 Child undergoing physiotherapy for cerebral palsy
Child undergoing physiotherapy for cerebral palsy
Cerebral palsy (CP) stands as a prevalent group of neurological disorders impacting children, characterized by permanent conditions affecting movement and posture. This encompasses a spectrum of symptoms that can significantly impair mobility, motor skills, vision, speech, muscle tone, and overall physical function. These motor disorders are frequently accompanied by disturbances in sensation, cognition, communication, and behavior, presenting considerable challenges in diagnosis and long-term care.
Globally, cerebral palsy affects millions, with significant statistics highlighting its prevalence and impact:
- In the United States, the prevalence is approximately 1 in every 345 children.
- Diagnosis is often delayed, typically occurring between the ages of 2 and 3 years.
- Boys are diagnosed more frequently than girls.
- African American children have a higher incidence rate compared to white children.
- Premature infants and children with low birth weight are at an elevated risk of developing cerebral palsy.
The etiology of cerebral palsy is multifaceted, ranging from genetic mutations and prenatal events to birth injuries during labor and delivery, and asphyxia. Postnatal factors such as brain damage, trauma, injury, and infections like meningitis can also lead to the development of cerebral palsy.
Understanding the complexities of cerebral palsy diagnosis, classification, and care is paramount for healthcare professionals. A recent continuing medical education session emphasized the critical knowledge needed by pediatric primary care providers in managing children with cerebral palsy. Dr. Catherine P. Schuster, a specialist in pediatric physical medicine and rehabilitation at Norton Children’s Physical Medicine & Rehabilitation, and affiliated with the UofL School of Medicine, led this session. Her expertise focused on the classification systems used in cerebral palsy, current diagnostic approaches, and effective rehabilitation strategies. Dr. Schuster highlighted the importance of tailoring treatment plans to the severity of the condition, the underlying pathology, and the child’s anticipated functional abilities. Furthermore, she addressed the impact of involvement in other bodily systems and the necessity for adaptable treatment strategies as symptoms evolve and the patient matures.
The Indispensable Role of Accurate Cerebral Palsy Diagnosis
Achieving an early and precise diagnosis of cerebral palsy is not merely a formality; it is a cornerstone for improving outcomes for affected children and their families. Dr. Schuster underscored several key benefits of accurate and timely diagnosis:
- Establishing Realistic Expectations: A definitive diagnosis provides the family and the multidisciplinary medical team with a clearer understanding of the child’s developmental trajectory and the potential progression of the condition. This foresight allows for proactive planning and management.
- Enabling Early Intervention for Enhanced Outcomes: Early intervention programs are crucial in maximizing a child’s functional abilities and minimizing the long-term impact of cerebral palsy. Prompt diagnosis facilitates immediate access to these vital services, leading to better developmental outcomes.
- Preventing Unnecessary and Invasive Investigations: Accurate diagnosis can eliminate the need for extensive and often stressful diagnostic procedures aimed at identifying the cause of motor impairments when cerebral palsy is clearly indicated.
- Facilitating Access to Timely Support and Resources: A diagnosis of cerebral palsy opens doors to a network of support systems and resources, including financial aid, specialized therapies, and community support groups, all essential for families navigating the complexities of care.
- Informing Future Family Planning Decisions: For families considering expanding their family, understanding the diagnosis and potential genetic or environmental factors associated with cerebral palsy can be crucial for informed decision-making in family planning.
Differentiating Cerebral Palsy from Mimicking Conditions
The diagnostic journey for cerebral palsy is not always straightforward. Several conditions can present with symptoms that closely resemble cerebral palsy, often referred to as “cerebral palsy mimickers”.
Dr. Schuster clarified, “A mimicker is a condition that exhibits some cerebral palsy-like symptoms, such as spasticity, ataxia, or dyskinesia, but lacks the typical risk factors or neuroimaging findings associated with brain injury or congenital malformation.” She further noted that neuroimaging, a key diagnostic tool, can sometimes be normal in up to 15% of children ultimately diagnosed with cerebral palsy. This diagnostic ambiguity underscores the need for a comprehensive approach.
