Background
The cerebellum, often referred to as the “little brain,” is a vital component of the hindbrain. Despite its smaller size compared to the cerebral cortex, it houses a comparable number of neurons and plays a critical role in motor control, posture, gait, and the coordination of voluntary movements, including eye movements. Located in the posterior fossa, behind the pons and medulla, the cerebellum is connected to the brainstem via three pairs of cerebellar peduncles.
Cerebellar pathologies present a unique spectrum of diagnostic challenges. While some diseases are specific to the cerebellum, others are systemic and affect various brain regions. The increased utilization and enhanced resolution of Magnetic Resonance Imaging (MRI) for infratentorial structures have led to more frequent identification of cerebellar abnormalities. This article aims to provide a comprehensive review of pathological processes affecting the cerebellum, focusing on their distinct imaging features on MRI, essential knowledge for radiologists, neurologists, neurosurgeons, and even automotive repair experts who require a foundational understanding of neurological conditions that can impact vehicle operation and diagnostics. Understanding the Cerebellar Mass Differential Diagnosis is crucial for accurate assessment and appropriate management strategies.
Cerebellar pathologies can be broadly categorized into malformations, vascular events, infections and inflammatory conditions, toxic and metabolic disorders, demyelinating diseases, neurodegenerative conditions, and neoplasms. These categories will be discussed in detail in the following sections, providing a framework for cerebellar mass differential diagnosis.
Cerebellar Malformations
Developmental malformations of the cerebellum are diverse, arising from genetic mutations (e.g., Joubert syndrome), mechanical compression (e.g., Chiari II malformation), or prenatal, perinatal, and postnatal insults. These malformations may occur in isolation or alongside abnormalities in other brain structures like the pons, corpus callosum, and cerebral hemispheres. A thorough understanding of these malformations is essential for the cerebellar mass differential diagnosis, particularly in pediatric cases.
Dandy-Walker Continuum
The Dandy-Walker continuum is a sporadic disorder resulting from hindbrain developmental arrest, often linked to chromosomal abnormalities, single gene disorders, or teratogen exposure. This spectrum of anomalies is characterized by cerebellar vermis hypoplasia and cystic dilatation of the fourth ventricle, readily visualized on MRI. Dandy-Walker malformation, the most severe form, is distinguished from the Dandy-Walker variant (Figure 1) by features such as an enlarged posterior fossa, elevated tentorium and torcula Herophili, and absent vermis (versus hypoplastic vermis in the variant). Cerebellar hemispheres may also be hypoplastic. Obstructive hydrocephalus is a common complication, occurring in approximately 75% of cases due to aqueduct stenosis.
Figure 1.
Figure 1. 5-year-old male with Dandy-Walker variant. Axial T2-weighted (A), T1-weighted (B), and sagittal T2-weighted (C) MR images showing widely separated and hypoplastic cerebellar hemispheres (A, B) and hypoplastic vermis (C). Alt text: MRI scans (axial T2, T1, sagittal T2) of a child’s brain showing Dandy-Walker variant with cerebellar hypoplasia.
Associated conditions include nervous system malformations (neuronal migration anomalies, agenesis of corpus callosum) and extracranial anomalies (cardiac anomalies, skeletal dysplasias). Early diagnosis and management, often involving ventriculoperitoneal or cystoperitoneal shunting, are crucial for improved outcomes.
Key differential diagnoses for Dandy-Walker continuum include mega cisterna magna and arachnoid cysts. Mega cisterna magna is differentiated by a normal cerebellar vermis and hemispheres. Arachnoid cysts can mimic mega cisterna magna radiologically but exert mass effect on the cerebellum and fourth ventricle, sometimes causing scalloping of the occipital bone. Ventriculography or cisternography can help distinguish mega cisterna magna by demonstrating communication with the perimedullary subarachnoid space. Blake’s pouch cyst is another entity in the cerebellar mass differential diagnosis, characterized by ballooning of the superior medullary velum into the cisterna magna but with a normal vermis and cistern.
