resolving central fever. For instance, a case study involving a patient with a brain tumor and hydrocephalus who developed central fever post-surgery demonstrated fever resolution within 72 hours of bromocriptine initiation. Similarly, another case involving a patient with intraventricular hemorrhage showed fever reduction within 72 hours of bromocriptine treatment. These case reports, while limited, suggest bromocriptine’s potential in managing and, indirectly, confirming central fever diagnosis when other causes are excluded and treatment is effective.
Propranolol in Central Fever Management
Propranolol, a nonselective beta-adrenergic antagonist, is another medication used in central fever management. Its mechanism in central fever is less clear but may involve modulating parasympathetic hyperactivity within the central nervous system. Case series and reports indicate propranolol’s efficacy in reducing central fever in patients with traumatic brain injuries and intracranial hemorrhages. One case series reported fever reduction in patients with traumatic brain injury within 72 hours of propranolol administration. Another case report described a patient with frontal and temporal contusions who achieved normothermia within 48 hours of propranolol initiation. The positive response to propranolol, in the absence of infection, can further support a central fever diagnosis.
Baclofen in Central Fever Management
Baclofen, a GABA-B receptor agonist, is also explored for central fever management. Its proposed mechanism involves regulating brown adipose tissue thermogenesis. Case reports suggest baclofen’s ability to restore normothermia in central fever. A case of central fever following basilar artery occlusion showed temperature normalization after baclofen treatment initiation. Another case involving pontine hemorrhage-induced central fever demonstrated normothermia within 72 hours of baclofen initiation, following dose adjustment. Like bromocriptine and propranolol, baclofen’s effectiveness in reducing fever in these cases, when infections are excluded, strengthens the central fever diagnosis.
Table 1. Central Fever Management Results with Bromocriptine, Propranolol, and Baclofen
| Author | Medication | Report type, number of patients | Precipitating event | Dosing | Time to resolution of fever | Comments |
|---|---|---|---|---|---|---|
| Kang et al | Bromocriptine | Case report N = 1 | Mass in suprasellar region, obstructive hydrocephalus, craniopharyngioma | Initial: 0.05 mg/kg by mouth 3 times daily Maintenance: 0.05 mg/kg by mouth 5 times daily | 72 hours | Fever presented 35 days postoperatively. Bromocriptine ordered for 32 days. Patient weight not specified |
| Yu et al | Bromocriptine | Case report N = 1 | Intraventricular hemorrhage | Initial: 2.5 mg by mouth daily Maintenance: 5 mg by mouth daily | 72 hours | Bromocriptine ordered for 14 days |
| Meythaler et al | Propranolol | Case report N = 1 | Traumatic brain injuries | Initial: 10–20 mg by mouth every 6 hours Maintenance: 30 mg by mouth every 6 hours | 72 hours | Fever returned in one patient when propranolol was held for a procedure. Propranolol continued postdischarge in all patients for 1-2 months, then weaned |
| Garg et al | Propranolol | Case report N = 1 | Frontal and temporal contusions with associated midline shift | Initial: 10 mg by mouth twice daily Maintenance: 10 mg by mouth 3 times per daily | 48 hours | Hypothermia reported. Propranolol continued for 17 days |
| Huang et al | Baclofen | Case report N = 1 | Basilar artery occlusion | Initial:30 mg by mouth daily Maintenance: 30 mg by mouth daily | Unspecified | Duration not reported |
| Lee et al | Baclofen | Case report N = 1 | Pontine hemorrhage | Initial: 30 mg by mouth daily Maintenance:60 mg by mouth daily | 72 hours | Baclofen continued through discharge, duration not reported |
Central Fever Diagnosis and Patient Outcomes
Accurate central fever diagnosis is not only essential for guiding appropriate treatment but also for understanding patient prognosis. As established, central fever is associated with poorer outcomes in neurocritical patients. Therefore, a prompt and accurate diagnosis allows for timely intervention, potentially mitigating the adverse effects of prolonged hyperthermia on neurological recovery. Early central fever diagnosis and management are critical steps in improving overall patient outcomes and reducing morbidity and mortality associated with neurological injuries.
Conclusion: Improving Central Fever Diagnosis in Neurocritical Care
Central fever diagnosis remains a complex clinical challenge, primarily relying on the exclusion of infectious causes and clinical risk assessment. While medications like bromocriptine, propranolol, and baclofen are used for management post-diagnosis, their effectiveness can also indirectly support the diagnosis, especially when infectious etiologies are ruled out and the fever responds to these agents. Given the significant impact of central fever on patient outcomes, continued research is needed to develop more definitive diagnostic tools and refine management strategies. For now, a high index of suspicion in at-risk neurocritical patients, coupled with thorough exclusion of infections, remains the cornerstone of effective central fever diagnosis and subsequent management.
References
References are the same as the original article and are not repeated here to conserve space as per instructions. They are readily available in the original article provided.