To enhance diagnostic accuracy and differentiate cerebral palsy from mimickers, Dr. Schuster recommends utilizing a combination of advanced tools in conjunction with clinical expertise and judgment:
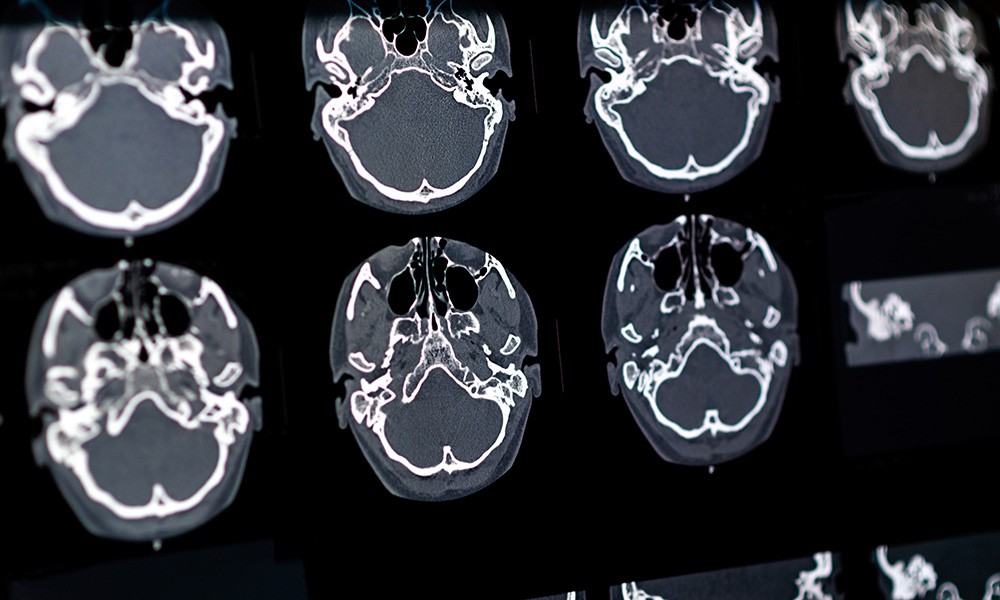
- Magnetic Resonance Imaging (MRI): MRI is crucial for visualizing brain structures and identifying lesions or abnormalities indicative of cerebral palsy. It helps rule out other neurological conditions and provides insights into the nature and extent of brain damage.
- Prechtl’s Assessment of General Movements: This qualitative assessment method evaluates spontaneous movements in infants, proving highly effective in early detection of neurological impairments and predicting cerebral palsy risk, even before traditional symptoms are fully evident.
- Hammersmith Infant Neurological Examination (HINE): HINE is a standardized neurological examination specifically designed for infants. It assesses various aspects of neurological function, aiding in the early identification of neurological abnormalities consistent with cerebral palsy.
Cerebral Palsy Classification: A Framework for Understanding
Once a definitive diagnosis of cerebral palsy is established and mimicking conditions are excluded, the next critical step is classification. “Classification is essential for understanding the specific challenges a child faces and tailoring appropriate interventions,” explained Dr. Schuster. The classification of cerebral palsy is based on three primary aspects:
-
Type of Movement Disorder: Cerebral palsy is categorized into three main types based on the predominant movement disorder observed:
- Spastic Cerebral Palsy: This is the most common type, characterized by increased muscle tone (hypertonia) and stiff or rigid muscles. Spasticity can affect different parts of the body, leading to difficulties with voluntary movement.
- Dyskinetic Cerebral Palsy (including Dystonic and Athetoid): This type involves involuntary movements. Dystonia is characterized by sustained or intermittent muscle contractions causing twisting and repetitive movements or abnormal postures. Athetosis involves slow, writhing, involuntary movements, particularly in the hands, feet, arms, and legs.
- Ataxic Cerebral Palsy: Ataxia primarily affects balance and coordination. Individuals with ataxic CP may have difficulties with depth perception, fine motor tasks, and maintaining balance and a steady gait.
-
Anatomical Distribution: This refers to the parts of the body affected by motor impairments. Common classifications include:
- Monoplegia: Affecting one limb.
- Diplegia: Primarily affecting the legs, with lesser involvement of the arms.
- Hemiplegia: Affecting one side of the body (arm and leg on the same side).
- Quadriplegia: Affecting all four limbs, often with involvement of the trunk and facial muscles.
-
Function: Classification also considers how the movement disorder impacts a child’s functional abilities and overall quality of life. The Gross Motor Function Classification System (GMFCS) is a widely used five-level system that describes gross motor function in children with cerebral palsy, ranging from level I (walking without limitations) to level V (severely limited mobility).
Dr. Schuster emphasized that “understanding the classification allows families and healthcare providers to anticipate the child’s prognosis and plan for appropriate support and interventions to optimize their quality of life.”
Prognosis Based on Cerebral Palsy Classification
One of the most pressing questions families have after a cerebral palsy diagnosis is regarding their child’s future mobility, particularly walking. “Predicting ambulation is a key concern for families,” Dr. Schuster acknowledged. Prognosis for walking is assessed based on several factors, including:
- Presence or Absence of Primitive Reflexes: The persistence of primitive reflexes beyond their typical developmental window can indicate neurological delays and impact motor development.
- Gross Motor Skill Development: Monitoring the progression of gross motor milestones, such as sitting, crawling, and pulling to stand, provides valuable insights into a child’s motor capabilities and potential for ambulation.
- Type of Cerebral Palsy: The classification of cerebral palsy itself is a significant prognostic indicator. For instance, children with milder forms of spastic diplegia often have a higher likelihood of walking compared to those with quadriplegia or more severe dyskinetic forms.