Cerebellar Hypoplasia
Cerebellar hypoplasia, previously termed Chiari IV malformation (now obsolete), refers to a generalized underdevelopment of the cerebellar hemispheres and vermis without associated cysts or posterior fossa enlargement. It can be unilateral or bilateral. Etiological factors include prenatal exposure to phenytoin, cytomegalovirus infection, ionizing radiation, and genetic defects (trisomies 21, 18, and 13). Patients often present with cognitive impairments affecting memory, behavior, language, social functioning, and autism spectrum disorder. In the cerebellar mass differential diagnosis, cerebellar hypoplasia needs to be considered in cases of global developmental delay and ataxia.
Joubert Syndrome
Joubert syndrome is a rare autosomal recessive disorder characterized by vermian dysplasia and abnormal decussation of fibers in the superior cerebellar peduncles and pyramidal tracts. Clinically, it manifests with neonatal breathing irregularities, developmental delay, hypotonia, ataxia, nystagmus, intellectual disability, and distinctive facial features. The pathognomonic MRI findings include vermian hypoplasia (or agenesis) leading to a ‘batwing’ or triangular fourth ventricle and the ‘molar tooth sign’ (Figure 2). The molar tooth sign is formed by thickened, horizontally oriented superior cerebellar peduncles, a thinned ponto-mesencephalic junction, and a deep interpeduncular fossa. This distinctive sign is crucial for the cerebellar mass differential diagnosis of Joubert syndrome.
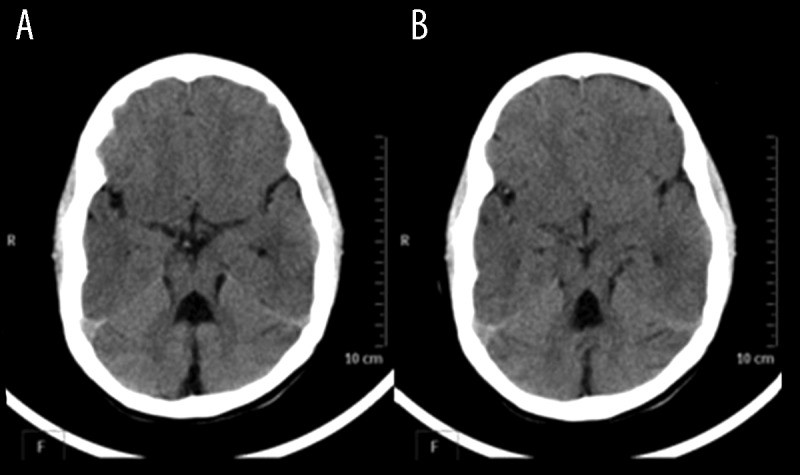
Figure 2.
Figure 2. 6-year-old boy with Joubert syndrome. Axial non-contrast CT images showing dilated batwing-shaped fourth ventricle (A), hypoplastic vermis (A, B), thickened and elongated superior cerebellar peduncles with deep interpeduncular fossa (A, B) creating a molar-tooth appearance. Alt text: Axial CT scans showing molar tooth sign in Joubert syndrome patient with batwing ventricle and vermian hypoplasia.
Associations include brain anomalies (corpus callosum agenesis, gray matter heterotopias, cortical dysplasias, ventriculomegaly) and systemic abnormalities (congenital hepatic fibrosis, multicystic dysplastic kidney, retinal dystrophy, polydactyly).
Rhomboencephalosynapsis
Rhomboencephalosynapsis is a rare congenital cerebellar abnormality characterized by absent or small vermis and fusion of cerebellar hemispheres and peduncles, with or without dentate nuclei fusion. This malformation is part of the cerebellar mass differential diagnosis in congenital ataxia cases.
Other rare syndromes associated with vermian hypoplasia include Oro-facial-digital syndrome type IV, COACH syndrome, and Arima syndrome (cerebro-oculo-hepato-renal syndrome).
Cerebellar Cortical Dysplasia/Heterotopias
Cerebellar cortical dysplasia or heterotopias represent focal areas of disorganized cerebellar hemisphere architecture. While the pathogenesis is not fully understood, associations include chromosomal trisomies, intrauterine infections, and congenital muscular dystrophies. Common sites of involvement are the nodulus, flocculus, and tonsils. MRI features include folial thickening, irregular gray-white interface with abnormal fissures, heterotopias, and cortical cystic lesions (in severe cases) without contrast enhancement. These dysplasias should be considered in the cerebellar mass differential diagnosis when focal cerebellar abnormalities are identified in the context of developmental delays or seizures.
Lhermitte-Duclos Disease
Lhermitte-Duclos disease, also known as dysplastic cerebellar gangliocytoma, clinically presents with macrocephaly and seizures. It results from disrupted laminar cellular organization in the cerebellum, leading to thickened folia. MRI typically reveals non-enhancing focal cerebellar enlargement with prolonged T1 and T2 relaxation times and characteristic curvilinear stripes isointense to cortex (tigroid or striated appearance) (Figure 3). Lhermitte-Duclos disease is an important consideration in the cerebellar mass differential diagnosis of adult cerebellar lesions, especially those with a striated appearance on MRI. It has a known association with visceral hamartomas.
Figure 3.
Figure 3. 40-year-old male with Lhermitte-Duclos disease. Axial T1 (A) and T2-weighted (B) MR images show a well-defined mass in the left cerebellar hemisphere, hypointense on T1 and hyperintense on T2, with isointense and hyperintense striations. Mass effect on the fourth ventricle is evident. Alt text: MRI scans (axial T1, T2) of Lhermitte-Duclos disease with a striated cerebellar mass and ventricular compression.
The diagnostic approach to cerebellar malformations is summarized in Supplement Figure 1.
Chiari Malformations
Chiari malformations are common hindbrain malformations involving caudal displacement of the cerebellum and brainstem. They are crucial to consider in the cerebellar mass differential diagnosis, especially when assessing posterior fossa crowding or spinal cord abnormalities.
Chiari I malformation, the most common type, is characterized by herniation of peg-like cerebellar tonsils more than 5 mm below the foramen magnum. Syringohydromyelia is a frequent association. Patients may be asymptomatic or present in adolescence with ataxia, neck pain, and headaches.
Chiari II malformation involves caudal displacement of the cerebellar vermis, medulla, and fourth ventricle through the foramen magnum, often associated with spina bifida and lumbosacral myelomeningocele (Figure 4). Clinical symptoms vary with age, ranging from myelomeningocele and cranial nerve palsies in neonates to raised intracranial pressure in childhood and scoliosis in adults.
Figure 4.
Figure 4. (A, B) 1.5-year-old male with Chiari II malformation. Sagittal T2-weighted images of the cervicodorsal spine and craniocervical junction showing caudal displacement of the cerebellar vermis and medulla with spina bifida and meningomyelocele in the lower dorsal spine. Syringohydromyelia is also present in the dorsal spinal cord. Alt text: Sagittal MRI of Chiari II malformation showing cerebellar and brainstem displacement with spina bifida and syringomyelia.
Chiari III malformation is rare, combining Chiari II malformation with occipital or high cervical encephalocele. Chiari IV malformation is an obsolete term previously used for severe cerebellar hypoplasia without herniation.
Vascular Pathologies
Vascular pathologies of the cerebellum include infarcts and hemorrhages, both critical components of the cerebellar mass differential diagnosis due to their acute presentation and potential for significant neurological deficits.