Discussions about prognosis should be ongoing and nuanced, occurring over multiple consultations. Healthcare providers should provide realistic expectations regarding the level of physical assistance a child may require for walking and other activities, ensuring families are well-informed and prepared.
Associated Disorders and Comprehensive Management
Cerebral palsy is not solely a motor disorder; it can affect multiple body systems. The likelihood of involvement in other systems increases with the severity of brain damage.
Dr. Schuster highlighted the high prevalence of visual impairments, stating they “can occur in up to 100% of children with cerebral palsy, ranging from common conditions like amblyopia to severe cortical visual impairment.”
Beyond visual issues, other associated disorders are common:
- Hearing Impairments: Hearing loss can affect communication and development, necessitating early screening and intervention.
- Cognitive Impairments: Intellectual disability and executive function deficits are frequently observed, requiring tailored educational and therapeutic strategies.
- Seizures and Epilepsy: Epilepsy is a common comorbidity, often requiring long-term management with anticonvulsant medications.
- Nutritional Deficiencies and Low Bone Mineral Density: Feeding difficulties and reduced mobility can lead to nutritional deficits and decreased bone density, requiring proactive nutritional support and monitoring.
Navigating the Challenges of Cerebral Palsy Care and Treatment Strategies
The overarching goal of physical medicine and rehabilitation in cerebral palsy is to maximize mobility, functional abilities, and ultimately, improve the quality of life for individuals with CP. A multidisciplinary approach is crucial, involving a range of specialized interventions and treatments, including:
- Physical Therapy: To improve gross motor skills, strength, balance, and mobility through exercises, stretches, and gait training.
- Occupational Therapy: To enhance fine motor skills, daily living skills, and adaptive strategies for performing everyday tasks.
- Speech Therapy: To address communication difficulties, speech impediments, and swallowing problems.
- Assistive Devices: Including braces, orthotics, wheelchairs (manual or powered), and adaptive equipment to support mobility, posture, and independence.
- Recreation Therapy: Utilizing recreational activities to improve physical, emotional, and cognitive well-being.
- Surgery: Orthopedic surgeries may be considered to correct deformities, improve joint alignment, and reduce spasticity in some cases.
- Medication: Pharmacological interventions play a role in managing specific symptoms, particularly spasticity.
When considering treatment options, especially for managing spasticity, Dr. Schuster emphasized the importance of individualizing care. “The family’s goals, available resources, and lifestyle are critical factors in determining the most appropriate interventions,” she stated.
Medication Interventions for Spasticity Management
The effectiveness of medication in cerebral palsy varies depending on the type of CP and individual patient factors. For spasticity, common medication interventions include:
- Benzodiazepines: Frequently used for spasticity, especially in younger children with severe symptoms. However, they come with challenges related to dosing, delivery methods, and potential sedative side effects.
- Baclofen: A common antispasticity medication available in pill form, although a suspension formulation is available but less accessible.
- Dantrolene: A peripherally acting antispasticity medication that minimizes sedative side effects but requires liver function monitoring and can be challenging to dose accurately in liquid form.
- Tizanidine and Clonidine: Alpha agonists that can contribute to spasticity control.
Chemodenervation, using injections like botulinum toxins (FDA-approved for spasticity management), offers targeted relief for specific muscle groups. Alcohol blocks, using diluted alcohol injections, can also be employed to weaken muscle contractions by denaturing motor nerve points.
Addressing the Lifelong Journey: Aging with Cerebral Palsy
Cerebral palsy is a lifelong condition. Pediatric patients transition into adulthood, bringing new challenges and healthcare needs. “Adults with cerebral palsy face not only the typical health concerns of aging but also disorder-specific issues,” Dr. Schuster noted.
Key considerations for adults with cerebral palsy include:
- Routine Health Screenings: Adults with CP require standard health screenings like colonoscopies, alongside specialized services.
- Pain Management: Chronic pain is a significant concern, requiring comprehensive pain management strategies.
- Adaptive Equipment and Physical Assistance: Ongoing needs for adaptive equipment, mobility aids, and physical assistance are common.
- Potential Decline in Mobility: Studies indicate that mobility can decline in at least 25% of adults with cerebral palsy, necessitating proactive management and support.
With approximately 400,000 adults living with cerebral palsy in the U.S., understanding and addressing their long-term needs is crucial. While the overall survival rate at 30 years is around 87%, factors like intellectual disability or epilepsy can negatively impact survival.
In conclusion, cerebral palsy is a complex condition stemming from brain injury occurring in early life. Accurate classification based on movement disorder type, anatomical distribution, and function is essential for guiding prognosis and treatment. Effective management necessitates a multidisciplinary healthcare team and, crucially, incorporates the family’s perspectives and goals to navigate the ongoing challenges of care and optimize the individual’s quality of life throughout their lifespan.