Cerebellar Infarcts
Cerebellar infarcts, although less frequent than hemorrhages, account for a small but significant percentage of all strokes. Infarcts can occur in the territories of the superior cerebellar artery (SCA), anterior inferior cerebellar artery (AICA), or posterior inferior cerebellar artery (PICA). Each artery supplies a distinct cerebellar region: SCA – superior cerebellum and vermis; AICA – anteroinferior cerebellum and middle cerebellar peduncle; PICA – posteroinferior cerebellum, vermis, tonsils, and lower medulla. MRI reveals a wedge-shaped area of altered signal intensity (hypointense on T1, hyperintense on T2 and FLAIR) corresponding to the affected arterial territory, often with mass effect and diffusion restriction (Figure 5). Accurate and timely diagnosis of cerebellar infarcts is crucial due to the high mortality rate (20–50%) and potential for fatal complications like brainstem compression and obstructive hydrocephalus. Infarcts are a critical consideration in the cerebellar mass differential diagnosis in patients presenting with acute onset ataxia and vertigo.
Figure 5.
Figure 5. 60-year-old male with bilateral PICA infarcts. Axial FLAIR (A) shows hyperintensity in bilateral posterior inferior cerebellar hemispheres (PICA territory) with acute diffusion restriction on DWI (B). Alt text: MRI FLAIR and DWI images showing bilateral PICA infarcts with diffusion restriction.
Cerebellar Hemorrhage
Cerebellar hemorrhages constitute about 10% of all brain hemorrhages. Uncontrolled hypertension is the most common cause, followed by vascular malformations and neoplastic bleeds. MRI signal characteristics vary with the age of the hemorrhage. Timely management, including evacuation and hydrocephalus control, is essential, especially for hemorrhages larger than 3 cm or with brainstem compression. Prognosis is generally favorable with prompt intervention. Remote cerebellar hemorrhage, a rare entity following supratentorial craniotomy, has a self-limiting course. Risk factors include male sex, perioperative hypertension, CSF loss, and preoperative anticoagulation. Hemorrhage is a key component of the cerebellar mass differential diagnosis in acute neurological presentations, requiring rapid differentiation from infarcts and tumors.
Infective and Inflammatory Conditions
Infective and inflammatory conditions, while less common than other cerebellar pathologies, are important to consider in the cerebellar mass differential diagnosis, especially in patients presenting with acute ataxia and systemic inflammatory signs.
Acute Cerebellitis
Acute cerebellitis (acute cerebellar ataxia) is a rare inflammatory disorder characterized by isolated cerebellar inflammation. It can be infectious, post-infectious, or post-vaccination, often triggered by viral agents like Varicella zoster, Epstein-Barr virus, measles, mumps, rubella, herpes simplex, and coxsackie viruses. More common in children, it presents with acute onset ataxia, nystagmus, and dysarthria. Neuroimaging is often initially normal, with recovery typically occurring over weeks. Severe cases may show features of raised intracranial pressure, hydrocephalus, and brain herniation, with corresponding MRI findings. Common MRI findings include diffuse swelling of bilateral cerebellar hemispheres (gray and white matter), T2 hyperintensities, mild diffusion restriction, and contrast enhancement in the cerebellar cortex and leptomeninges (Figure 6). Unilateral involvement and vermis/peduncle involvement are variable.
Figure 6.
Figure 6. 20-year-old male with scrub typhus cerebellitis. Axial FLAIR (A) shows diffuse hyperintensities in both cerebellar hemispheres with fourth ventricle compression and hydrocephalus. Parasagittal T2 (B) shows gray matter hyperintensities and tonsillar herniation. Axial contrast-enhanced T1 (C) shows leptomeningeal enhancement. Axial DWI (D) shows restricted diffusion. Alt text: MRI FLAIR, T2, contrast T1, and DWI of cerebellitis showing diffuse cerebellar inflammation and leptomeningeal enhancement.
Parenchymal granulomas, such as tuberculomas and neurocysticercosis, can also occur in the cerebellum, similar to other brain regions, and must be considered in the cerebellar mass differential diagnosis in endemic regions.
Toxic/Metabolic Disorders
Toxic and metabolic disorders represent a broad category in the cerebellar mass differential diagnosis, with diverse presentations ranging from cerebellar atrophy to specific patterns of involvement. Cerebellar abnormalities due to inborn errors of metabolism can be categorized into cerebellar hypoplasia, cerebellar atrophy, white matter abnormalities, and involvement of dentate nuclei and cerebellar cortex.
Cerebellar atrophy is differentiated from hypoplasia by the presence of enlarged fissures due to tissue loss, although differentiation can be challenging, and atrophy can overlay hypoplasia. Atrophy can result from toxins like alcohol (alcoholic cerebellar degeneration), drugs like phenytoin, and genetic neurodegenerative disorders.
Symmetric dentate nuclei involvement is seen in metabolic disorders like Leigh disease, maple syrup urine disease (also affecting cerebellar white matter), Wernicke encephalopathy, and toxins like metronidazole (Figure 7), methyl bromide, and organic solvents. MRI shows T2/FLAIR hyperintensity with or without diffusion restriction. Cerebellar cortex involvement is characteristic of infantile neuroaxonal dystrophy.
Figure 7.
Figure 7. 40-year-old male with metronidazole toxicity. Axial FLAIR (A) and coronal T2 (B) show symmetric hyperintensities in bilateral cerebellar dentate nuclei. Axial DWI (C) shows mild diffusion restriction. Alt text: MRI FLAIR, coronal T2, and DWI of metronidazole toxicity showing dentate nuclei involvement.
Genetic Neurodegenerative Disorders
Genetic neurodegenerative disorders are a complex group of chronic conditions characterized by progressive ataxia and dysarthria. Familiarity with these entities and their imaging features is crucial for the cerebellar mass differential diagnosis of ataxias of uncertain etiology.
Ataxia-Telangiectasia
Ataxia-telangiectasia is a rare autosomal recessive neurocutaneous disorder characterized by progressive cerebellar ataxia, oculomucocutaneous telangiectasias, and predisposition to infections and malignancies. Resulting from a defective gene on chromosome 11q22-23, MRI shows marked cerebellar atrophy (vermis and hemispheres). T2 gradient echo images may reveal low signal intensity foci representing capillary telangiectasias. Hemorrhages can occur due to vessel rupture. MR spectroscopy may show increased choline in the cerebellum, aiding differentiation from other ataxias.
Friedreich Ataxia
Friedreich ataxia, the most common inherited progressive ataxia (autosomal recessive), results from GAA trinucleotide repeat expansion on chromosome 9q. Pathologically, it involves loss of myelinated fibers and gliosis in the posterior and lateral columns of the cervical spinal cord. MRI shows cervical spinal cord thinning and signal changes. Cerebellar atrophy, particularly peridentate cerebellum and superior cerebellar peduncles, correlates with neurological deficits. Atrophy of the medulla, midbrain, pons, and optic chiasm is also observed. Friedreich ataxia is a key consideration in the cerebellar mass differential diagnosis of progressive ataxia, particularly with spinal cord involvement.
Olivopontocerebellar Atrophy
Olivopontocerebellar atrophy (multiple system atrophy-cerebellar type) is a neurodegenerative disorder caused by alpha-synuclein metabolism abnormalities and intracellular deposition in neurons and oligodendroglia. Presenting with ataxia and bulbar dysfunction, MRI shows gross atrophy and T2 hyperintensities in the pons, middle cerebellar peduncles, and cerebellum. The ‘hot cross bun sign’ in the pons (cruciate T2 hyperintensity due to pontocerebellar tract involvement) is characteristic (Figure 8). Olivopontocerebellar atrophy is an important differential in the cerebellar mass differential diagnosis of adult-onset ataxia with prominent pontocerebellar involvement.
Figure 8.
Figure 8. 40-year-old female with olivopontocerebellar atrophy. Axial T2 (A) shows diffuse cerebellar and pontine atrophy with the hot cross bun sign in the pons. Axial FLAIR (B) shows hyperintensity in middle cerebellar peduncles and pontocerebellar atrophy. Alt text: MRI T2 and FLAIR of olivopontocerebellar atrophy showing cerebellar and pontine atrophy with hot cross bun sign.
Fahr Disease
Fahr disease is a rare familial neurodegenerative disorder characterized by abnormal cell loss and calcium deposition in the basal ganglia (globus pallidus), internal capsule, dentate nucleus, thalamus, and cerebellar and cerebral white matter. Etiology remains unclear. Fahr disease, while primarily affecting basal ganglia, should be considered in the cerebellar mass differential diagnosis when calcifications are noted in the dentate nuclei and cerebellum alongside basal ganglia.
Fragile X-Associated Ataxia/Tremor Syndrome (FXTAS)
Fragile X-associated ataxia/tremor syndrome (FXTAS) is an X-linked dominant neuropsychiatric degenerative disorder and the most common cause of inherited mental retardation. Clinical features include cognitive impairment, behavioral problems, ataxia, tremors, and rigidity. MRI findings include symmetric T2 hyperintensities in middle cerebellar peduncles (MCP sign – characteristic) and cerebellar/cerebral white matter, along with pontine, cerebellar, and cerebral atrophy. The MCP sign is particularly relevant in the cerebellar mass differential diagnosis of adult-onset ataxia with white matter abnormalities.
Demyelinating Disorders
Demyelinating disorders, including multiple sclerosis (MS), acute disseminated encephalomyelitis (ADEM), and progressive multifocal leukoencephalopathy (PML), can involve the cerebellum. Imaging findings range from small punctate lesions to large tumefactive lesions with relatively less mass effect than their size. Enhancement is variable, ranging from non-enhancing to open-ring enhancement, a characteristic pattern. While demyelinating lesions are not typically considered ‘masses,’ they enter the cerebellar mass differential diagnosis when presenting as larger, atypical lesions mimicking tumors.
Neoplasms
Neoplasms are a critical category in the cerebellar mass differential diagnosis, ranging from benign to highly malignant, and varying significantly between pediatric and adult populations.
Childhood Tumors
The most common cerebellar neoplasm in children is pilocytic astrocytoma, followed by medulloblastoma. Less common tumors include atypical teratoid/rhabdoid tumor (ATRT), teratoma (in infants), and hemangioblastoma (in Von Hippel-Lindau syndrome [VHL]).
Juvenile Pilocytic Astrocytoma
Juvenile pilocytic astrocytomas (JPAs) are WHO grade 1 tumors, typically occurring in the first two decades of life. Predominantly cerebellar (85% of cerebellar astrocytomas), they often involve both vermis and hemisphere. Imaging typically shows a large cystic lesion with an intensely enhancing mural nodule (Figure 9). The cyst wall may or may not enhance. Solid components are T1 hypointense and T2 hyperintense. Vasogenic edema is rare. Neurofibromatosis type 1 is a common association. Histopathology reveals pathognomonic eosinophilic Rosenthal fibers. Prognosis is excellent with complete surgical resection, and recurrence/dissemination is uncommon. Pilocytic astrocytoma is a primary consideration in the cerebellar mass differential diagnosis of cystic cerebellar lesions in children.
Figure 9.
Figure 9. 9-year-old boy with pilocytic astrocytoma. Axial T2 (A) and post-contrast T1 (B) show a large, well-defined cystic lesion with a mildly hyperintense mural nodule in the left cerebellar hemisphere and vermis, with thick, irregular enhancement of the cyst wall and mural nodule. Alt text: MRI T2 and contrast T1 of pilocytic astrocytoma showing cystic cerebellar mass with enhancing mural nodule.
Medulloblastoma
Medulloblastomas are WHO grade 4, highly cellular, small round blue cell tumors, also known as CNS primitive neuroectodermal tumors (PNETs). Median age of occurrence is 9 years, more common in males (M:F 2-4:1). Most commonly cerebellar vermis (three-fourths). Obstructive hydrocephalus is common due to fourth ventricle protrusion. Brainstem involvement can occur. Hyperdense on CT, isointense on T1, T2, with diffusion restriction on DWI. Cyst formation/necrosis (40-50%) and calcification (10-20%) are common. Contrast-enhanced MRI of the entire neuraxis is crucial to screen for CSF seeding and leptomeningeal spread, common in these patients (Figure 10). Medulloblastoma is a critical consideration in the cerebellar mass differential diagnosis of solid, enhancing cerebellar masses in children, especially those with hydrocephalus and potential CSF dissemination.
Figure 10.
Figure 10. 7-year-old boy with medulloblastoma. Axial T1 (A) and coronal T2 (B) show a well-defined homogeneous vermian mass, hypointense on T1 and mildly hyperintense on T2, with fourth ventricle mass effect and hydrocephalus. Axial DWI (C) shows diffusion restriction. Axial post-contrast T1 (D) shows moderate enhancement with peripheral necrosis. Sagittal post-contrast T1 (E) of the dorsolumbar spine shows diffuse leptomeningeal spread. Alt text: MRI T1, T2, DWI, and contrast T1 of medulloblastoma showing vermian mass, enhancement, diffusion restriction, and spinal leptomeningeal spread.
Atypical Teratoid/Rhabdoid Tumor (ATRT)
Atypical teratoid/rhabdoid tumors (ATRTs) are uncommon, highly aggressive WHO grade 4 tumors, mostly cerebellar in children under 2 years. Histologically distinguished by sheets of rhabdoid cells. MRI shows iso- to slightly hyperintense T1 and hyperintense T2 lesions with necrosis, cysts, calcification, hemorrhage, and heterogeneous enhancement. Leptomeningeal spread is common, worsening prognosis. ATRT is a crucial differential in the cerebellar mass differential diagnosis of aggressive cerebellar tumors in very young children.
Tumors in Adults
Metastases are the most common cerebellar neoplasms in adults, with lung and breast cancer being the most frequent primaries. Less common primaries include melanoma, thyroid cancer, and renal cell carcinoma. Metastases are sharply demarcated lesions with disproportionate peritumoral edema. Approximately 50% are multiple, and hemorrhage is possible. Typically isointense on T1 and hyperintense on T2/FLAIR, though hemorrhage can alter signal. MR spectroscopy shows depleted NAA and elevated choline, unlike primary tumors (e.g., glioblastoma) where NAA is less profoundly decreased. Metastases are a primary consideration in the cerebellar mass differential diagnosis of adult cerebellar masses, especially in patients with known primary malignancies.
Hemangioblastoma
Hemangioblastomas are WHO grade 1 vascular tumors occurring in the CNS and extraneural sites (kidneys, liver, pancreas). Sporadic cases (75-80%) peak at 30-60 years. VHL-associated cases occur earlier and are often multiple. 5-40% of patients have polycythemia due to erythropoietin production. Most common location is cerebellar hemisphere (85%), then vermis (10%). MRI shows well-defined cystic lesions (non-enhancing wall) with vividly enhancing mural nodule (60%). Mural nodule is T1 hypointense, T2 hyperintense, with flow voids. Solid tumors (40%) occur with or without cysts. Preoperative embolization may be used for large lesions. Surgery is usually curative. Hemangioblastoma is an important consideration in the cerebellar mass differential diagnosis of cystic cerebellar lesions in adults, particularly in the context of VHL syndrome.
Rarely, medulloblastomas and astrocytomas occur in adults (<1% of tumors).
Conclusions
The cerebellum is a critical brain structure, and its dysfunction can manifest in a wide range of motor and non-motor deficits. Cerebellar pathologies can have significant mass effect, potentially causing life-threatening brainstem and fourth ventricle compression. Therefore, awareness of the imaging features of cerebellar abnormalities is essential for prompt and accurate diagnosis. This comprehensive overview of cerebellar mass differential diagnosis, focusing on MRI characteristics, provides a valuable resource for clinicians and specialists involved in neurological assessment and management, as well as for automotive repair experts who benefit from a broader understanding of neurological conditions.
Supplement Figure 1. Approach to diagnose cerebellar malformations.
References
[List of references from original article]
Associated Data
Supplementary Materials
Supplement Figure 1. Approach to diagnose cerebellar malformations.